Intensive treatment of type 2 diabetes – leads to reduced gum inflammation: results of a recent study
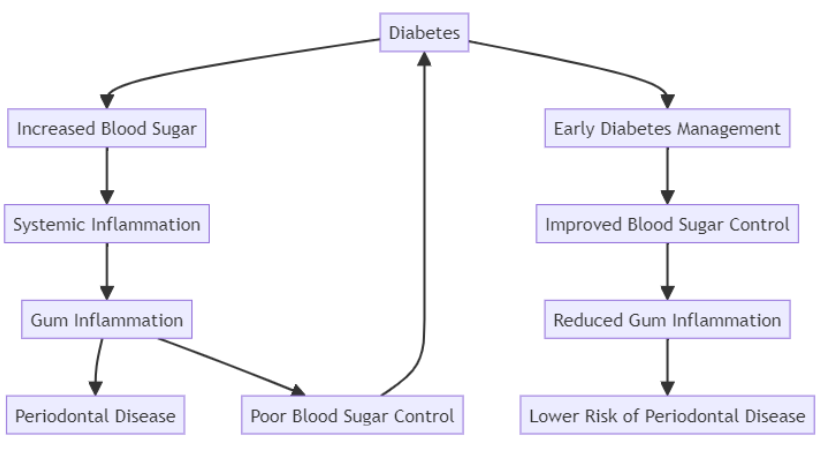
Understanding the Connection Between Diabetes and Periodontal Disease
Diabetes, particularly type 2 diabetes, has long been associated with an increased risk of periodontal disease. This interrelationship is well documented: elevated blood glucose levels can lead to inflammation throughout the body, including the gums, increasing the risk of gum disease.Recent research by experts at Osaka University published in Diabetes, Obesity and Metabolism emphasizes that improving glycemic control can directly impact periodontal health, making the link between diabetes management and gum disease more important than ever.
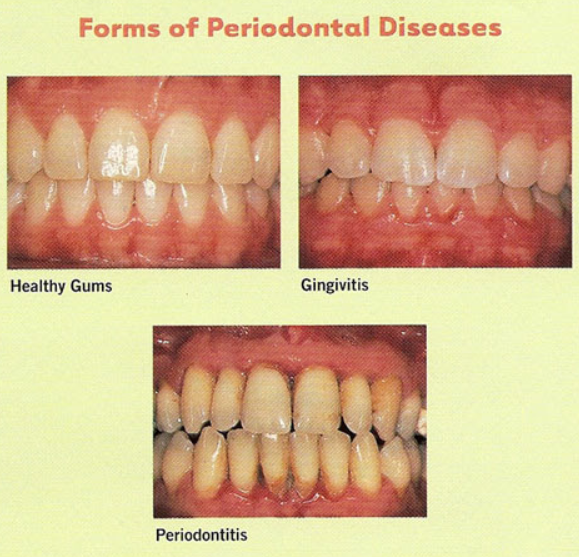
Periodontal Disease as a Diabetes Complication
Periodontal disease is a chronic inflammatory condition affecting the tissues surrounding the teeth. It progresses in stages, starting as gingivitis and evolving into more severe forms of periodontitis if untreated. For individuals with diabetes, the severity of periodontal disease is often exacerbated due to compromised blood sugar levels, which fuel inflammation. In turn, this inflammation can worsen blood sugar control, creating a vicious cycle between diabetes and gum health.
