Understanding the Link Between Gum Disease and Alzheimer’s: A Breakthrough Study
In recent years, researchers have been uncovering intriguing connections between oral health and systemic diseases, challenging the conventional belief that oral disease is limited to its impact on the mouth. One area that has gained significant attention is the link between gum disease and Alzheimer’s disease. Groundbreaking research conducted by the Forsyth Institute in collaboration with Boston University has shed new light on how periodontal disease, commonly known as gum disease, may be associated with the formation of amyloid plaque, a key hallmark of Alzheimer’s disease. This comprehensive study, titled “Microglial Cell Response to Experimental Periodontal Disease,” published in the Journal of Neuroinflammation, delves into the fascinating world of oral bacteria’s potential role in cognitive decline and neuroinflammation.
Contents
The Intriguing Discovery
The research team, led by Dr. Alpdogan Kantarci, a distinguished senior member of staff at Forsyth Institute, sought to investigate whether oral bacteria could cause changes in brain cells, particularly microglial cells. These specialized white blood cells are responsible for digesting amyloid plaque and play a crucial role in defending the brain from harmful substances. Previous studies had already established that inflammation linked to gum disease can trigger an inflammatory response in the brain. This led the team to explore the potential impact of oral bacteria on microglial cells.
Microglial Cells and Their Response
In their groundbreaking study, the researchers exposed microglial cells to oral bacteria to observe their reaction. To their surprise, they found that when these cells were exposed to oral bacteria, they became overstimulated and their normal function of digesting amyloid plaque was disrupted. Essentially, the microglial cells became “obese,” losing their ability to efficiently process plaque formations. This crucial finding suggests that gum disease can indeed influence brain health by interfering with the vital role of microglial cells in clearing amyloid plaque.
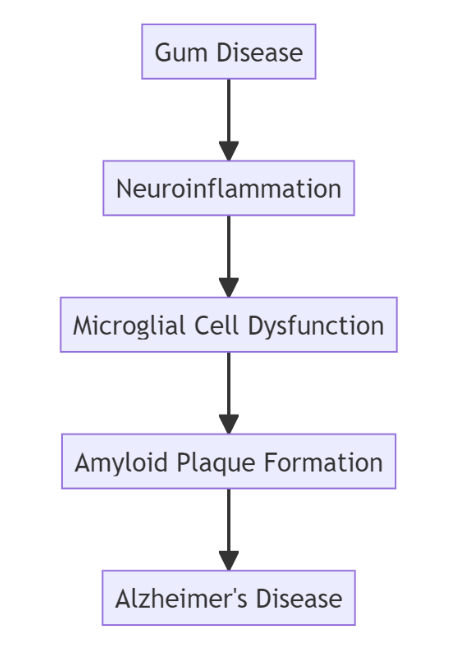
Diagram (Markdown Mermaid Syntax)
In this diagram, we illustrate the chain of events connecting gum disease to Alzheimer’s disease. Gum disease can lead to neuroinflammation, which, in turn, affects microglial cells’ normal function and leads to the formation of amyloid plaques. The presence of these plaques is a significant factor in the development of Alzheimer’s disease.
(Note: The diagram is a visual representation and does not include all potential factors and complexities of the relationship between gum disease and Alzheimer’s.)
Unraveling the Mechanism
To better understand the mechanism underlying the link between gum disease and Alzheimer’s, the scientists used a unique approach. They utilized mouse oral bacteria to induce gum disease in lab mice, enabling them to track the progression of periodontal disease in these mice and observe its effects on the brain. Confirming the hypothesis, the researchers discovered that the bacteria from the mouth had traveled to the brain.
