Comparison Between Digital and Conventional Workflow in Implant Prosthetic Rehabilitation: A Randomized Controlled Trial
Our website already features several articles dedicated to the digitalization of dental processes. Most often, this involves CAD/CAM technologies, where a digital image of the patient’s jaws and remaining teeth is captured, and the design of prostheses and surgical templates is processed in a virtual environment. The patient experiences minimal discomfort, as there are fewer fittings and adjustments, and in simple cases, the prosthesis fits immediately.
However, is everything as seamless as it seems? Many specialists still use conventional methods and are reluctant to switch to digital. Recently, our Italian colleagues published a study on this topic, and we found its results interesting enough to review and highlight the key points. You can read the original study in full here.
The aim of the researchers’ work
There are many scientific and promotional publications regarding the advantages of the digital workflow. However, some analog operations are still necessary, so prosthetics are often performed using a combined workflow. For example, the casting and production of a physical model of the jaws are performed using a conventional analog workflow, while the development and production of the prosthesis are done using digital technologies. To achieve this, the casts and models are scanned and converted into a 3D file. Sometimes, a physical model of the jaws is required during the digital scanning stage, and it is printed on a 3D printer, which in most cases provides greater accuracy compared to plaster models.
Regarding the comparison of the accuracy and quality of prosthetics performed by different methods, there is still no unified data. Some clinical studies for single implants show greater accuracy in prosthesis production using the digital workflow. Other publications indicate no significant difference in the accuracy of prostheses manufactured by different methods. However, researchers agree on one point, confirmed by several systematic studies: the digital workflow is easier for patients to tolerate, and the time required to obtain digital impressions is significantly shorter.
Until now, there have been no full-scale randomized clinical trials comparing digital and conventional workflows. Therefore, the research team aimed to compare the accuracy of fit and the quality of prosthesis production, as well as to assess patient satisfaction with both the process and the result. To achieve this, a three-component randomized clinical trial was conducted. The following workflows were compared:
- Fully digital workflows (DG)
- Combined analog–digital workflows (ADG)
- Fully analog workflows
The criteria for comparison were:
- Interproximal contact (IC) quality.
- Occlusal contact (OC) quality.
- Marginal fit (IF).
- Impression-Taking Time (IT).
- Patient satisfaction through the VAS scale.
The task is to perform a sufficient number of prosthetics using all methods and compare the results.
Materials and methods for studying workflows
Let’s briefly recall what a digital workflow involves. First, you need to obtain the source data.
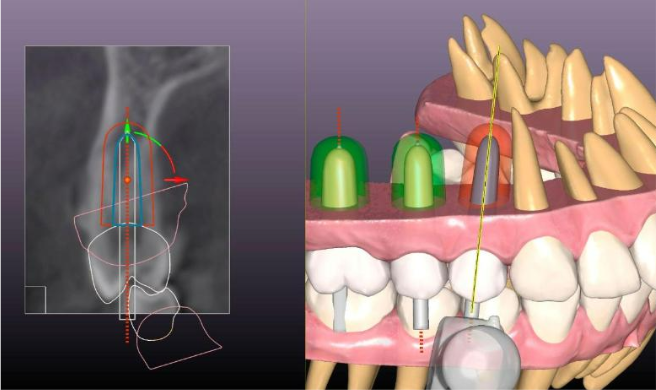
- The patient must undergo a high-frequency CBCT scan. The resulting images/sections are converted by specialized software into a 3D model of the patient’s jaws. This model clearly shows the condition of the patient’s bone tissue but requires a more accurate representation of the remaining teeth and soft tissues. Moreover, computed tomography data may have defects and inaccuracies, for example, due to micro-movements of the patient’s head or the presence of metal elements in the remaining teeth. Therefore, when converting CBCT data into a 3D file, corrections are required. In some cases, the dentist may request a repeat tomography.
.
- Optical scanning of the oral cavity is performed using an intraoral scanner in all planes. This means that the lower and upper jaws are scanned separately, as well as the outer part of the closed teeth. The scanning data is then combined to provide a clear picture of the condition of the remaining teeth and soft tissues. Many dentists are still wary of the scanning results due to the fact that the first models of intraoral scanners were indeed less accurate than conventional impressions. Additionally, achieving good results requires skill in using the intraoral scanner. However, this is not a difficult skill to acquire, and sufficient smoothness and continuity of hand movement with the scanner can be developed in a couple of days.
