What abutment morphology is better for a gingival connection: linear divergent or concave? Randomized controlled trial of CAD/CAM abutments
We have repeatedly mentioned in our blog the importance of the abutment emergence profile for gum health. And now it is believed that the expansion angle of the abutment should not exceed 30°. With this form of abutment, a full-fledged gingival cuff with well-defined papillae is formed. If the expansion angle of the abutment is significantly greater, there is a risk of deformation and gum recession. But the researchers went further and decided to find out what would happen if the abutment neck was made concave and compared the condition of the soft tissues with a group of patients where the abutment neck was simply conical.
We present the results of a randomized controlled trial (RCT) on the effect of concave and linearly divergent CAD/CAM zirconia abutments on peri-implant tissue dynamics and health indicators in the anterior maxilla. The results show that abutment design did not have a significant effect on changes in mucosal zenith, tissue thickness, or peri-implant health outcomes at one year. The original article can be found at Wiley Online Library.
Introduction
The esthetic success of implant restorations largely depends on the architecture of the peri-implant tissues. The transition from a cylindrical implant interface to anatomically contoured clinical crowns requires careful consideration of the morphology of the transmucosal abutment. Previous studies indicate that subtle differences in abutment profiles can influence soft tissue health. However, reliable data from a well-designed RCT on this issue are not yet available.
The purpose of this study was to evaluate the effect of customized zirconia abutments with a concave or linearly divergent transmucosal profile on the health and esthetics of peri-implant tissues in a delayed loading protocol.
Materials and methods
Study design and ethical compliance
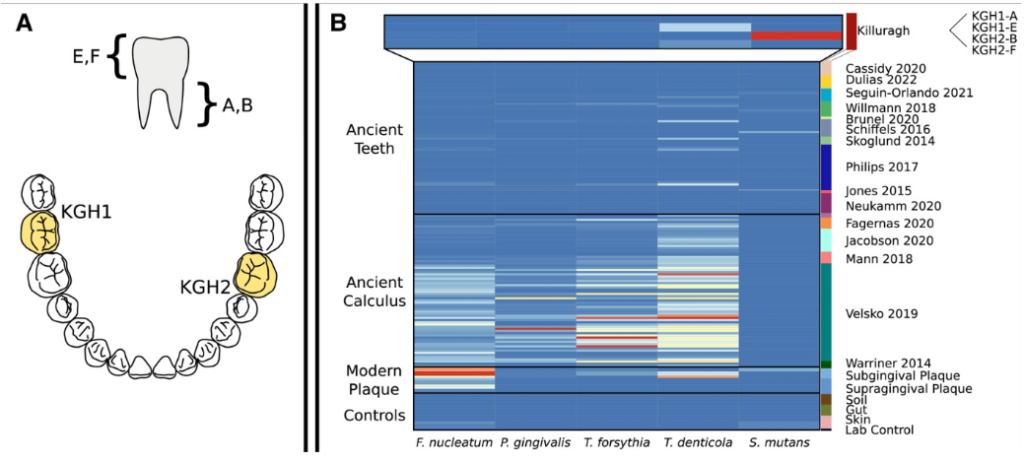
A single-center, two-arm RCT was performed at the University of Iowa in accordance with CONSORT guidelines and ethical standards. 60 patients requiring restoration of the anterior maxilla were randomized into two groups: with concave (experimental group) and linear divergent (control group) abutments.
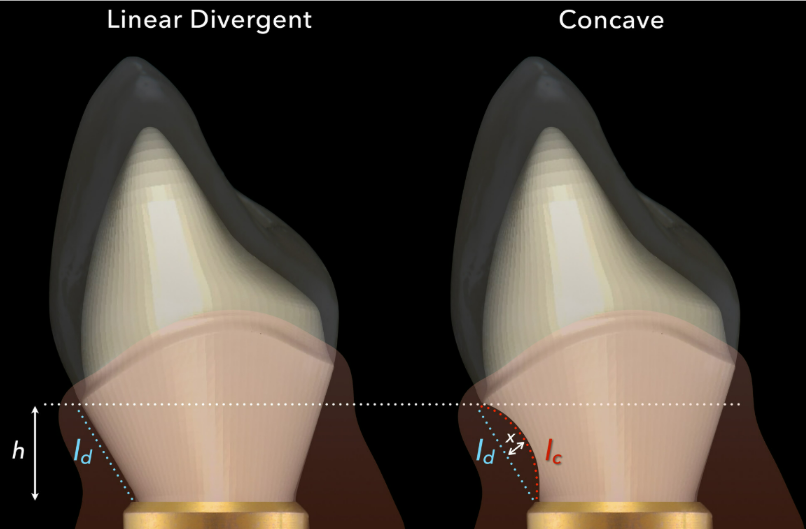
Custom screw-retained CAD/CAM zirconia abutments with either a linear divergent (left) or maximum concave (right) facial emergence profile. Linear (lc–ld) and volumetric (x) differences due to the CAD/CAM abutment design were characterized in relation to peri-implant mucosal outcomes Wiley Online Library / Christopher A. Barwacz / Clinical Oral Implants Research / 2024
Sample size
A minimum sample size of 30 participants per group was calculated to detect a clinically significant difference (1.0 mm) in change in mucosal zenith position with 80% power and a significance level of 5%.
