Which Is Better: Screw-Retained or Cement-Retained Implant Crowns? A Comparison Guide for Dental Professionals

In this article, we will try to find out whether screw retention is superior to cement retention. We will discuss it from a practical point of view, based on research results, and case studies. We would like to make it clear that neither system has an unqualified advantage over the other. We would also like to reassure the fervent admirers of one system or the other, that both fixation methods are good enough and can be used to achieve a high-quality restoration with a positive long-term prognosis. However, screw retention is becoming increasingly common with the spread of CAM/CAD technology and the use of prostheses made of a single piece of zirconium dioxide. Let’s go through them all in order.
Contents
When only screw-retained dentures can be used
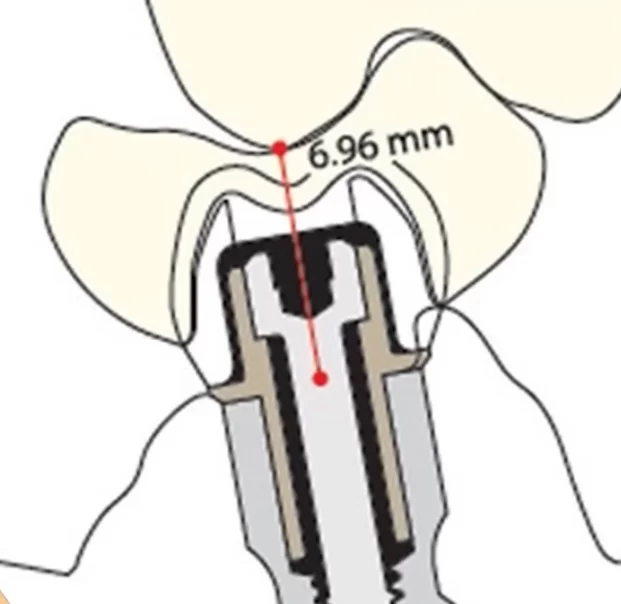
- A direct indication for manufacturing a screw-retained restoration is when you have an interocclusal distance from the screw platform to the nearest antagonist cusp of seven millimeters under. This is a situation where it is simply physically impossible to make a cement fixation.
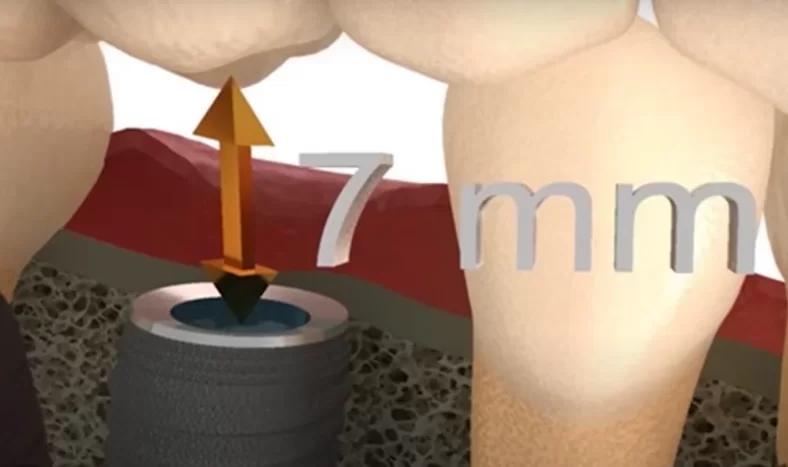
Critical distance from the implant base to the antagonist tooth for which only screw fixation should be used
There is an explanation for this, and it comes from the fact that the height of the abutment for a reliable cement fixation must be somewhere around five millimeters and the thickness of the denture material on the occlusal side is about two mm, which is extremely small. Whether it is a metal-ceramic or zirconia restoration, it is virtually impossible to fabricate an abutment and crown with these limitations in both cases.
All this is drawn in many textbooks and has been an indisputable rule for many years.
2. Screw retention is a conditionally removable restoration and is, therefore, always used when the restoration needs to be removed on a regular basis. The prosthesis is fixed with screws to the abutment and the screw shafts are covered with composite. If necessary, the screw shafts can be easily released and the prosthesis removed. This is especially relevant if a temporary denture is fitted first and after a few months it is necessary to replace it with a permanent denture. Yes, it can be argued that there is a temporary cement for cement fixations, but there are often cases where the denture becomes cemented before the time is up, or the crown cannot be removed without destruction.
What is the essence and simple nature of cement-retained dentures?
Nowadays, it seems that screw fixation is new, but in fact screw fixation has been used in implantology since implants were introduced. Even with the very first implants of the Branemark system, screw fixation was used. Of course the system was different to today. Cement fixation has become widespread as a more convenient form of work from the point of view of orthopedists.
Since an implant is an artificial root and an abutment is essentially a stump of a tooth, there is nothing easier for the dental technician than to process the abutments and make a crown or bridge, and for the denturist to cement the denture. In addition, the cement itself can compensate for small inaccuracies in the manufacturing of the denture. The installation of such dentures is relatively easy.
Both techniques have coexisted peacefully for a long time, but disputes nevertheless occurred.
Which type of retention is more reliable in the long term?
There are proponents of screw fixation alone. There were those who favor cement fixation. It got to the point that in 2009, Dr. Salvi and his team from the University of Bern did a special review for a consensus conference held at ITI.
Here are the conclusions of Dr. Salva’s group’s work:
“No increased mechanical or technical risks were found for fixed prostheses after reviewing three of four studies (one prospective, one retrospective, and one sequential study) comparing screw fixation with cement fixation”.
That is, the group found no difference, either in terms of survival or any complications.
To add a bit of humor to the question: Who’s cooler skiers or snowboarders? We get the answer – both are cool. However, recall that at that time metal-ceramic restorations dominated, and now zirconia is increasingly used. Although the risk of complications has not been affected by the use of the new material, screw retention, especially when combined with more precise manufacturing of prostheses using CAD/CAM technology, has become more convenient and easier for both the specialist and the patient.
How the confrontation between cement and screw fixation methods began
Let’s understand why this confrontation appeared in the first place. The point is that when implants became available on the market, standardized superstructure elements, in particular abutments of different configurations, appeared immediately.

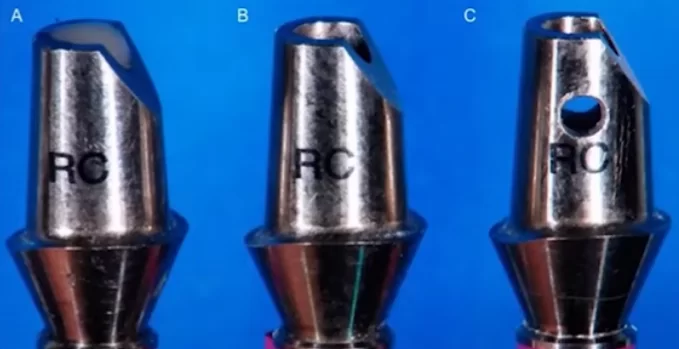
Prepared abutments for implants with internal hex interface – from left to right: straight abutment for cement fixation; angled abutment for cement fixation; angled abutment with anatomical ledge along the gingival line for cement fixation; angled multi-unit abutment for screw fixation.