- Creating a working virtual model. Modern CAD/CAM software packages allow the combination of data from the CT and optical scanner into a single 3D model with real dimensions.
- Operation planning. The selection of implants by diameter and length, as well as the choice of seating depth, also occurs in virtual space. Almost all manufacturers, including Uniqa Dental, provide virtual images of their implants and multi-unit abutments. This is because screw retention is most often used in the digital prosthetics workflow.
.The 3D model clearly shows the depth of the mandibular nerve relative to the alveolar ridge, and the thickness of the bone tissue of the upper jaw, making it possible to select implants without perforating the membrane lining the maxillary sinus. The virtual model allows you to try on several implant options and choose the optimal angle for placing the implants.
- Development and production of a surgical template. The template is completely customized, making it easier for the surgeon to prepare the implant bed.
.
- Development and production of a prosthesis. For one-stage implantation with the installation of a prosthesis, a temporary prosthesis is made of PEEK plastic. If the prosthetics are carried out according to a deferred workflow, a permanent prosthesis is made immediately, for example, milled from zirconium dioxide. The accuracy of development in the digital workflow is so high that the prosthesis often fits perfectly and does not require revision. However, in the case of a deferred workflow, when the patient returns with fully integrated implants, a second scan is performed using an optical intraoral scanner. During the scanning, markers are installed in the implants to show the exact position and angle of inclination of the implant relative to the dentition. Based on the updated data, the prosthesis is developed.
Study design and equipment
In total, 72 implants and crowns for them were installed in the study for 60 patients, who were divided into 3 groups. All patients underwent single-tooth implant-supported prosthetics with support on the implant. In accordance with the CONSORT criteria, the following locations were chosen for the experiment:
- University of Bari “Aldo Moro” (Italy)
- Institute of Magna Graecia (Italy).
The study was conducted in accordance with the Declaration of Helsinki, and the workflow was approved by the Local Ethical Committee of Hospital “IRCCS Giovanni Paolo II” (Study n. 1355/CE). The study was registered at ClinicalTrials.gov (NCT06215781).
All patients were volunteers and signed consent forms. The selection criteria for the study were quite strict. Each participant met the following criteria:
- Good oral health
- No dental caries
- No periodontal disease
- If implant-supported dentures had already been installed, the patient must have been successfully followed-up by a dentist for 6 months to 1 year, with no complications registered
- No parafunctions such as bruxism, etc.
- Patients must be generally healthy
Exclusion criteria for the experiment were the following:
- Poor oral health
- Presence of caries or periodontitis
- Pronounced parafunction (bruxism) and TMJ pathology (condylar meniscal incoordination, ankylosis, joint click)
- Poor general health
- Failure to complete the follow-up period
The initial stage was diagnostics. At this stage, all patients underwent orthopantomography and obtained data from a small FOV Cone Beam Computed Tomography (CBCT). For consistency, the same NewTom GiANO HR device was used for all patients.
All patients followed the proper workflow and the following conditions were met for all:
- Placement of an implant at least 3 months after tooth extraction
- Loading of the implant at least 3 months after placement to ensure successful osseointegration.
The success of osseointegration was assessed using an intraoral X-ray machine (Sopro Imaging, La Ciotat, France). The allocation of patients to groups was completely random, using the random number generator Research Randomizer by Geoffrey C. Urbaniak and Scott Plous, accessed at https://www.randomizer.org on January 23, 2018. This demonstrates the seriousness of the researchers’ approach and the expected reliability of the results obtained.
Description of a fully digital workflow
Digital impressions were performed with the intraoral scanner Trios 3 (3Shape, Copenhagen, Denmark). Correct use of this scanner allows recording of the occlusal and lateral surfaces of the teeth. The scan results were exported to STL format and used for the development and testing of the prosthesis. Final crowns were made of monolithic colored zirconia CAD-CAM milled with Nobel Procera Crown Zirconia (Nobel Biocare, Zurich, Switzerland).
The pictures below show one of the clinical cases with a fully digital workflow.
