Tooth extraction, healing implantation (part one)
Today we will look at the processes that occur after the tooth is removed. That is, how the bone heals and when it is better to install implants. Let's analyze the most frequent questions that dentists have, as well as the advantages and disadvantages of different periods of implant installation.
Basics of alveolar bone anatomy
At the very beginning, it is worth agreeing the terminology because, unfortunately, even in serious publications you can find wording like: “the alveolar process of the lower jaw”. This is incorrect. On the lower jaw, the alveolar part is isolated, as well as on the upper jaw. The term “alveolar ridge” can only be used if the tooth has been extracted and the alveolar bone has completely healed. That’s right, and in the future we will adhere to this terminology.
In the lower jaw, specialists distinguish the alveolar part and the basal part, see the illustration below.
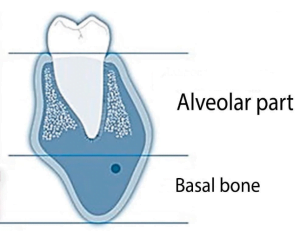
It should be understood that the boundary between the basal bone and the alveolar part is contingent and rather imaginary.
The alveolar part, in turn, is divided into:
- Lamellar alveolar bone is a dense plate lining the inner space of the hole (alveoli). In radiology, it is called the internal cortical plate (Lamina Dura). There is also a histological term – bundle bone (Bundle bone). In all cases, we are talking about the same anatomical structure, see the illustration below. It is tightly connected with the tooth, literally permeated with sharpei fibers, and receives nutrition from the periodontal ligament.
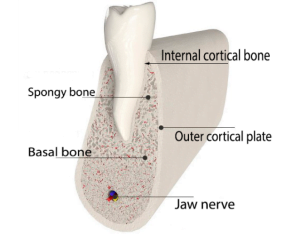
- The supporting alveolar bone is the outer cortical plate and cancellous bone underneath that fills the space between the inner and outer cortical plates.
When a tooth is removed, resorption of the lamellar alveolar bone inevitably occurs. The socket fills with cancellous bone, and the cortical plate grows and hardens from above – this is a normal healing process, and in most cases we do not directly observe the fascicular bone.
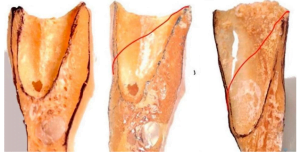
However, the situation may get complicated. It is not for nothing that we devote so much time to the structure of the alveolar bone. Because if on the vestibular side the total thickness of the inner and outer cortical plates is less than 1.8 mm, then the probability of bone resorption is high (more than 60%). One of the options for this phenomenon is shown in the photo below. There is still a completely living tooth with a virtually bare root. Implantation in such cases is quite difficult and there is a possibility that the abutment will be visible over the gums.

The following image shows several variants of the alveolar bone thinned to the outside.
This is extremely important, especially in cases of immediate implantation, because a root implant needs a sufficiently wide and massive bone in which it will be held.
There is an interesting study from 2013 examining the relationship between bone loss and the initial thickness of the bundle bone.
The studies were performed using high-precision tomography on the most problematic areas – the frontal teeth of the upper jaw. The results showed that if the thickness of the vestibular bone plate ≤ 1 mm, then in almost 70% of cases there is a significant resorption, an average of 7.5 mm. This is up to 2/3 of the tooth root. The results of such resorption can be clearly seen in the image below. Here we see a deep sag in the alveolar bone in the place of the extracted tooth.
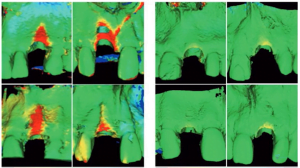
Conversely, if the thickness of the vestibular plate is greater than 1 mm, then the resorption of the alveolar part on average does not exceed 1.1 mm.
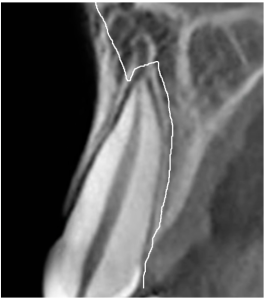
The following image illustrates well what will happen in the event of tooth loss. The image shows that the front side of the bundle bone is very thin.

In the case of tooth loss, the bundle bone will be completely dissolved. The following image shows a line of possible bone loss.
To summarize the intermediate results, we have discovered that:
- the alveolar bone conventionally consists of two sections:- the bundle bone is the dense bone plate that lines the inner surface of the hole;
– the supporting structure is the outer cortical plate and some amount of cancellous bone. - In some cases, the outer side of the alveolar bone is so thin that essentially the “bare” bundle bone remains.