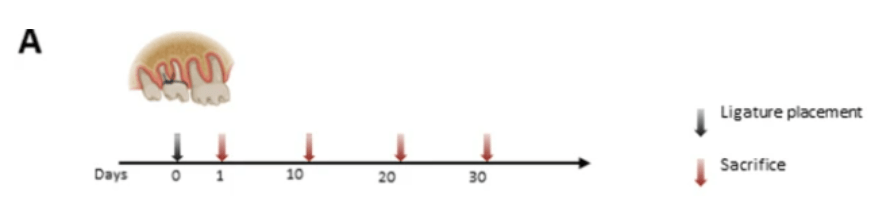
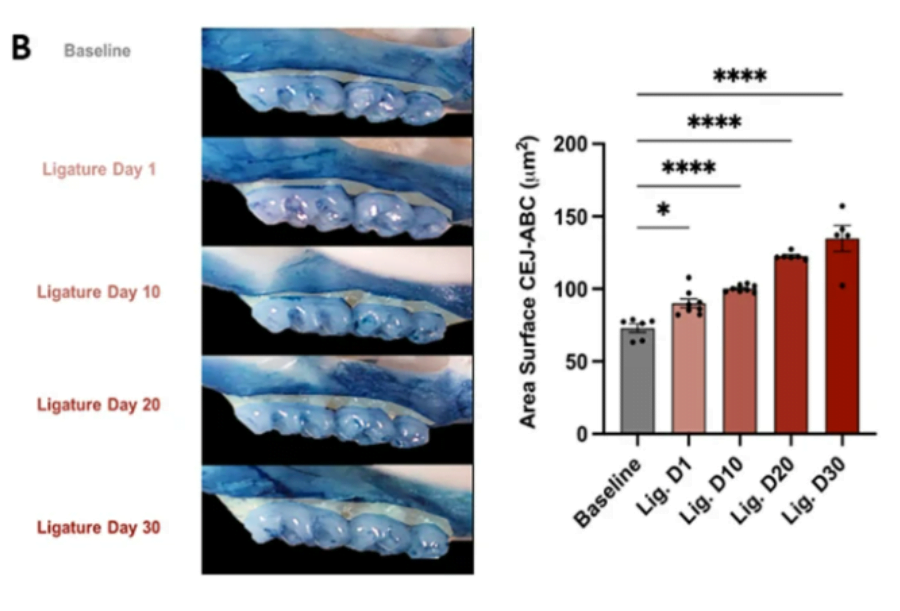
Alveolar bone resorption and mRNA expression levels of RANKL and OPG in periodontal tissues of mice with ligature-induced experimental periodontal disease. A In vivo experimental design (n = 36, 7–8 mice per group). The baseline group was left untreated, and four groups had ligatures around maxillary right and left second molars for different timepoints corresponding to 1,10, 20, and 30 days and then sacrificed. Black arrow: placement of ligatures. Red arrows: sacrifice. B Left: representative images of the left maxillae from each experimental group (buccal view). Right: quantification of the area between the alveolar bone crest level and the cementoenamel junction of the three maxillary molars, using Fiji software (ImageJ). C Levels of mRNA expression of proteins involved in periodontal tissue metabolism RANKL and OPG. The right and left gingival tissue of each mouse were pooled together and represented one sample. Baseline: mice without ligature placement. Lig. D1, D10, D20, and D30: mice with ligature placed for different timepoints corresponding to 1,10, 20, and 30 days, respectively. (n = 36, 7–8/group, Mean ± SEM, ANOVA, *p < 0.05, ****p < 0.0001)
The Impact on Neuroinflammation
With periodontal disease established in the lab mice, the researchers then isolated the brain microglial cells and exposed them to the same oral bacteria. The exposure triggered the microglial cells, resulting in neuroinflammation. This neuroinflammation disrupted the normal function of microglial cells in dealing with amyloid plaques, thereby potentially contributing to the progression of Alzheimer’s disease.