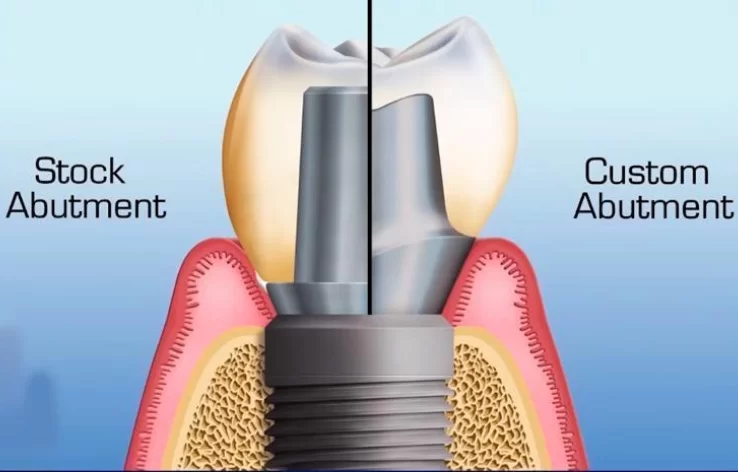
Restoration on implants follows the standard scheme. The implant itself is a root prosthesis, the abutment, which is placed in the implant, is a kind of tooth stump, for which the dental technician makes a crown (single, bridge or full denture).
For a long time, only standard factory abutments were used, which were finalized by the dental technician for a specific type of denture. Until the 2010s, the main mass of abutments was stock abutments from manufacturers. Around the same time, more technical possibilities to produce abutments individualized to the gingival profile appeared.
There is no doubt that the standard abutment is good enough plus inexpensive due to mass production. It is made in the same factory where the implants are made, so they have perfect interface compatibility.
The technician takes a standard abutment, removes as much as necessary in height, creates some semblance of a profile, then models a metal-ceramic crown and sends the work to the clinic.
The dentist receives the abutment and crown, screws in the abutment and seats the crown on cement. That’s it, it’s a very simple scheme that a lot of specialists are still working with today.
Not everything, however, is so simple. As an example, take a look at a rather old restoration. There you can see that a planar interface (external hex) is used and a single crown is cemented on a standard abutment.
It’s not unusual, they’ve done it everywhere and got good results.
Now look at a standard abutment that “sank” into the patient’s gingival hole.

The patient’s gingival thickness is too thick for this type of abutment – cemented crowns are not recommended under these conditions
Most importantly, you can’t say that the technician made a mistake. He could not have done it differently. If we look at the abutment itself, we can see that the abutment neck is standard and there is nothing that can be done about it.
Gingival thickness varies from patient to patient. If the gingiva was thinner than the abutment cervix, the technician would most likely grind off the cervix with an engraver. In this case, the margin of attachment of the crown was deep under the gingiva, and this gives rise to difficulties, because the dentist realizes that he will not be able to effectively remove the cement, which will protrude from the margin of the crown.
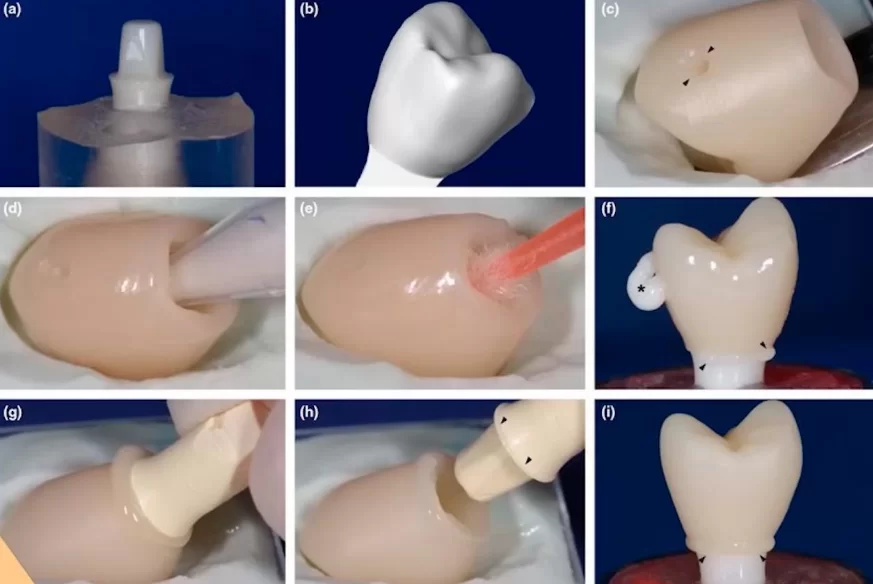
Such situations have given rise to different techniques that would make it possible to ensure that the cement does not protrude into the peri-implant space. For example, as in the image below, a so-called duplicate abutment was made.
That is, a duplicate abutment made of silicone or composite is made, and then the cement is worn on the duplicate and put into the crown, after which the duplicate is removed and the crown with cement inside is placed on the abutment in the patient’s mouth.
Everything had to be done very quickly to remove the duplicate, remove the excess and place the crown in the mouth. It was believed that with this method there would be no excess cement in contact with the soft tissues at the level of the gingival cuff. In principle, the method works and can be used for single crowns. However, when the denture is complex and there are many crowns, this method is almost impossible to use.
Most importantly, it does not give a 100% guarantee that the cement will not come out.
There have been other ways to solve this problem. For example, papers have been written with these recommendations, see the illustrations below.
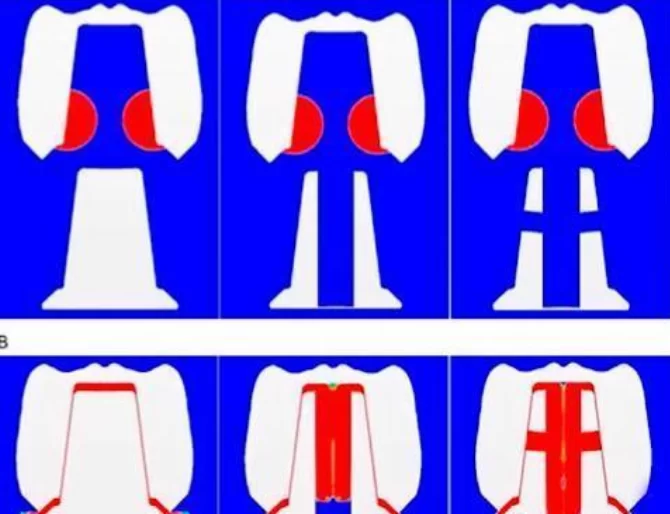
This work from 2014 studies how to make sure that the cement does not squeeze out into the peri-implant tissues.
In this case, it was suggested to drill out the abutments and make special ventilated canals to allow excess cement to escape. The results were not bad, and this is also a working method.
Another option was proposed in a paper from 2018, where it is suggested to make a hole in the crown so that excess cement under pressure goes there.
Unfortunately, practice shows that none of these techniques can save you if the edge of the crown sinks too deeply into the gingival cuff.