- When a tooth is lost, the bundle bone inevitably dissolves. If everything happens in the area of molars, where there is a large enough mass of bone, the hole heals without loss. However, in the area of the anterior teeth, the bundle bone can be almost the only thing that holds the root of the tooth on the vestibular side, and with it a significant portion of the alveolar bone will dissolve. This means that alveolar ridge augmentation (bone augmentation) is likely to be necessary.
This is important to understand and taken into account when making a treatment plan.
How is the healing of the hole?
Let’s take a closer look at the variety of processes that occur after a tooth extraction. The practitioner needs to remember the main healing trigger points that are important for implant planning.
First we will take the study of Dr. Cardaropoli from 2003. The study was performed (in vivo) on dogs to find out on the histological level what happens in the extraction site after a tooth extraction.
- Day One:
– the well is lined with bundle bone because it has not yet had time to dissolve;
– the well is filled with a blood clot, which contains: fibrin; red blood cells, inflammatory cells, which appear after a couple of hours.
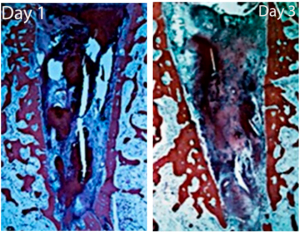
In addition, there is a lot of tissue detritus in the hole: fragments and debris. Macrophages should therefore clear the hole of all of this in the first place. - By the third day, the situation is already changing noticeably. New structures appear. The fibrin network, which heals the vessels and consists of:
– some number of erythrocytes and platelets;
– inflammatory cells (neutrophils, etc.).Close to the bundle bone you can already see:
– mesenchymal cells ready to turn into connective tissue; ruptured periodontal fibers; dilated vessels.Most importantly, in the center of the blood clot the blood cells begin to be replaced by a well vascularized granulation tissue, and an inflammatory infiltrate. From that moment on, it is the granulation tissue that will replace the entire content of the blood clot. - Interesting changes occur by the 7th day. In the picture we can see that the entire well is partially filled with granulation tissue rich in blood vessels. Part of the granulation tissue is already turning into an osteoid. It is also called the fibrin matrix. Mesenchymal cells and leukocytes are also observed. There is also the action of osteoclasts, which begin to resorb the bundle bone.
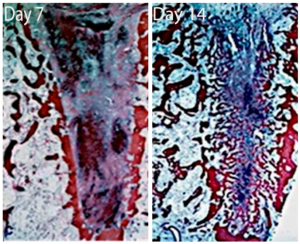
- By the 14th day, the situation changes dramatically. There is still an osteoid in the center, which turns into a coarse-fiber bone. At the same time, most of the bundle bone is resorbed. The medullary space in the interdental septa is directly fused with the newly formed bone, because the remnants of the bundle bone practically do not interfere with this.
- By the 30th day, most of the hole is filled with newly formed bone. A large number of primary osteons are observed. They are formed around the already formed vessels. The process of bone modeling and remodeling has also started.
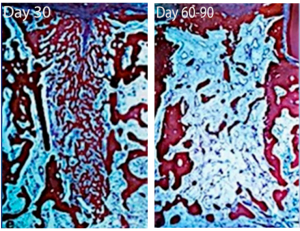
- Days 60-90th: A significant part of the coarse fiber bone has been replaced by spongy bone. The bone marrow spaces are filled with:
– large blood vessels;
– while there are some inflammatory cells;
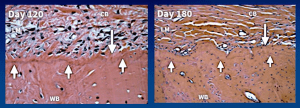
– adipocytes.The process of forming a bone “lid” above the hole has begun – this is a hard and dense cortical bone. This process is also called corticalization. - The entrance to the well is closed by a powerful layer of cortical bone after 4 months (120 days), see the illustration below.
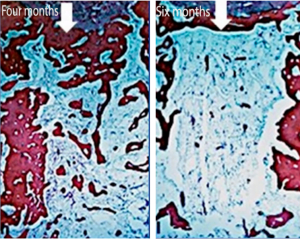 The hole is finally filled with young spongy bone. There is no trace of inflammation. The cortical lid is fully formed, but you can still notice the place of the hole.
The hole is finally filled with young spongy bone. There is no trace of inflammation. The cortical lid is fully formed, but you can still notice the place of the hole. - The bone finally heals after six months – 180 days. The entrance to the well is covered with a dense cortical bone. The space at the site of the former well is filled with spongy bone with large bone marrow spaces. The bone marrow contains a large number of adipocytes.However, these studies were conducted on dogs and it is impossible to transfer the results directly to humans. In dogs, faster metabolism and healing processes occur. Notwithstanding that, this research has great value as an aid to understand the biological processes.
When is the best time to place implants after a tooth extraction?