The Role of PISA in Measuring Periodontal Inflammation
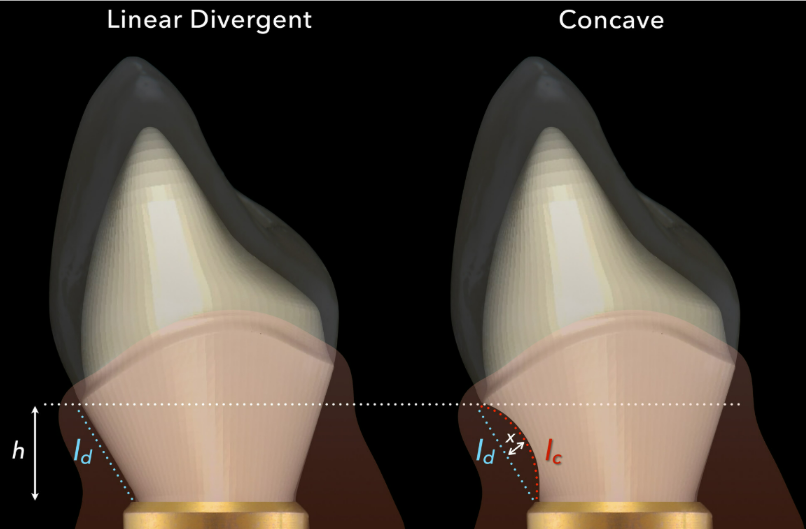
Periodontal Inflamed Surface Area (PISA) is a critical metric used to assess the extent of gum inflammation. It measures the surface area of bleeding gums, offering a quantifiable indicator of periodontal health. Elevated PISA levels reflect more severe inflammation, often correlated with poor blood sugar control in diabetes patients. By tracking PISA, researchers can better understand how systemic conditions, like diabetes, influence periodontal outcomes.
Intensive Diabetes Treatment: A New Approach to Gum Health
Recent groundbreaking research has demonstrated that intensive diabetes treatment—particularly under hospitalization—can significantly reduce not only blood sugar levels but also periodontal inflammation. A study published in Diabetes, Obesity and Metabolism revealed that two weeks of intensive diabetes treatment for type 2 diabetes patients led to measurable improvements in both glycemic control and PISA scores, even without direct periodontal interventions.
Study Overview: Diabetes and Periodontal Disease Management
The study conducted by a team from Osaka University involved 29 patients with type 2 diabetes. These patients underwent two weeks of intensive diabetes treatment, with a primary focus on stabilizing blood sugar levels. No dental treatments or periodontal interventions were provided during the study period. The results were compelling:
- Improved Blood Sugar Control: Patients showed significant reductions in glycoalbumin, a marker for long-term blood glucose levels.
- Reduced PISA Scores: Periodontal inflammation, as measured by PISA, decreased notably, demonstrating that better blood sugar control positively impacts gum health.
These findings confirm that controlling diabetes early can mitigate periodontal inflammation, providing a new pathway to manage both conditions simultaneously.
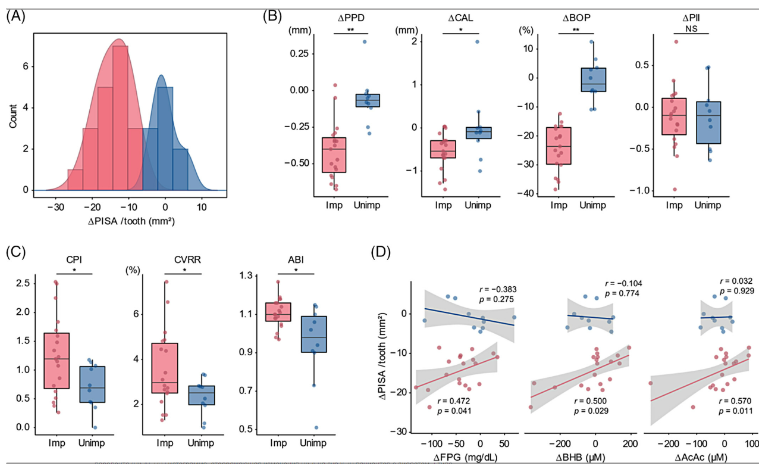
Clinical characteristics of the periodontal inflamed surface area (PISA)-improved and non-improved groups. (A) Histogram displaying the changes in PISA per tooth in 29 patients with type 2 diabetes revealed a bimodal distribution, dividing the patients into the PISA-improved (< −5.0 mm2) and non-improved (≥ −5.0 mm2) groups. (B) Differences in the changes in the periodontal indicators between the PISA-improved and non-improved groups *p < 0.05, **p < 0.01. (C) Significant differences can be observed in the values for clinical indicators before glycaemic control treatment between the PISA-improved and non-improved groups. *p < 0.05. (D) Positive correlations can be observed between the changes in PISA per tooth and systemic indicators in the PISA-improved group. ABI, ankle brachial pressure index; AcAc, acetoacetic acid; BHB, beta-hydroxybutyrate; BOP, bleeding on probing; CAL, clinical attachment level; CPI, C-peptide index; CVRR, coefficient of variation of R-R interval; FPG, fasting plasma glucose; Imp, PISA-improved group; NS, not significant; PlI, plaque index; PISA/tooth, periodontal inflamed surface area/number of residual teeth; PPD, probing pocket depth; Unimp, PISA non-improved group.