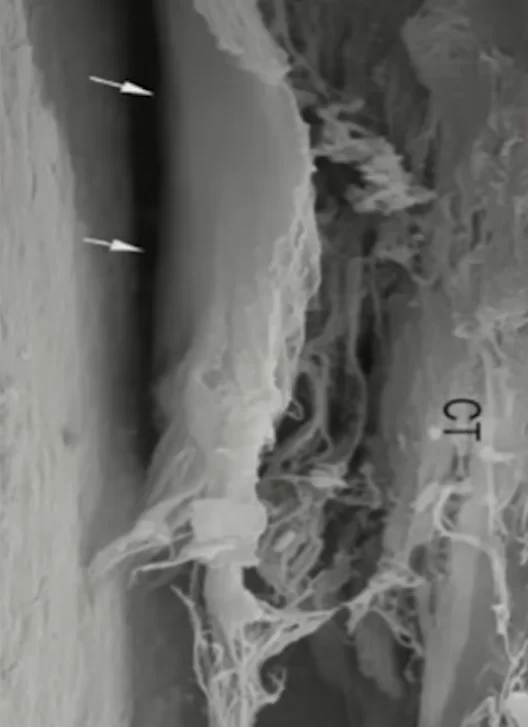
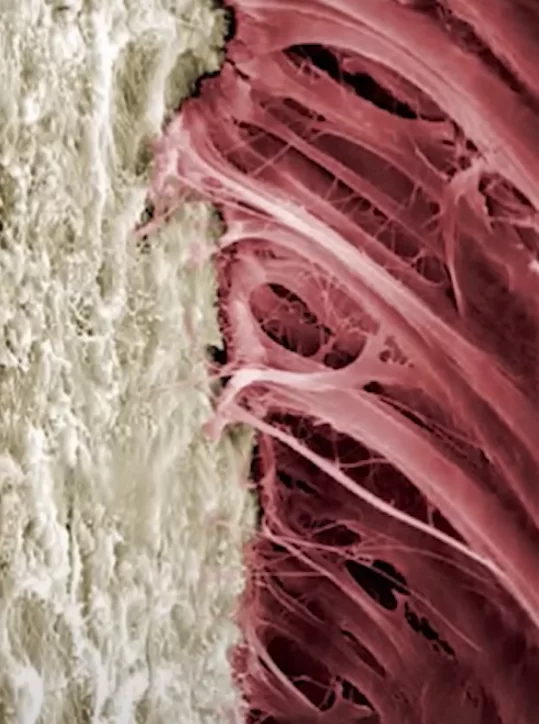
We have already discussed in detail the difference in the structure of the gingival cuff around a living tooth and around an implant in our series of articles on soft tissue integration. You and I know that the gingival connection to the implant is not very strong.
When the crown is placed, some of the cement is squeezed out and tears the fragile collagen bonds and penetrates wherever the initial impulse from the placed crown allows. The only thing that could stop the flow of cement is a normal gingival ligament, but there is none around the implant.
We have mentioned only a small number of the techniques aimed at combating cement penetration into the peri-implant space. They all have one thing in common – there is no guarantee that cement extrusion will not occur.
In their book “Zero Bone Loss”, Dr. Linkevičius and his colleagues discuss many techniques, with good illustrations, and confirm the conclusion that no technique can save from cement penetration if the separation line between the crown and the abutment base is too deep.
If one does not switch to screw fixation, there are two methods to solve this problem:
- Stock abutments with different base heights. You can choose the closest possible variant to the thickness of the patient’s gingiva and bring the edge of the crown to a minimum depth. No drilling of abutments, making duplicate abutments and other shamanism is required. The problem with stock abutments is that it is still not possible to get perfectly in the gingival line.
Standard abutments with different base heights (available with gingival heights from 1 to 5 mm)
- Custom abutment manufacturing. Here, it is not only possible to raise the abutment platform to a height where the cement can easily be removed, but also to take into account the difference in gingival level on the cheek and tongue side of the denture. This allows for a perfect aesthetic result. Molded individual abutments were the first to appear. In those days, CAD/CAM technology was not yet available, so the dental technician made an abutment template out of wax and ashless plastic, and then cast the abutments in metal. Let’s break down the analog technique in a little more detail. The dental technician received the finished abutment base, see illustration below.
The finished base was usually made of precious alloys, such as gold-platinum alloy, and was very expensive, even considering that precious metal prices used to be somewhat lower.
At first, it was the only material option to which the body of an individualized abutment could be fused.
Then cobalt-chromium alloys appeared, but precious alloys were the gold standard.
The dental technician formed the desired profile and volume of the future abutment from plastic and wax. A refractory medium of special clay was formed around the wax mold. Further into the mold poured molten metal vaporized the wax or ashless plastic, occupied its volume, and the result was an individual abutment. It was polished, placed in the jaw model and a crown was formed.
Although many jobs performed in the first decade of the Century with such abutments still work, practicing dentists stopped using precious alloys because of the very high price.
So, doctors tried to perform work on stock abutments, while researchers tested ideas and looked for new possibilities. For a long time, cement fixation was considered the gold standard.
Everything would have been fine if there had not been an unhealthy buzz about the fact that cement-retained restorations have a lot of biological complications, such as peri-implantitis.
It all started with a paper published in 2012.
A team of experts analyzed their own very well-loaded practice. Among the many cases, they found a very interesting pattern:
There are far more biological complications on cement-retained crowns. They compared all the clinical cases on cement-retained and screw-retained crowns. It turned out that there were more cases of peri-implantitis on cement-retained crowns, and that’s an interesting pattern.
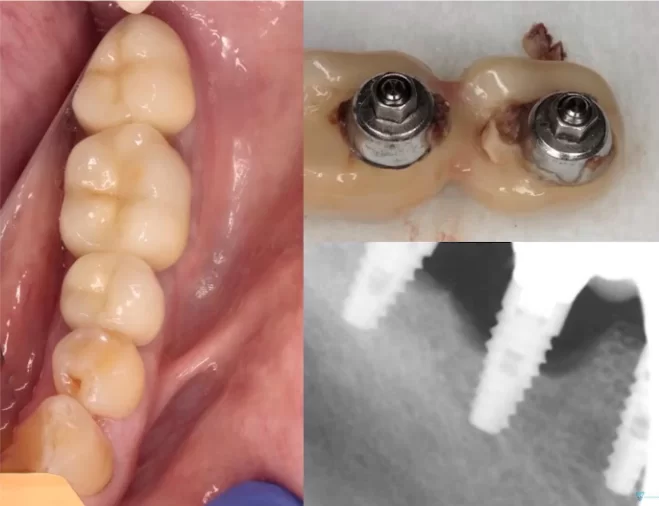
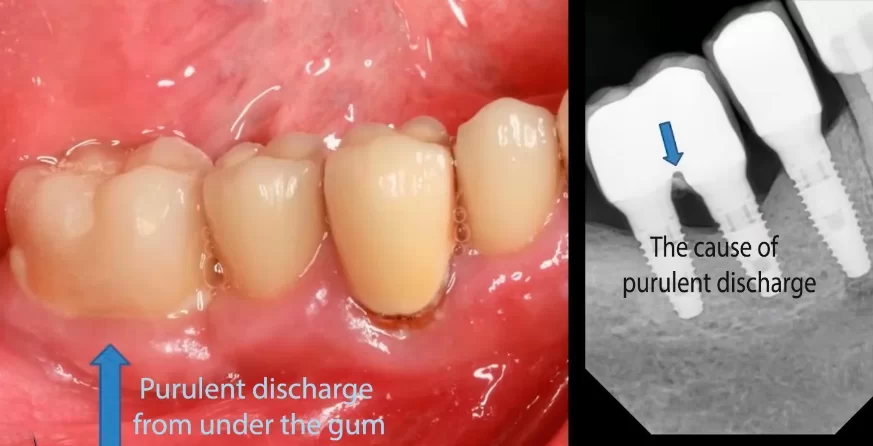
Inflammation and suppuration in the area of cement-retained restorations.
Then they analyzed what this was related to. The sample was quite large. They examined almost all of their patients who agreed to come. They performed revision of all patients and found that, even where there were no biological changes, there were cement residues in peri-implant tissues.