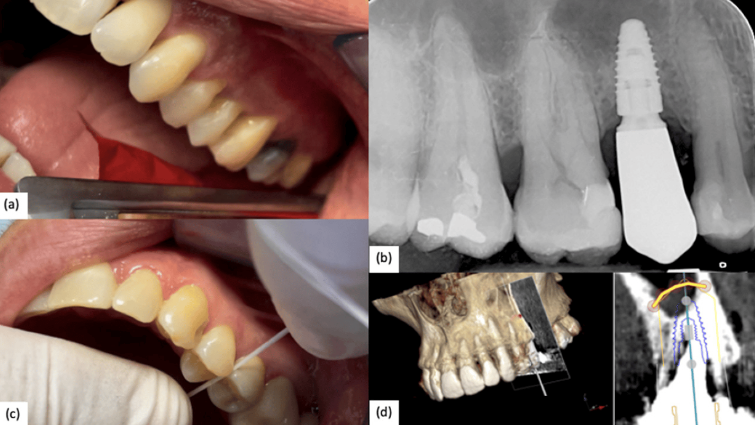
(a) Occlusal contact check; (b) Intraoral Rx confirms a correct implant–abutment fit; (c) Interproximal contact check; (d) Digital planning of implant insertion. The yellow line represents the expected maxillary sinus lift.
Description of a Combined Digital–Analog Workflow
For the definitive impressions, highly hydrophobicsilicone Hydrorise (Zhermack, Badia Polesine) (single-phase two-component technique) was used. The impressions were cast in type IV GC Fujirock Gold (GC Corporation, Tokyo, Japan) precision plaster. The physical impressions were converted into a digital file using a DOF Swing laboratory scanner (DOF, Inc., Seoul, Republic of Korea). A resin provisional was applied when necessary. Final crowns were made of CAD-CAM milled monolithic colored zirconia. In some cases, cut-back zirconia crowns were made with subsequent ceramic vestibular layering in the esthetically relevant areas.
The pictures below show one of the clinical cases of prosthetics using a combined workflow.
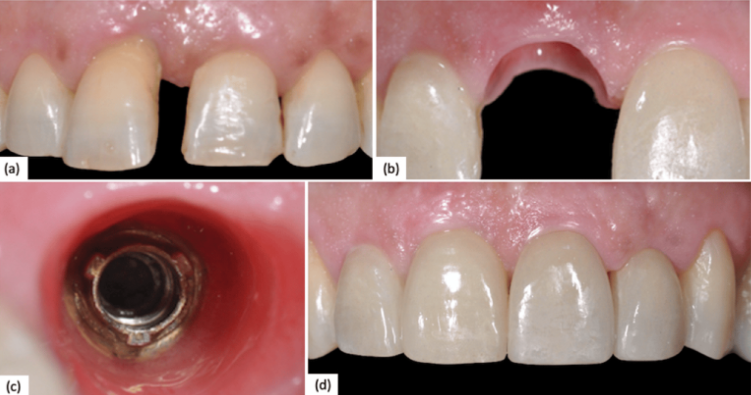
(а) Preoperative clinical situation; (b) Peri-implant tissue after provisional conditioning; (c) Peri-implant tissue before polyvinylsiloxane impression; (d) Final restoration.
Description of a Fully Analog Workflow
The same material was used for the casts as in the previous workflows. Plaster models were cast from the same brand of plaster, which provides minimal shrinkage. Permanent dentures are metal-ceramic crowns. The base is made of a chromium-cobalt alloy with subsequent feldspathic ceramic layering. Digital steps were not carried out.
The pictures below show one of the clinical cases of prosthetics using a fully analog workflow.
