In this article we talk about how to reduce the risk of infection in oral surgery. Implantation of dental prostheses belongs to the second class of purity of surgical wounds. This is a combined class of clean-contaminated wound that has a moderate chance of foreign matter or pathogenic microorganisms entering the wound. This is inevitable because it is not possible to completely disinfect the oral cavity, and surgery will take place in the presence of a microbiota. Infection rates with second-class surgical wounds average between 10 and 15 per cent. The task of implantologists, with the help of correct surgical techniques and prophylaxis with antibiotics, is to reduce the probability of infection to 1% or less. Behind the dry statistics of the percentage is the pain and suffering of specific people.
To begin with, we look at what else besides antibiotics affects the risk of complications associated with infection. We will not focus on aseptics and antiseptics. Since the importance of sterility of the tool and disinfection in the preparation of the operating field, as well as washing and treating the wound during and after the application of sutures is strictly prescribed in the protocols of operations. We will consider that, in terms of aseptics and antiseptics, everything was done 100% perfectly. However, the chance of infection after surgery remains. We have already mentioned why, because oral surgery is a pure-contaminated type, and even if the protocol of operations is strictly followed, the probability of infection remains. After all, the surgeon opens the gate with the first incision for micro-organisms, which are literally only a few millimeters and at most only centimeters from the incision site, in the folds of the mucous membrane. Neither washing nor disinfection can remove 100% of the microbiota. The probability of infection is affected by:
- Time – the sooner the operation is finished, the better. The lowest frequency of complications associated with wound infection is observed if the operation lasts less than one hour. It was noted that if the operation lasted less than an hour, infection of the wound was observed in no more than 1.3% of cases. While in operations the duration of which was three hours, this indicator reached more than 4%. On average, the chance of a post-operative infection can double with each hour the wound remains open.
- Experience and qualification of a surgeon. The frequency of complications in specialists who have made up to 50 root implants is 7.3%. Whereas more experienced colleagues have less than 2%. This is related to the previous paragraph. The less experience, the longer the operation lasts. Of course, the ease, speed of movements and muscle memory are working out, a novice specialist should not undertake the installation of several implants in one operation. First, you need to gain enough experience on single implants with the installation of simple healing abutments. Note that a single-moment implant with a permanent abutment and crown is also a complex procedure and should be treated with care.
Now let’s return to the main question of our article – prophylactic antibiotics before dental surgery. Unfortunately, at the time of writing there are no high-quality and uncontroversial studies that confirm the effectiveness of antibiotics. Those that do exist are somewhat contradictory. Some show good results, while others show little effect. It is very difficult to separate the effect on the incidence of complications of the surgeon’s experience and the patient’s condition prior to dental implantation.
Therefore, there are both opponents and supporters of prophylactic antibiotics among dental implant specialists. We are proponents of antibiotics and will further try to argue our position based on facts and results of other specialists.
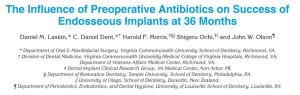
One of the documents on which our recommendations are based is an article on the prophylactic antibiotic protocol developed and published by
Dr. Resnick and Dr. Misch (Resnick and Misch 2008).
Dr. Resnick even has an entire book on the prevention of antibiotic infections.
A second equally interesting document is the work of Dr. Laskin and his team (Laskin et al 2000).
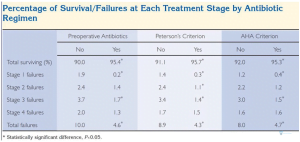
The work examined the effectiveness of preoperative antibiotics on the success of dental implants. The study involved almost 3,000 patients, who were divided into three groups. One group received prophylactic antibiotics from the penicillin group, another group received clindamycin or other broad-spectrum antibiotics from the lincosamide group, and the third group was a control group to whom no antibiotics were given.
The results were unequivocal that the groups that downplayed antibiotics before dental surgery had a markedly higher percentage of engraftment of dental implants. See the table below:
Summarizing the results, the number of complications in the groups taking antibiotics was not much more than 4%. In the groups where antibiotics were taken before the dental implantation, the frequency of complications was about 10%.
This was not a short study. A team of specialists observed patients over a period of 36 months. During this period, the healing implantation itself was the stage of implantation, and the prosthetic itself – the installation of the abutment and crown. Observations were made throughout the period as well as after the final restoration of the dentition.
This work was done very qualitatively and objectively, and is noticeable for not lobbying for neither the interests pharmacological companies nor the manufacturers of platforms for dental prosthetics.
This study confirms that it is possible and necessary to use antibiotics for prophylactic infection.
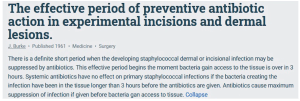
In addition to the already mentioned studies and the article by Dr. Carl Misch and Dr. Reznik, let’s turn to the earliest document, which examines the period and dosages of preventive use of antibiotics. This is a 1961 article by Dr. Berke.
Dr. Berke has proven in practice (in vivo) exactly how the antibiotic works when it makes sense to take it, and when taking antibiotics after surgery does not make much sense (more precisely, the effectiveness is not high).
It is important that at the time of the operation there is a sufficient concentration of antibiotic in the patient’s blood. To do this, you need to take a preventive dose an hour or two before the operation. It is the action of the antibiotic during the operation that allows you to minimize the risk of infectious complications.