The specialists then analyzed this information and the history of each patient at the time of treatment. They made some very interesting conclusions:
“Within the limitations of this study, we can conclude that peri-implantitis may be associated with cement residues in the peri-implant tissues, especially in patients with existing periodontitis.
Cement residues in patients without a history of periodontitis may cause a less severe course of peri-implantitis or may not predispose to infection at all. Cement residues should be considered as an additional predisposing factor in the development of chronic peri-implantitis.
Finally, screw-retained restorations may be considered as an option of choice in patients with periodontal status.”
When this paper was published, the justified and not-so-justified persecution of cement-retained restorations began. Suddenly, other publications by reputable specialists began to appear, where they confirmed that clinical base checks showed the same results. By 2013-14 there were many such publications. Dr. Wittneben’s presentation at the 2013 ITI Bern Conciliation Conference can be considered the landmark publication of its kind.
This is a very high quality paper. Moreover, the report of Dr. Wittneben’s group formed the basis for the recommendations that were included in Volume 8 of the ITI Treatment Guide – Biological and Technical Complications of Implant Treatment.
Let’s take a look at the findings of Dr. Wittneben’s systematic review published in 2014.
“The five-year survival rate of screw-retained restorations is similar to that of cement-retained restorations.”
That is, the conclusion is completely consistent with Dr. Salvi’s 2008 paper that we mentioned earlier in this article. That is, it cannot be argued that one fixation option is worse than the other.
These, however, aren’t the only findings that were published. This is what else they found:
“The overall incidence of technical complications was statistically significantly higher in cemented restorations.
Technical complications in the form of ceramic fractures or chips were significantly more frequent in screw-retained restorations compared to cement-retained restorations (most likely due to the weakening of the structure due to the screw shaft).
Complications in the form of loosening of abutment retention were more frequently observed in cemented restorations.
The other technical complications such as abutment fracture, framework fracture, implant fracture or screw fracture were statistically on the same level.”
It is worth noting that loosening of the abutment fixation in cement restorations is the most serious of this list of complications because it is almost impossible to remove the restoration without destroying it. If the screw fixing the abutment is loose, the entire restoration will have to be redone.
With screw retention there is no such problem, because the restoration is easily removable. You can remove, replace or tighten the screw and put the restoration back in.
That said, screw-retained restorations are more likely to chip. There is an explanation for this. Screw-retained crowns have holes, usually in the center of the occlusal surface.
This weakens the entire structure. Although this reason is still more in the field of conjecture, it explains why the screw fixation gives more chipping.
This problem has been partially solved by using tapered rosen screws, which distribute the load more evenly and make it possible to do without titanium sleeves inside the restoration. This means that the thickness of the zirconia is greater, which reduces the likelihood of chipping and fracture of the restoration. However, at the time of writing this article, no qualitative studies have been conducted on how much less likely chipping is with tapered screws.
Let’s break down the findings on biological complications from Dr. Wittneben’s paper.
“The overall incidence of biological complications was significantly higher in cement-retained restorations compared to screw-retained restorations.
Festering and fistula were statistically significantly more common in cement-retained restorations. Other biological complications such as bone loss greater than 2 mm, peri-implantitis, peri-implant mucositis, recession, and implant loss were not statistically different between the 2 fixation types.”
This is a very interesting and definitive conclusion and recommendation for practitioners:
“Given the risks associated with the use of cemented restorations, as well as the limited opportunities for re-interventions after final cementation, it seems reasonable to recommend and favor screw-retained restorations.”
It seems that the conflict is resolved, and screw retention is better, but screw retention is often difficult to realize. This is why:
The implant has to stand in an ideal position, so that the screw shaft comes out in the center of the crown and the axis is directed clearly on the antagonist teeth. How was this to be realized in 2014, if even today having computer models of jaws and individual surgical templates, it is not always possible to place the implant in the ideal prosthetic position? Moreover, sometimes it is simply not advisable to place “perfectly”. It is better to place the implant at an angle and avoid bone augmentation surgery.
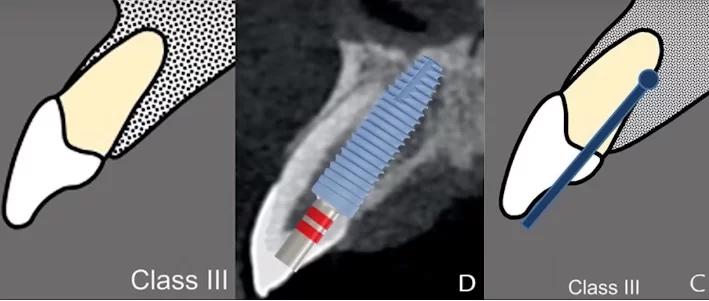
Drilling in the apical direction, parallel to the tooth axis and with the drill axis offset palatally – the screw shaft would come out on the tooth edge, so it is necessary to place a crown on cement fixation
Dogmatic opinions that this is better and that is worse limit specialists. In each case, you need to solve multifactorial problems. Medicine is often similar to art.
The fact remains. All the findings of Dr. Wittneben’s group and what Dr. Linkavicius wrote about earlier are facts.
Cement contact with gingival cuff tissue is a risk factor. There is always cement there, and the fact that not all patients develop peri-implantitis on cement fixation does not mean that all of the cement has been cleared. It’s just that if the patient has an initially healthy periodontium, even contact with the cement will not cause any problems.
If, however, the patient has a history of periodontitis, then cement, even in a very small amount, will cause a reaction in the form of aggressive peri-implantitis, in the appearance of a fistula, suppuration, etc.
That’s why there was a movement against cement. At the same conciliation conference in Bern in 2013, several other conclusions were reached that set the stage.
“High survival rates can be achieved with fixed implant-supported prostheses with both cemented and screw fixation. Failure and complications cannot be avoided when choosing the type of prosthesis fixation.”
After the first reconciling conclusion, the controversy over cement types is also over:
“Based on the literature reviewed, the type of cement used does not affect the failure rate of cement-retained prostheses.”
A small addition from a practicing dentist: all cements work except temporary denture cements, or, as they are called, temporary cements.
They either do not come off when you need them, or they lose adhesion at the worst possible time. Especially difficult situations occur when your patient is in another city or abroad and the restoration has fallen off.
This is an important statement:
“Technical complications occurred in both cement-retained and screw-retained prostheses (estimated annual event rate of up to 10%). In the pooled data, cemented prostheses showed a higher rate of technical complications.”
Think about it, up to 10%, and in fact reality shows that yes, stuff happens. Although it’s worth noting that in complications they included everything including ceramic chipping, darkening of the screw shaft filling on the occlusal surface. Most of the complications are easily corrected and some do not affect the success of the restoration, nevertheless even the slightest deviations from the ideal were taken into account.
If we categorize the complications by type, then:
“Screw-retained dentures have a higher rate of ceramic chipping than cement-retained dentures”
Today, this is no longer a relevant problem because metal-ceramics are not used as often anymore, giving way to solid zirconia dentures that are much less prone to chipping.
One more statement from Dr. Wittneben’s work:
“Biologic complications are found in both cement-retained and screw-retained prostheses (approximate annual event rate of up to 7%). Cement-retained prostheses show a higher rate of fistula formation and suppuration.”
Those are disappointing statistics. Although screw fixation has some advantages in most comparisons, it cannot be said that screw fixation will avoid all problems and complications.
A special edition has been published as a result of this conciliation conference, and we are particularly interested in the treatment recommendations:
Based on the data from this review, it is not possible to make a universal recommendation on the choice of cement or screw fixation.
However, in a clinical situation that offers a choice of prosthetic fixation type, the following recommendations can be made.