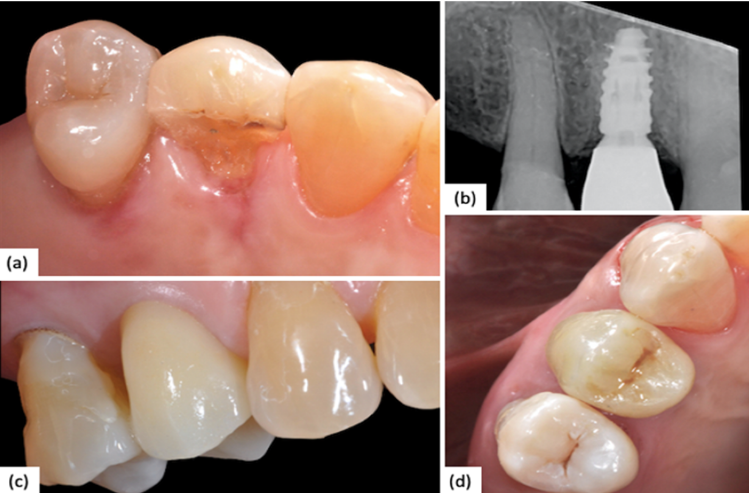
(а) Preoperative clinical situation showing a vertical fracture of 1.4; (b) Intraoral Rx showing no marginal implant–abutment gap; (c) Vestibular view of final restoration; (d) Occlusal view of final restoration.
As you can see from the pictures, all three restorations look very good, and there are no problems with the gums. For the integrity of the experiment, all three workflow variants were performed by the same specialists—three highly qualified professionals. The same dental technician was involved in the production of prostheses and other laboratory procedures.
The results of the work were evaluated by two experienced clinicians with many years of experience in prosthetics, who are also academic professors (MC and SC). The verification stage was not blinded; the specialists knew from which group each patient was, but they understood the importance of the work and remained objective. After checking IC, OC and the marginal fit, the patients were surveyed about their satisfaction with the process.
Let’s take a closer look at the quality criteria that were assessed by the invited clinicians:
- Interproximal contact (IC). This is the entity of contact between the prosthetic crown and the adjacent tooth. Measurements were taken using waxed dental floss (Essential floss, Oral-B, Procter & Gamble, Cincinnati, OH, USA). The resistance to sliding of the floss into the interproximal space was evaluated. The resistance was divided into five categories from 0 to 4, where 0 means no contact and 4 means excessive contact such that the floss cannot pass through. Interproximal contact values were classified as follows:
– Missing: crown remake required
– Slight: slight interproximal adjustment required
– Good: requires no adjustment
– Optimal: requires no adjustment
– Excessive: slight interproximal adjustment required - Occlusal contact (OC). The accuracy of the occlusal contact of the prosthetic crown with its antagonist tooth. To assess the contact and identify discrepancies, both static and dynamic, dichromatic articulating paper (Bausch Articulating Paper, Bausch Inc., Nashua, NH, USA) was used. To standardize the results, four OC quality categories were proposed:
– 0 means no contact between the crown and antagonists
– 1 means contact that does not require correction;
– 2 means slightly altered contact requiring minor correction;
– 3 significantly altered contact between the prosthetic crown and its antagonist, requiring significant correction. - Implant–Abutment Fit (IF) or marginal fit. The presence of a gap between the crown margin and the abutment was assessed using a Rinn intraoral x-ray at 0° +/- 10°. This radiographic approach is a well-established method for assessing potential gaps between prosthetic and implant components that may reduce the overall survival of the prosthesis. A score of 0 was assigned if there was no gap and 1 if there was a gap. The images below show the results of three patients.
.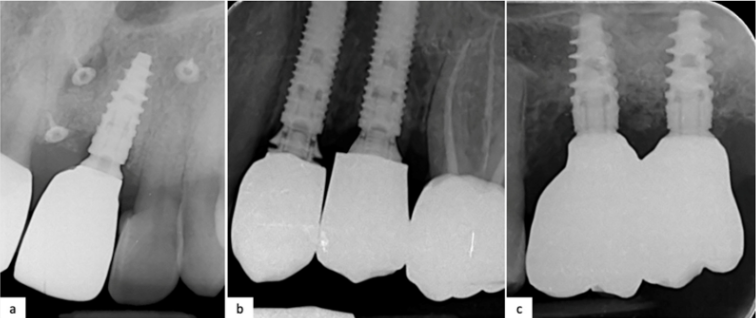
Intraoral Rx: (a) 2.1 after 1 year which followed the fully digital workflow after a GBR (Nobel Biocare N1); (b) 2.5 and 2.4 after conventional workflow that shows an implant–abutment misfit of 2.4 that needs to be corrected (Nobel Parallel TiUltra CC); (c) 1-year follow-up Rx of 2.7 and 2.6 which followed a combined analog–digital workflow (Nobel Active TiUltra CC)
.