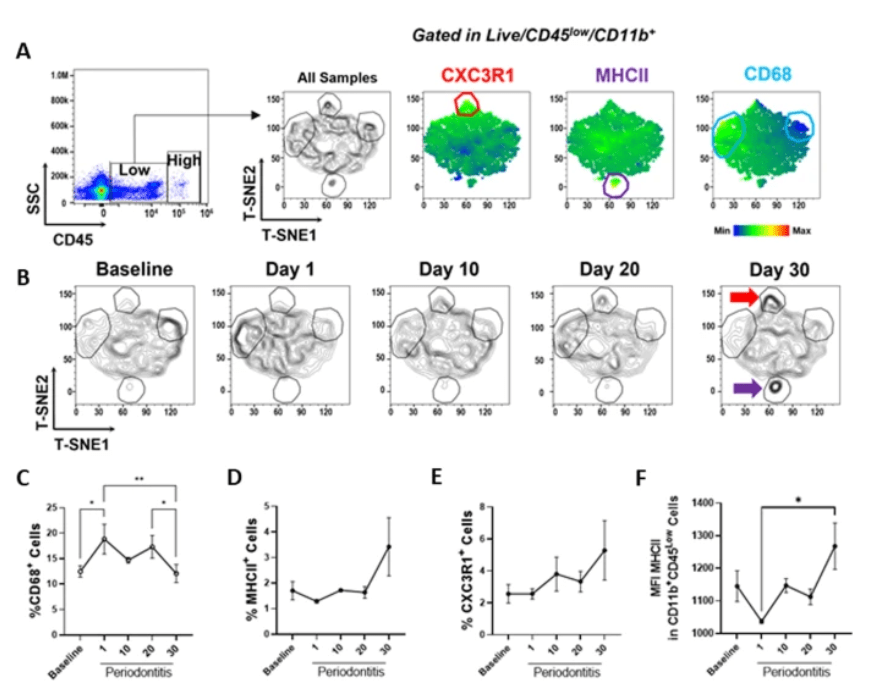
Impact of ligature-induced periodontal disease on microglial cell activation in vivo. A Multiparametric analysis of microglia (CD45low CD11b+) by flow cytometry, T-SNE plots indicate CX3CR1, MHCII, and CD68 expression on concatenated data (n = 3 per group). B Differential expression of microglial markers in healthy animals (baseline) and animals with experimental periodontal disease for 1, 10, 20, or 30 days. Red and purple arrows highlight increased expression of CX3CR1 and MHCII, respectively. C Percentage of CD68 + (high) D MHCII + and E CX3CR1 + in microglia. F Mean fluorescence intensity (MFI) of MHCII within MHCII + microglial cells. (Mean ± SEM, ANOVA, *p < 0.05, **p < 0.01)
The Significance of Gum Disease on Systemic Health
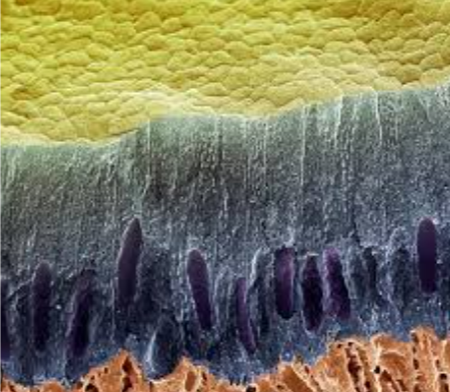
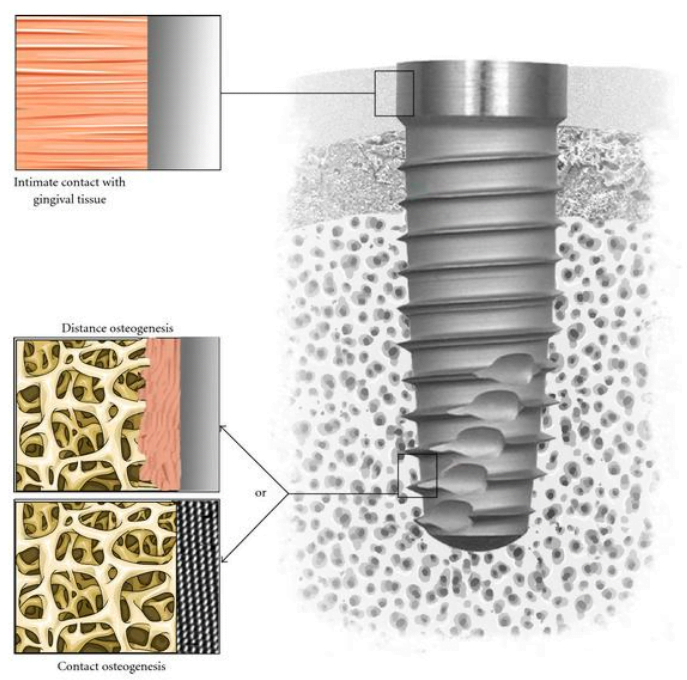
The implications of this study are far-reaching, emphasizing the importance of oral health for overall systemic well-being. Gum disease causes lesions to develop between the gums and teeth, creating an open wound that allows oral bacteria to enter the bloodstream. From there, these bacteria can travel throughout the body, including the brain, by crossing the blood/brain barrier. Once in the brain, they can impact microglial cells, leading to neuroinflammation and potentially contributing to the development and progression of Alzheimer’s disease.