Cement retention may be recommended:
- For short-extended dentures with crown margins at or above gingival level. The procedure for removal of cement residue is straightforward in these settings.
- To improve aesthetics when the screw shaft is passed transocclusively or when the implant is misaligned.
- When an intact masticatory surface is desired. In the case of screw fixation, the screw shafts will be covered with composite on the masticatory surface.
- To reduce the initial cost of treatment.
- It is further recommended that the clinician understand that the procedures associated with cement-retained implant-supported crowns are not simple and should be performed with great care.
Screw fixation can be recommended.
- In conditions of minimal interocclusal space, screw retention has been the number one indication from the beginning of screw retention until now.
- To avoid the possibility of excess cement escaping into the tissue (this is especially important if the edge of the denture is placed submucosally, as it has been shown that it is more difficult to completely remove residual cement from the margins if the box edge is placed more than 1.5 mm submucosally). This is where we would recommend screw retention if the crown margin is more than 0.5 mm below the gingival level, even at 1 mm, it is very difficult to remove cement residue.
- When the possibility of revision of the crown is important. This is also a very important point, the possibility of removing the prosthesis is one of the key advantages of screw retention.
- In the aesthetic zone, to facilitate contouring of the tissues in the zenith and transition zone (eruption profile).
- For screw retention, it is recommended that the implant be placed in the orthopedically correct position.
These are very good recommendations, you can even take a screenshot and return to them periodically. Despite the fact that ten years have passed , these recommendations are still relevant.
Real cases and practical recommendations for both screw and cement fixation
Let’s look at a few real clinical cases to see where the advantages of screw-retained or cement-retained prostheses are realized.
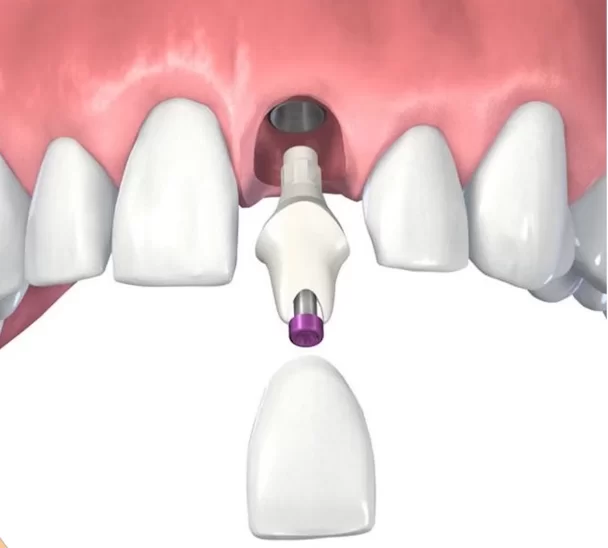
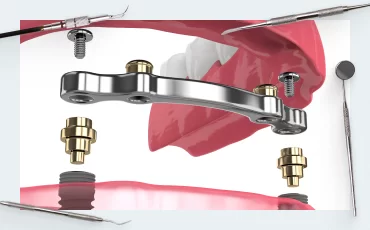
As a reminder, screws and cement are present in one way or another in both types of retention. Only in the case of cement retention, the abutment is first fixed in the implant and then a crown or a more extensive prosthesis with multiple abutments is cemented onto it.
As the fixation takes place in the mouth, it is difficult to remove excess cement.
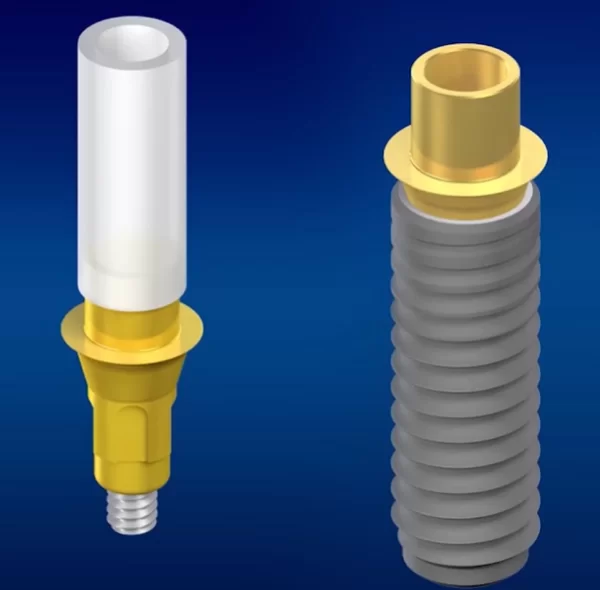
In the case of screw fixation, there are two cases:
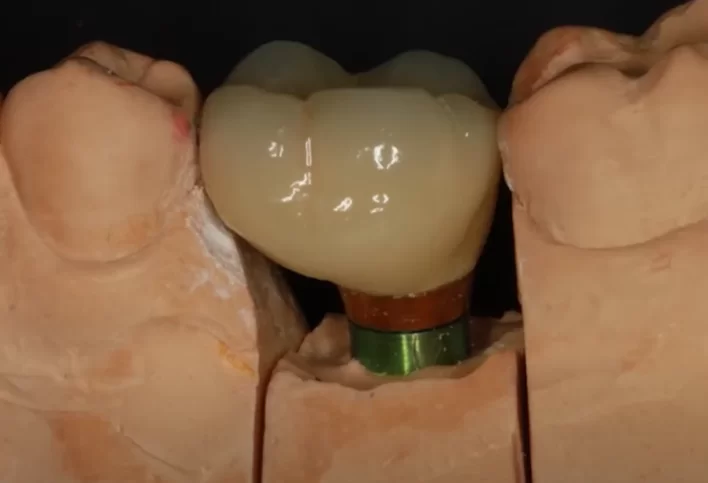
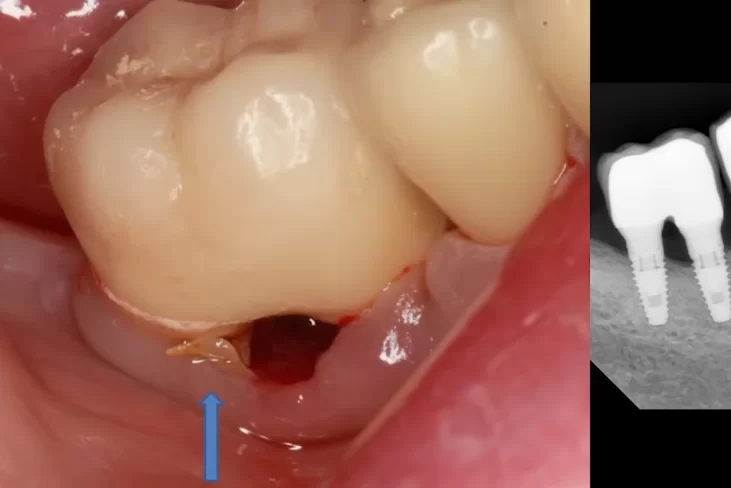
- The abutments are connected to the prosthesis with the same cement, but outside the patient’s mouth, and are placed in the implant already cleaned of cement residue. This is how single defects are prosthetized.
.
. - For multiple restorations, special multi-unit abutments are used, which are placed immediately after integration of the implants and are not removed for the entire service life of the prosthesis. The prosthesis is designed and fixed at the level of the already installed multi-unit abutments. Special sleeves are cemented into the prosthesis, which are in contact with the interface of the multi-unit abutment. However, it is also possible to fix the prosthesis without sleeves, in which case no cement is used at any stage. More information on the restoration of multiple defects will be given in the next article in the series on screw and cement retention of dentures.