- The Impression-Taking Time (IT) was estimated in seconds (s).For the analog technique, the total calculated time is the sum of the time for the extraoral mix of the impression material and performing the procedure; for the digital technique, the calculated time is the time required to fully scan the arch (time provided by the scanning software, version 21.4).
- Patient Comfort. All participants completed a questionnaire to assess their comfort during impression taking procedures. The included a VAS scale in order to quantify the degree of comfort felt during the procedure. The authors decided to consider only the comparison between digital and combined workflows to avoid redundancy of results, because the comfort experienced by the patient is critically affected by the type of impression. Combined and fully analog workflows shared the same analog impression procedures; thus, their results are similar.
Statistical analysis methods for evaluating results
In order to determine the presence of statistically significant differences between the means of the parameters examined in the groups previously reported, a one-way ANOVA (analysis of variance) statistical model was used. Formally, the null hypothesis is the following: there are no differences between clinical parameters based on different treatment flows. The alternative hypothesis is the following: at least one group presents a significant difference. The error α is set to 0.05. In the case wherep< α, the null hypothesis H0 is rejected. In cases where the differences between the groups are statistically significant (p< 0.05), a post hoc analysis will further be performed using the LSD (least significant difference) Fisher test. This test allows us to assess the presence of a statistically significant difference between each pairwise combination of the groups when LSD values were lower than |µ1− µ2| values. Fisher’s contingency test is used to measure parameters with binary values. The data are calculated using the electronic program MATLAB (MathWorks version 23.2, Natick, MA, USA).
Results
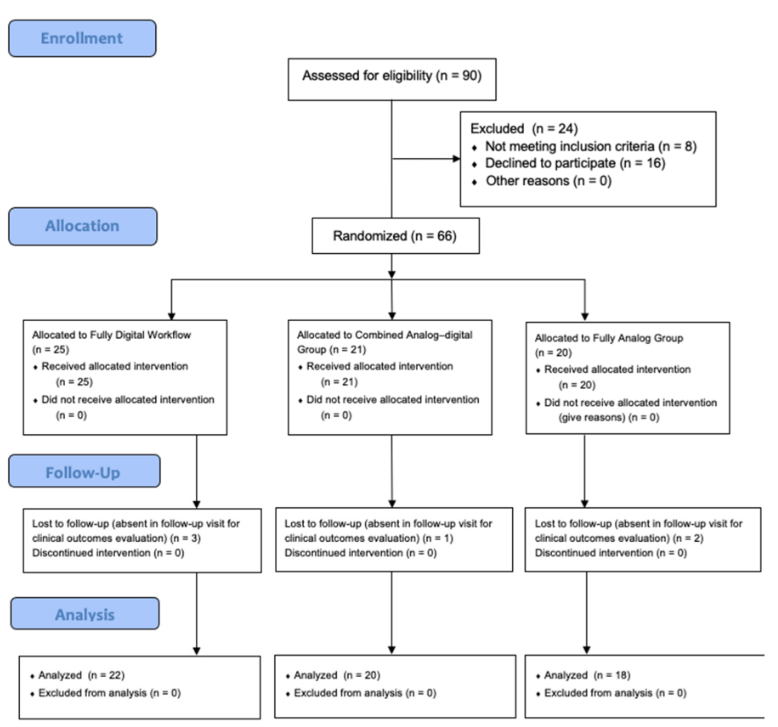
A total of 60 patients, 33 females and 27 males, participated in the study over 5 years and were randomly assigned to groups following the CONSORT criteria, see diagram below.
.
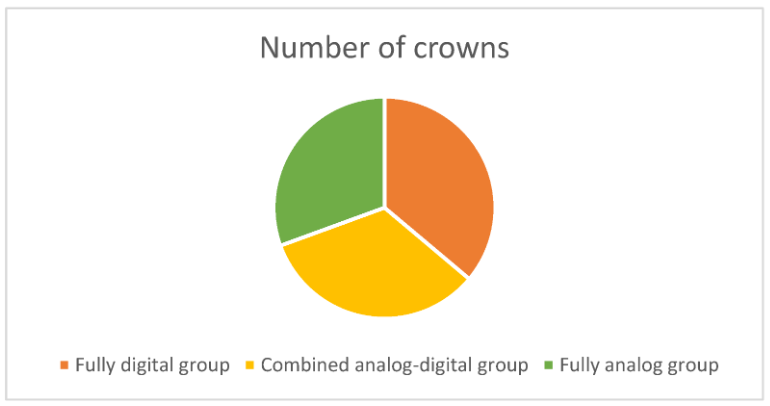
Based on their diagnostic results and needs, 72 implants and crowns were positioned for them.