For the sake of objectivity, we must accept and explain the point of view of specialists who do not consider preventive antibiotics mandatory. Indeed, tooth removal or single implantation is a fairly simple surgical procedure. The percentage of survival of implants even if there were no antibiotics is noticeably more than 90%.

The statistics show that the incidence of complications related to wound infection is 2.5-3% higher if the patient did not take an antibiotic before surgery.
We believe it is extremely important to inform the patient of all the risks. After all, it is up to the patient to decide whether to take antibiotics. If the patient has any chronic condition that can be affected by taking antibiotics, you should always consult with his or her doctor, then provide the patient with all available information about the risks and consequences.
This is extremely important in terms of the risks of a dentist. The specialist’s area of responsibility is to perform the operation quickly and carefully to install the implant in an ideal geometric position. Even if the treatment protocol was fully followed, something could go wrong and it may need to be re-implanted. In this case, it is performed at the expense of the clinic. If the doctor prescribed antibiotics, but the patient did not take them, then at whose expense the repeated surgical intervention will be done is still a big question.
What are the best antibiotics to prescribe?
This is the most complicated question, because there are always contraindications and you must always consult a specialist. However, there are general recommendations based on practical experience and research results.
For the prevention of infection in dental implants, a broad spectrum of antibiotics is necessary. They must act both on aerobes and anaerobes, also on Gram-negative, and on cocci (Staphylococcus aureus, etc.) and bacilli. In short, they must act on all members of the oral microbiota that can cause an infectious infection.
Most often penicillin antibiotics, such as Amoxicillin with clavulanic acid, are used for this purpose. Clavulanic acid itself acts as an antibiotic, and is effective against penicillin-resistant bacteria.
We will not give the commercial names of these drugs, but they are available all over the world. This antibiotic is bactericidal. That is, it not only inhibits the development, but also destroys the shell of the bacteria and destroys the source of infection.
This is not the only antibiotic with this effect. The main thing at this stage is to know what effect the medicine should have. A particular drug will need to be chosen specifically for the patient. After all, the situation when a patient is allergic to antibiotics of the penicillin group is not uncommon. The good news is that it is always possible to find an equivalent material for the action, to which the patient will not be allergic or have other contraindications.
Chlorhexidine bigluconate is a powerful bactericidal agent that is prescribed for mouthwash twice a day until the stitches are removed.
It is also important to educate the patient about the rinse. Because chlorhexidine stains the tooth wells darker, patients tend to substitute another product or stop rinsing early.
In fact, staining is a sign that chlorhexidine is working properly. The dark plaque is actually the destroyed manifested and fixed microbiota.

After the end of the course of treatment, the dark plaque is easily removed. But please be aware that patients can find “alternative” drugs with a dubious antiseptic effect, or even variants of “chlorhexidine” that do not stain teeth dark. If a drug does not stain plaque and does not destroy the microbiota, its chlorhexidine content is doubtful.
Prescribing antibiotics depending on the complexity of the operation
Here we will also rely on the work of Dr. Carl Mirsch and Dr. Reznik, who have developed a prophylactic reception scheme. These principles still adhere to the protocol developed by Carl Misch at the Temple University in Philadelphia, USA.
| Patient health status | Procedure type | Description of procedure type | Antibiotic | Antiseptic |
| ASA1/ASA2 | Type 1 | Simple Removal, Single Implant Installation, Implant Opening | No need | Gargle with chlorhexidine solution twice a day |
| ASA1/ASA2 | Type 2 | Multiple simple removals, Traumatic removals, Multiple implants with limited flap detachment, Immediate implantation | Amoxicillin: 1g 1 hour before surgery, and 500mg in 6 hours | Gargle with chlorhexidine solution twice a day |
| ASA1/ASA2 | Type 3 | Multiple Implants with Significant Flap Detachment, Multiple Immediate Implantation, Directed Bone Regeneration (with xeno, alomaterials) | Amoxicillin: 1 g 1 hour before surgery, and 500 mg twice a day for 3 days | Gargle with chlorhexidine solution twice a day |
| ASA2
long surgery; less experienced surgeon; immunodeficiency; active periodontitis |
Type 4 | Multiple simple removals, Traumatic removals, Multiple implants with limited flap detachment, Immediate implantation | Amoxicillin: 1 gr 1 hour before surgery, and 500 mg twice daily for 5 days | Gargle with chlorhexidine solution twice a day |
Dosage recommendations are given for patients weighing between 60 and 70 kg. The exact dosage in a particular case depends on the patient’s weight and other recommendations of the treating physician.
The international classification, which we have already mentioned, is used to assess the patient’s state of health.
In a nutshell:
- ASA1 is a practically healthy person without chronic diseases;
- ASA2 – there are chronic diseases that can easily controlled with medication, such as mild hypertension, etc.;
- ASA3 – severe systemic diseases that have weakened the immune system and cannot always be controlled with medication, and medications such as immunosuppressors themselves can cause complications during implantation.
For more severe conditions, dental implantation is not recommended.
Also note that surgical procedures go into difficulty type 4:
- Duration more than 1 hour;
- Surgeon with 50 or fewer successful implantations;
- Immunodeficiency condition – caused by disease or treatment (chemotherapy, radiation therapy, immunosuppressants in high doses);
- Active periodontitis.
We hope the material in this article was interesting and useful. We look forward to the next publication.