In dentistry, as in other fields of science, we apply the principle of Occam’s razor, i.e. the simpler the design, the better.
In this case, when the abutment and the screw-retained crown form a single unit, and have an optimal eruption profile without complicated manufacturing of individual abutments, it is simpler and in many cases better.
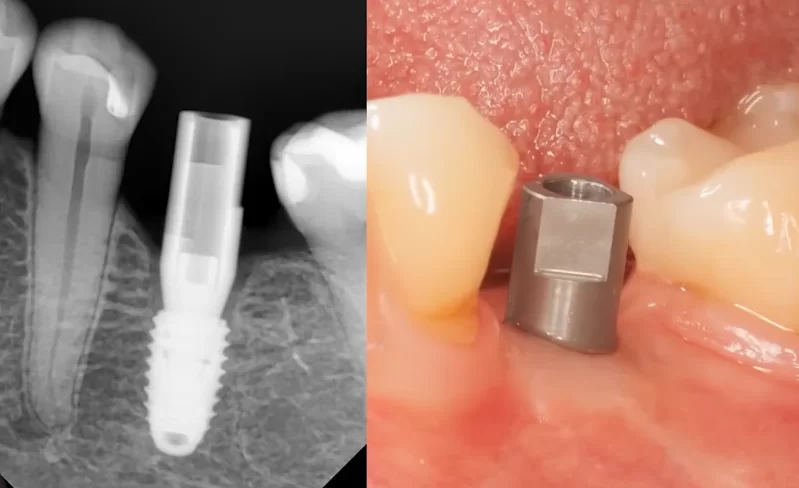
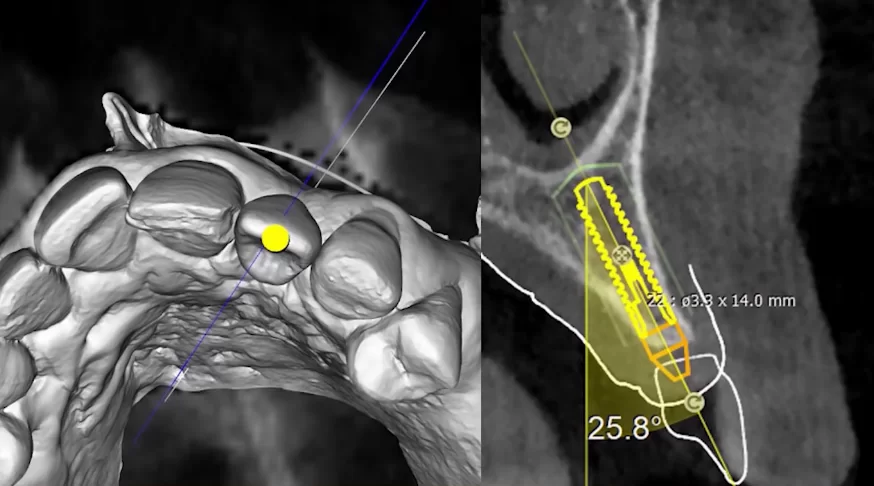
Let’s look at a specific clinical case. The implant is placed in a fairly good position – almost perfectly.
Next, a standard abutment has been placed, and we can see that the potential bonding line for the crown is quite deep.
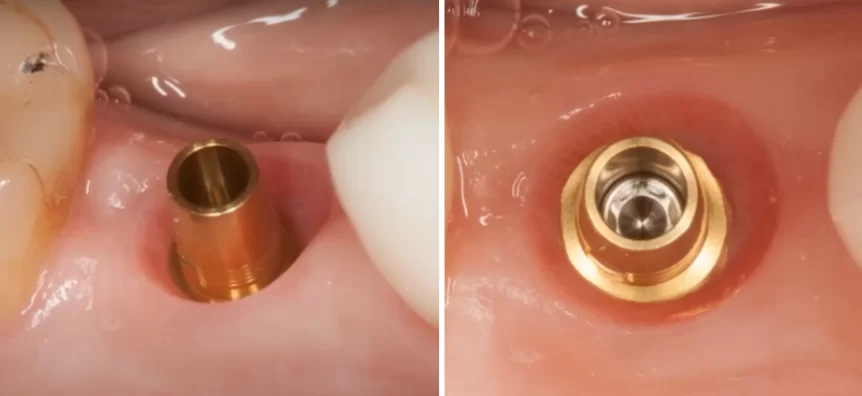
The line between the crown and the abutment base is more than 1. 5 mm deeper than the soft tissue level
This case is not suitable for cement fixation.IIf you try to glue a crown here, it will fail. There is no way to remove the excess cement except bysurgical intervention, but it is a very bad idea to destroy such a good gingival cuff.
Therefore, in this case we use a titanium abutment and a digitally milled crown.
The crown is glued to the abutment in the laboratory or in the clinic, the main thing is that this operation takes place outside the patient’s mouth.
The only difference with cement fixation in this case is where the bonding takes place. Ant excess cement can be removed in the laboratory.
In this case, the implant is in the ideal position. Screw retention in this case is easier and cheaper than manufacturing an individual abutment and crown for cement retention.
Now let’s return to one of the disadvantages of screw retention, which is the darkening of the composite where the screw shafts are located on the occlusal surface of the prosthesis. The pictures below are an example of what this looks like.
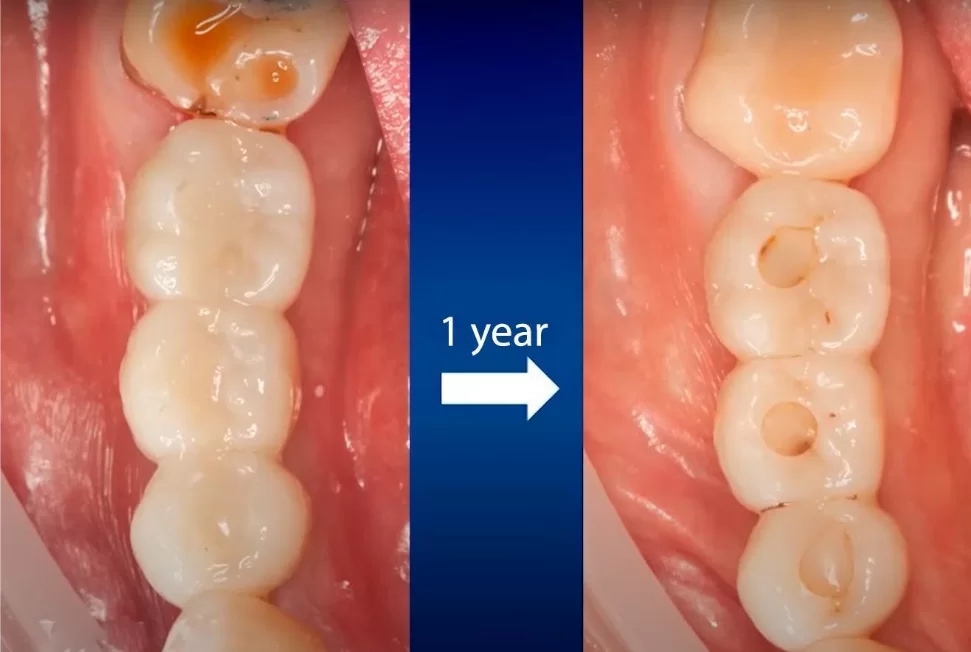
Darkening of the screw shafts of screw-retained dentures one year after the installation of the denture
Is this a terrible complication? It is not a problem for most patients. At the very least, if a patient comes in, they change these plugs and that’s it. Sometimes it happens that the composite plug falls out, but the patient comes to the mine closed with a new composite and he left satisfied. Dentists always have the opportunity to remove the restoration, clean, or treat soft tissues and put it back on. This is a huge advantage that compensates for such a minor defect as discoloration.