Key Findings: Insulin Secretion and Complication Severity Influence Outcomes
Further analysis of the study’s results revealed that patients with better insulin secretion capacity and fewer diabetes complications showed the most significant improvements in periodontal inflammation. Pre-treatment C-peptide levels, which indicate the body’s ability to produce insulin, were higher in patients with greater PISA reductions. This suggests that patients with residual insulin production can respond more effectively to intensive diabetes treatment, benefiting both their blood sugar levels and periodontal health.
Impact of Diabetic Complications on Gum Disease
Patients with severe diabetic complications, such as neuropathy and peripheral vascular disorders, exhibited less improvement in PISA scores. This correlation underscores the importance of early diabetes management to prevent the onset of complications that could hinder the ability to improve periodontal health later.
The Importance of Early Intervention
The research strongly supports early intervention in diabetes care to manage and prevent periodontal disease. The sooner diabetes is controlled, the less likely patients are to experience severe gum inflammation. This opens the door to a more integrated approach to healthcare, where medical and dental professionals collaborate to address the systemic effects of diabetes on periodontal health.
Collaborative Care: A Holistic Approach to Diabetes and Gum Disease
The results of this study emphasize the need for a collaborative approach between healthcare providers. By combining diabetes management with regular dental care, patients can achieve better outcomes in both areas. Early diagnosis and treatment of diabetes, coupled with proactive periodontal care, can prevent the escalation of complications that make gum disease harder to treat.
Long-Term Benefits of Intensive Diabetes Treatment for Periodontal Health
Long-term management of diabetes is crucial for maintaining periodontal health. While the study focused on short-term, intensive treatment, the findings highlight the broader implications for chronic care. Continuous monitoring of blood sugar levels, alongside routine dental check-ups, ensures that patients remain in control of both their diabetes and gum health. Preventing the progression of periodontal disease not only protects oral health but also contributes to better glycemic control, reducing the risk of further complications.
Diagram: The Interrelationship Between Diabetes and Periodontal Disease
Conclusion: Prioritizing Early Treatment for Optimal Results
The relationship between diabetes and periodontal disease is well-established, but recent research sheds light on the importance of early and intensive diabetes management for improving gum health. By stabilizing blood sugar levels, patients can reduce periodontal inflammation and avoid the severe complications of both conditions. The key takeaway from these findings is that addressing diabetes holistically, in conjunction with dental care, offers a promising strategy for enhancing overall health and quality of life.
Incorporating intensive diabetes treatment from the onset, alongside continuous periodontal monitoring, will not only improve patients’ gum health but also support better diabetes control, creating a win-win scenario for long-term wellness.
Sources
- ScienceDaily – Getting to the root of the problem: Intensive diabetes treatment reduces gum disease inflammation – September 17, 2024
- Diabetes Obesity and Metabolism – Periodontal tissue susceptibility to glycaemic control in type 2 diabetes – August 14, 2024