Inclusion and exclusion criteria
Main inclusion criteria: age ≥18 years, stable adjacent teeth, sufficient bone and soft tissue. Patients with systemic diseases affecting healing, smokers, and those unable to attend follow-up appointments were excluded.
Measured parameters
- Main indicator: Changes in the position of the mucosal zenith.
- Secondary indicators: Soft tissue thickness, keratinized mucosa width (KMW), marginal bone level, probing depth, bleeding on probing, plaque index, and modified mucosal index.
Procedures
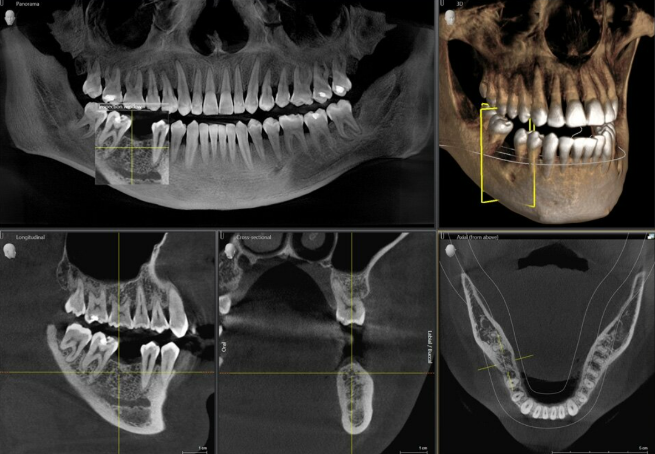
Standard implants, temporary abutments, and custom CAD/CAM abutments were installed. Measurements were taken at baseline, 1, 3, 6, and 12 months.
Results
Participant Demographics
Of the 60 patients, 54 completed the study. Implants were installed in incisors (51.6%), canines (11.7%), and premolars (36.7%). The implant survival rate was 100%, and the restoration success rate was 98.2%.
Main indicator: position of mucosal zenith
At 12 months, there were no significant differences between groups (p=0.853). Significant coronal zenith displacement was observed in both groups (p<0.001).
Secondary indicators
- Soft tissue thickness:
- There were no significant differences between groups (p=0.674) and over time (p=0.144).
- Keratinized mucosa width (KMW):
- Increase in KMW over time in both groups (p<0.001), without intergroup differences (p=0.106).
- Health indicators of peri-implant tissues:
- Bone level: minimal change (≤0.04 mm) with no differences between groups.
- Plaque index and modified mucosal index: increase over time (p=0.044 and p=0.001).
- Probing depth and bleeding: slight increase over time.
Discussion
The results show that transmucosal abutment morphology does not have a significant effect on soft tissue dynamics or peri-implant health outcomes at one year. These data are consistent with previous studies, highlighting the multifactorial nature of the influence on peri-implant tissues.
Clinical significance
- Practical application:
- Both types of abutments provide stable peri-implant results.
- The choice of abutment morphology can be based on esthetic and functional needs.
- Recommendations for practice:
- Integrating surgical precision and personalized prosthetic design.
- Regular programs to maintain the health of peri-implant tissues.
Limitations of the study
The short follow-up period and lack of data on subjective esthetic assessment limit the interpretation of the results. Long-term studies are required.
Conclusion
This study highlights the complexity of factors affecting peri-implant tissues and the need for an individualized approach in implant treatment. Although there is no significant impact of abutment design on soft tissue, this study provides insight into the formation of the gingival cuff and gives dentists more freedom to design customized abutments based on both functional and esthetic considerations.
Source
Wiley Online Library – Effect of CAD/CAM Abutment Morphology on the Outcomes of Implant Therapy: A Randomized Controlled Trial – December 6, 2024