Keep in mind that there is a category of patients, most often women, who are prone to dysmorphophobia. These patients may have an acute aversion to restorations with even the smallest defect. One should be extremely careful with such patients so that you do not have to redo restorations under the threat of lawsuits.
Let’s look at another not-so-obvious disadvantage of screw retention. As an example, let’s take a clinical case with a sufficiently deep implant.
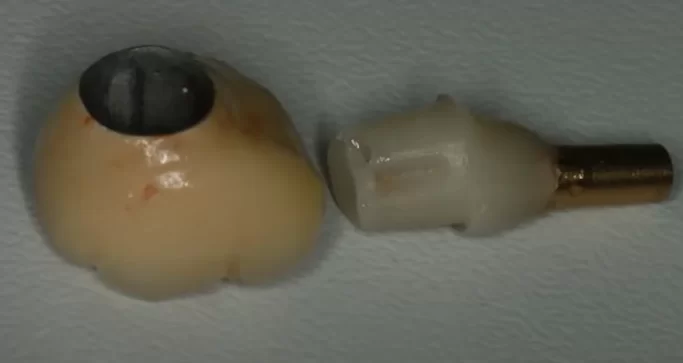
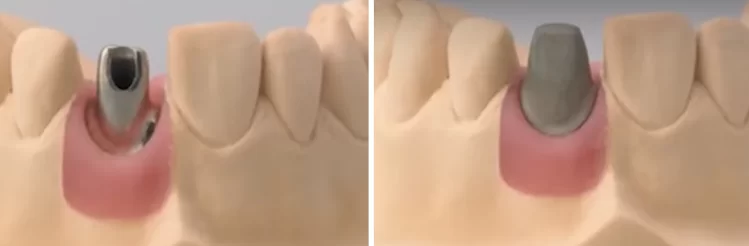
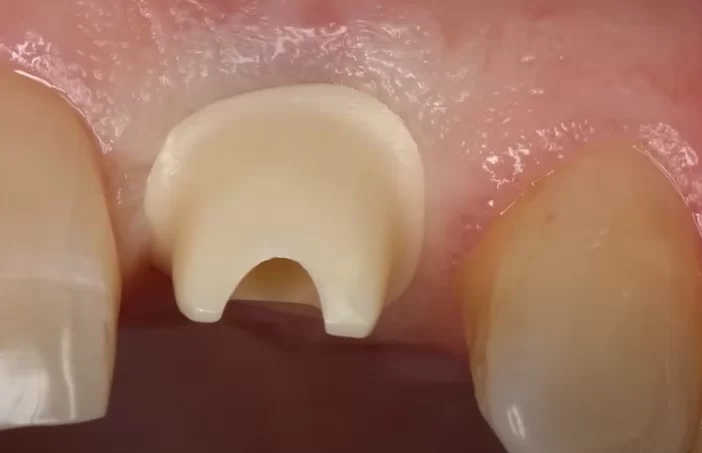
Next, we took a titanium abutment, prepared it, then milled a zirconium dioxide crown, glued and treated the surface that will be in contact with the gingiva, as recommended in the article on whether to polish the surface of abutments.
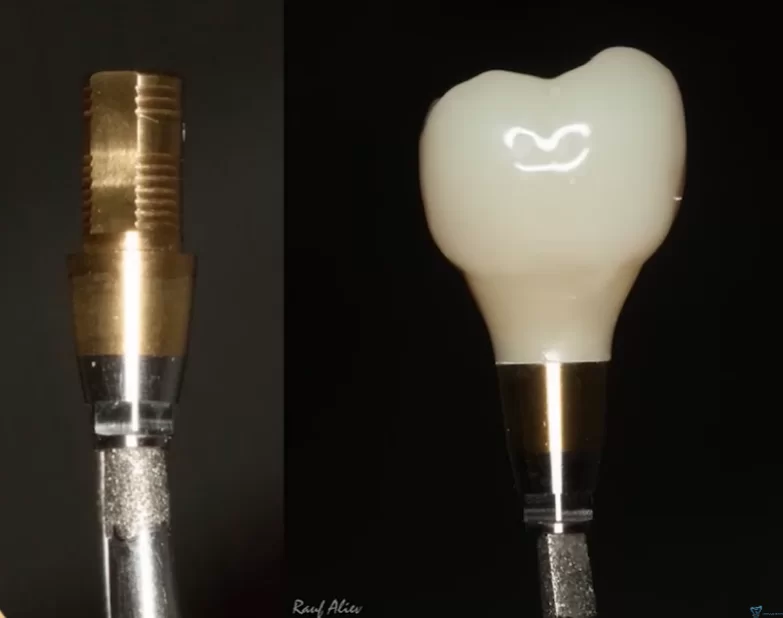
Abutment with anti-rotation facets and crown with optimal eruption profile for screw-retained single restoration
In other words, all the preparatory work was completed perfectly, but during the retention phase of the crown, the abutment was difficult to fit into the planned position. It took about 45 minutes between the two pictures below, which is a very long time. In addition, five more aiming shots with intermediate steps were taken because the abutment with the crown did not sit in the desired position.
Difficulties are related to the fact that the implant platform is deep, the crown touches the neighboring teeth, plus there is the task of not injuring the gum during insertion. All these factors together make the work very difficult. This should be taken into account when choosing the type of fixation, cement fixation on a customized abutment would take three to five minutes, not an hour as in this case. In the case of a double-implant-supported bridge, it would be much more difficult to fit the restoration into place. This is why multi-unit abutments are used for multiple screw-retained restorations, which are fitted independently of each other and the prosthesis is easily fitted with a perfect passive fit.
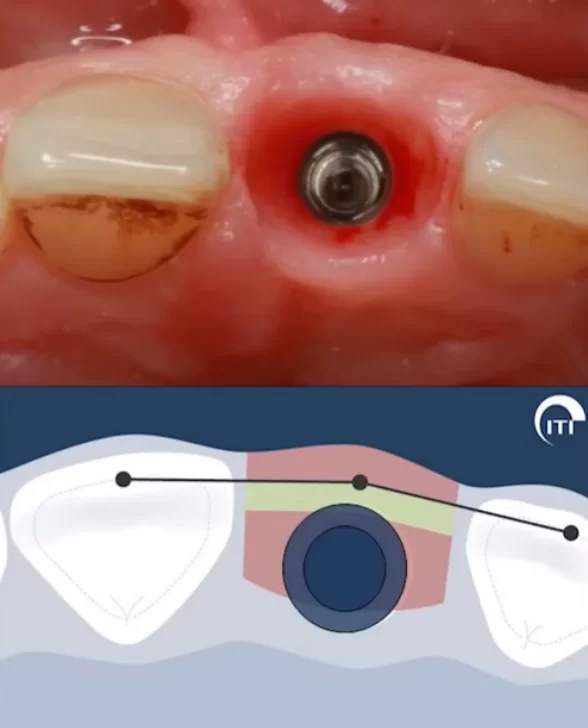
Here is another interesting observation. From the above recommendations, we know that screw retention requires correct implant positioning. The illustration below is well known to specialists, especially as the lower part is from the ITI guide.