Toward Targeted Strategies and Prevention
The discovery of how oral bacteria can cause neuroinflammation opens up new avenues for targeted strategies in the prevention and treatment of Alzheimer’s disease. Dr. Kantarci emphasizes the critical role of controlling oral inflammation and infection to prevent neurodegeneration and systemic diseases, such as Alzheimer’s. By taking care of oral health and addressing gum disease, it may be possible to reduce the risk of developing cognitive disorders and improve overall brain health.
The Promise of Future Research
This study marks the first time that scientists have successfully induced periodontal disease in mice using mouse-specific bacteria, making it a crucial step toward understanding the oral microbiome’s effects on the brain. While the research focused on mice, the use of same-species bacteria and cells brings us closer to replicating the process as it occurs in humans, providing hope for more targeted and effective treatment approaches in the future.
A Comprehensive Approach to Brain Health
As the scientific community continues to explore the intricate relationship between oral health and systemic diseases like Alzheimer’s, a holistic approach to brain health becomes essential. Beyond oral hygiene, adopting a brain-healthy lifestyle may contribute to overall cognitive well-being.
- Regular Physical Activity: Engaging in regular exercise has been linked to better brain health and reduced risk of cognitive decline. Physical activity promotes better blood flow to the brain, which can aid in the removal of toxins and support optimal brain function.
- Balanced Diet: Consuming a well-balanced diet rich in antioxidants, omega-3 fatty acids, and nutrients supports brain health. Foods such as fish, fruits, vegetables, nuts, and whole grains are associated with cognitive benefits.
- Mental Stimulation: Keeping the brain active through puzzles, reading, learning new skills, or engaging in hobbies can help maintain cognitive function and potentially reduce the risk of neurodegenerative diseases.
- Adequate Sleep: Prioritizing sufficient and restful sleep is crucial for brain health. During sleep, the brain performs essential functions such as memory consolidation and toxin removal.
- Stress Management: Chronic stress can have detrimental effects on the brain and overall health. Adopting stress-reduction techniques such as meditation, mindfulness, or relaxation exercises can promote brain well-being.
Spreading Awareness and Supporting Research
As we uncover more about the link between oral health and cognitive function, it is essential to raise awareness among the general public, healthcare professionals, and policymakers. Recognizing the potential impact of gum disease on brain health can encourage individuals to prioritize oral hygiene and regular dental checkups.
Furthermore, supporting research in this field is crucial to deepen our understanding of the complex relationship between oral health and systemic diseases like Alzheimer’s. Increased funding and collaboration among scientists, institutions, and healthcare organizations will accelerate progress in identifying effective prevention and treatment strategies.
Conclusion
The research conducted by the Forsyth Institute and Boston University has significantly advanced our understanding of the link between gum disease and Alzheimer’s. The study demonstrates how oral bacteria can impact brain cells and contribute to neuroinflammation, potentially affecting cognitive health. It reinforces the importance of maintaining good oral health as a measure to prevent not only oral diseases but also serious systemic conditions like Alzheimer’s disease. As the medical community continues to explore these connections, the study’s findings offer hope for the development of targeted strategies and treatments to mitigate the risk of neurodegenerative disorders and promote healthier brain aging.
Sources
- Science Daily – Gum disease linked to buildup of Alzheimer’s plaque formation 2023 July 10;
- Journal of Neuroinflammation – Microglial cell response to experimental periodontal disease 2023 June 14.