- The fully digital group (DG) – 26 crowns.
- Combined analog-digital group (ADG) – 24 crowns.
- Fully analog group (AG) – 22 crowns.
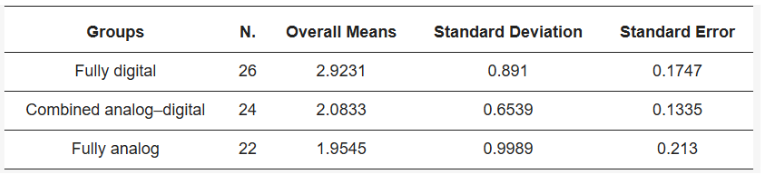
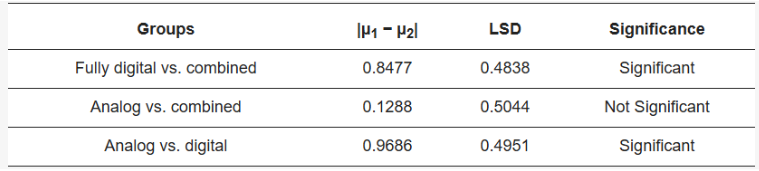
The results of interproximal contact (IC) testing showed a significant difference in the ANOVA test (p=0.0003), see Table 1.
Table 1 Interproximal contact
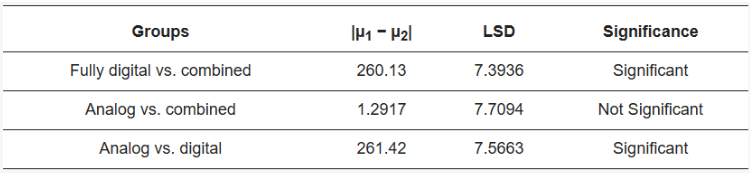
After the Fisher’s LSD test, the means of the intensity of IC of the DG group was found to be statistically higher compared to AG and ADG groups, see the table below. As a reminder, Fisher’s Least Significant Difference (LSD) test is used to compare the mean values between groups after conducting a one-way analysis of variance (ANOVA). This test helps determine which groups have statistically significant differences from each other.
Table 2 Fisher’s interproximal contact test (LSD)
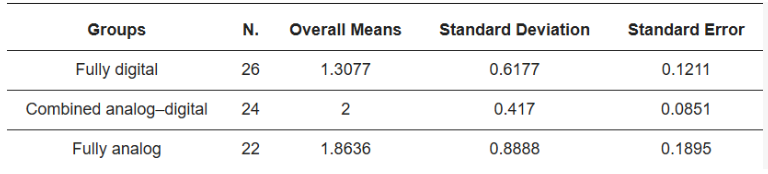
Occlusal contact (OC) quality testing also showed a significant difference between the three groups (p=0.0009), see Table 3 below.
Table 3 Occlusal Contact (OC)
After conducting Fisher’s LSD test, it turned out that the values of group DG were higher compared to groups AG and ADG, see Table 4.
Table 4 Fisher’s LSD test between groups
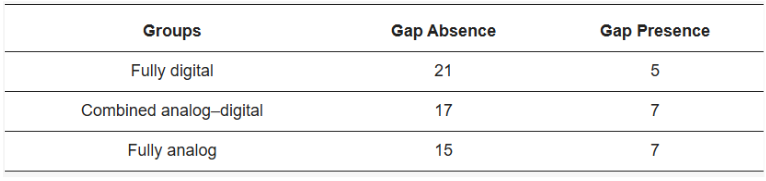
The results of the marginal or implant–abutment fit (IF) test showed no significant differences between groups (p=0.5966) see Table 5.