The dividing line of the safety zone (green bar), where the implant platform should be, is clearly shown here. This safety zone is determined by the preservation of the vestibular bone wall and sufficient gingival thickness.
It is coincidental that this position of the implant center coincides perfectly with the successful exit of the screw shaft of the restoration. This position of the implant center corresponds to an anatomical formation called a cingulum. This is a protuberance on the inner part of the central incisors and canines, which can be seen in the photo above. It is clearly expressed in young people. With age, the protrusion is erased.
The cingulum is the place where the screw shaft should be and, therefore, the center of the implant. Otherwise, you will have an exit of the screw shaft to the incisal surface or to the vestibular part of the restoration. This already implies the fabrication of an individual abutment and cemented restoration. It is now possible to use angled abutments and still bring the screw shaft to the lingual side of the restoration. That is the subject of the next article.
Here we will look at an example of screw fixation on a straight abutment with a good prosthetic position of the implant. There are, however, nuances here as well.
Note the thickness of the crown on the palatal side. The permanent crown, which will be made of zirconium dioxide, will be much thicker in this area. These are also nuances that should be taken into account and warn patients. There is nothing terrible in this. At first the patient will feel that this tooth is slightly thicker than the neighboring ones, but if there are no problems with clamping, the patient will quickly get used to it.
Again, there may be unpleasant questions from some patients. The dentist is correct everywhere, the implant is in the ideal position, all books and guides say that you can and should work with it, but you may face the need to make a restoration with non-standard proportions.
Sometimes you may think that it would be better to slightly incline the implant vestibularly and make a separate abutment and a separate crown, so that you do not have to deal with complaints and remarks.
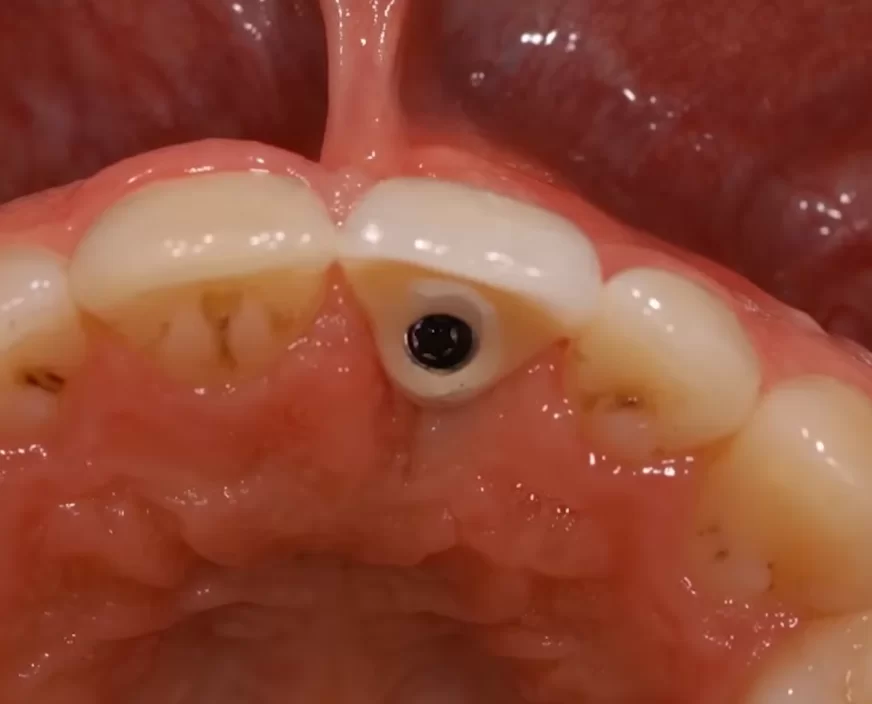
Therefore, let’s consider another case where a decision was made in favor of an individual abutment and cement fixation.
The process of planning the location of the implant and the future crown, taking into account the patient’s bone condition
If you try to move the center of the implant to make a screw fixation, you would have to build up a significant amount of bone tissue. In this case, the center of the implant is on the incisal plane and this is normal, there was also a small augmentation with bone graft on the vestibular side and this was sufficient for the implant to integrate well. Then a customized abutment was made, see image below.
Then the crown is glued onto the already placed abutment and the restoration is ready.
Notice the shape of the abutment, the edge of the restoration is supragingival.
The border between the crown and abutment is above the gingival level – this allows the cement residue to be removed completely
This is the ideal position for cement-retained restorations; in the most extreme case, the crown line can be equigingival.
This is the most important principle. If a customized abutment is already being fabricated, it is not necessary to plunge the edge of the crown deeper. Aesthetically everything will be perfect as it is, but with this positioning of the crown edge we remove all the cement and get a perfectly serviceable restoration.
Even if in this case the edge of the abutment is slightly visible or there is gingival recession, it is not a big deal. The abutment is made of light-colored zirconia and this will have almost no effect on the aesthetics.
Take a look at the picture below of how the crown is fixed. The cement is pressed outwards. Nothing goes into the subgingival tissue, and nothing goes into the peri-implant tissues. This is worth a lot; for the sake of this result, it is worth the effort to fabricate a customized abutment.
Now we can understand one of the main conclusions of this article. Neither screw nor cement fixation saves the dentist from low skills. Moreover, a true master gets brilliant results using both techniques and determines which is better by considering each clinical case individually.
The following case study shows what a dentist’s poor decisions can lead to in the long run.
The patient came in with inflammation and purulent discharge in the area of the paired restoration. The experienced specialist suspected even before the radiographs that the cause of the inflammation was cement residue under the crowns. This is a typical manifestation when purulent discharge is localized like this, while the condition of soft tissues around the neighboring teeth is more or less good.
The suspicions were confirmed, the radiograph showed the presence of a significant amount of cement under the united crowns. Moreover, it was discovered that the patient had once had periodontitis, but had been treated and had implants and crowns placed at another clinic.
Here, the dentist decided to combine the two crowns, that is, he made a common crown for the two implants. This option has a right to exist, but in this case it was a poor choice. Especially if we take into account that the patient has had periodontitis before, and it is initially unrealistic to remove the cement in such a crown design. First of all, the patient’s health should be taken care of, and then the convenience of making and installing the prosthesis. In this case, the dentist did not think about the elementary things of hygiene and maintainability of the restoration.
To solve the problem, it was enough to remove the cement through a simple operation and the patient was immediately relieved.
We have presented several clinical cases to make the point that successful restorations can be made with both cement and screw fixation, as well as problematic and complicated restorations.
And yes, we agree that screw fixation has some undeniable advantages. It’s convenient, it’s simple, and it’s fairly inexpensive. The fact that screw fixation is conditionally removable is a huge advantage for most clinical cases.
However, we have considered several situations when screw fixation is not the best option. For example, when the implant platform is very deep and fitting a crown and abutment will take a lot of time and effort. Or if the restoration is in the area of the front teeth. Sometimes it is better to place the implant in a conditionally orthopedically disadvantageous position and do without significant bone augmentation. The shaft of the screw would, however, extend to the front of the restoration. To avoid this problem, it is better to fabricate a customized abutment and crown for cement retention. Thanks to CAD/CAM technology, customized abutments can be CNC-machined from zirconia or even printed on a 3D printer. This no longer requires the use of precious metals and castings.
We encourage you to expand your capabilities and learn to master both techniques at a high level.Make an informed choice and act in the patient’s best interest in every clinical case.
In the next article, we will continue our comparison of the features and advantages of both types of retention for multiple restorations, and will go into more detail about the retention of multi-unit abutments. Until next time.