To answer this question, we turn to another study from 2008 by Dr. Trombelli and co-authors. The experiment was conducted on people who were informed and with all consents. They took histology from living patients at each of the stages of healing and, of course, a full protocol was kept.

These studies have confirmed that all the stages are exactly the same as the study on dogs, only the timing is slightly different. Let’s elaborate on that. Physically, the researchers took samples and analyzed the cell populations that are in the well.
It is useful for practicing dentists to look at a comparative analysis of the tissues and cell populations involved in different stages of hole healing. As would be expected in the early stages there is a high content of granulation tissue. After 6-8 weeks, osteoid and roughly fibrous bone is observed. Recall that osteoid in this case is an organic bone matrix of connective tissue, which will then be mineralized and transformed into normal bone.
| % content | 2-4 weeks | 6-8 weeks | 12-14 weeks |
| 100 | Coarse Fibrous Bone | Coarse Fibrous Bone | Cortical Bone |
| 90 | Connective tissue (osteoid) | Coarse Fibrous Bone | Coarse Fibrous Bone |
| 80 | Connective tissue (osteoid) | Coarse Fibrous Bone | Coarse Fibrous Bone |
| 70 | Connective tissue (osteoid) | Connective tissue (osteoid) | Coarse Fibrous Bone |
| 60 | Connective tissue (osteoid) | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 50 | Connective tissue (osteoid) | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 40 | Connective tissue (osteoid) | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 30 | Granulation tissue | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 20 | Granulation tissue | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 10 | Granulation tissue | Connective tissue (osteoid) | Connective tissue (osteoid) |
| 0-5 | Granulation tissue | Connective tissue (osteoid) | Connective tissue (osteoid) |
| Granulation tissue |
It was also found that it is impossible to establish the exact timing when the healing process is completed and at what time mineralization occurs. The healing of dental wells in humans is very variable. Therefore, each time the approach is individual and situational.
Now let’s move on to an equally important part, namely the healing of soft tissues when the tooth is removed. Fortunately, it is not difficult to track this process. Visual observation is enough, and biopsy is quite simple to take.
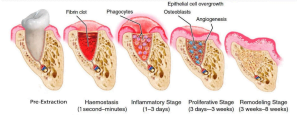
In the first three or four days there is nothing above the hole. Starting from the fourth day, the connective tissue matrix begins to form, and the proliferation of the epithelium begins from the edges of the hole. Moreover, the tissues begin to tighten from all sides: vestibular, oral, distal and mesial.
On the 21st-30th day, the epithelium will not only fill the entire hole, but keratinization of the epithelium over the hole will also begin. This is a very important point.
By the period of 90-180 days, almost complete healing is observed with the formation of cortical bone under the soft tissues. The periosteum is also formed and a characteristic groove can often be seen at the junction of the two layers of gums on the oral and vestibular sides.
Clinical classification of implant placement periods
To plan the surgery, it is important for us to know that the epithelium completely closes the hole from about the fourth week. The sixth week is considered the ideal time when the epithelium is completely closed and formed.
When implanted at this stage, the specialist will have no soft tissue deficiency, no disruption and loss of attached keratinized gum when the flap is sutured around the gum shaper. By the same time the bundle bone is completely gone, this is also positive for future implantation.
This is also reflected in the ITI Treatment Guide 3 classification, which is tabulated below.
| Classification | Description | Period after tooth extraction | Clinical situation during implant placement |
| Type 1 | Immediate implantation | Immediately after tooth extraction | No healing of bone and soft tissue |
| Type 2 | Early implantation after soft tissue healing | About 4-8 weeks | Gingival healing but no bone healing |
| Type 3 | Early implantation after incomplete bone healing | About 12-16 weeks | Gingival healing and substantial bone healing |
| Type 4 | Delayed implantation | About 6 months or later | Complete tissue healing in the well area |
Immediate implantation is used less often than the others and most often concerns cases where anterior teeth need to be restored.
Many schools of implantology consider the second type of early implantation to be preferable, for example, Professor Buser of the Bern School and his students. It really is one of the safest periods for dental implants including in terms of bone grafting. If you have to do bone augmentation, the chances of complications are minimal because the bone is still in the process of regeneration and there are plenty of protein factors that are favorable for both the engraftment of the new bone fragment and the integration of the implant.
The third and fourth types of implantation also have their advantages. In the latter, dentists are dealing with native bone, which is very good for primary stability. For a long time, the fourth type of implantation was considered the gold standard, and many experts still consider it as such.
In Part 2, we will take a closer look at the features of delayed implantation and take a closer look at how to maintain alveolar ridge width and height after a tooth extraction.
We hope you found this article useful and we look forward to reading more in the future.