Table 5. Marginal fit accuracy according to Fisher’s test
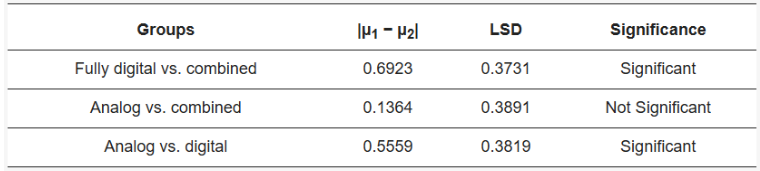
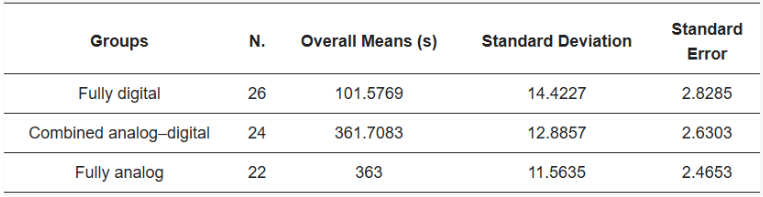
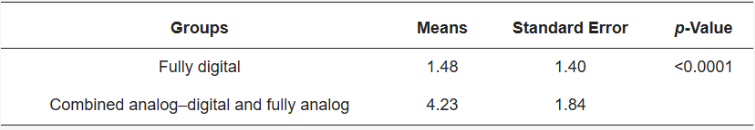
Impression-Taking Time (IT) showed a significant statistical difference between groups (p<0.0001) in favor of the digital workflow, see Table 6.
Table 6 Impression-Taking Time means
The Fisher’s test confirms that the digital workflow is the fastest in producing an impression, see Table 7.
Table 7 Fisher’s LSD Test
Patient comfort assessment showed better satisfaction with the fully digital workflow, see Table 8.
Table 8 Satisfaction according to Student’s t-test
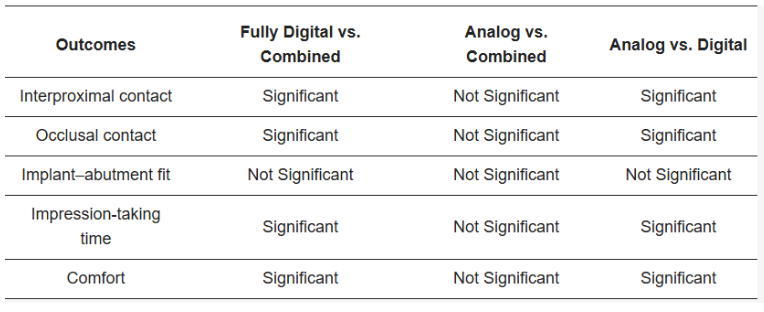
The final results of the five-year randomized clinical trial are summarized in Table 9.
Table 9 Overall results
Conclusions based on the results
Since the different methods showed significant differences, the null hypothesis that all methods give the same result was not confirmed. The best results were shown by the fully digital workflow, which excelled in the following areas:
- Interproximal contact is significantly better compared to the analog workflow, and somewhat better compared to the combined workflow
- Occlusal contact is significantly better compared to other methods
- Impression-taking time is excellent, with scanning results significantly faster than taking a silicone impression
- Patient satisfaction is higher, with minimal discomfort associated not only with speed but also with the absence of unpleasant sensations from the silicone tray in the patient’s mouth.
The quality of the marginal fit of the crown to the abutment did not show any significant difference between the three methods.
Therefore, the digital workflow has shown clear advantages and is preferable. It is evident that in the coming years, more specialists will adopt digital technologies. This will be facilitated by the reduction in prices for equipment related to the mass production of scanners, 3D printers, and milling machines for prostheses.
Considering that the study only addressed single defects, where the accuracy of the crown itself is not as critical, even more advantages of digital technologies will be revealed for multiple restorations. In particular, higher accuracy of prosthesis manufacturing and the use of screw fixation, which makes it much easier to achieve a good passive fit.
We hope we have managed to attract more attention to digital technologies. Until the next publications.
Source
Corsalini, M., Barile, G., Ranieri, F., Morea, E., Corsalini, T., Capodiferro, S., & Palumbo, R. R. (2024). Comparison between conventional and digital workflow in implant prosthetic rehabilitation: A randomized controlled trial. Journal of Functional Biomaterials, 15(6), 149. https://doi.org/10.3390/jfb15060149