Orthopedic and Surgical Aspects of Immediate Implantation: Analysis of a Case of Upper Jaw Tooth Restoration with a 9-Year Follow-Up
Thanks to advances in surgical techniques, biomaterials, and implant surfaces, dentists can now use simple procedures and proven techniques to achieve soft and bone stability in single-stage implant protocols. Today, we will briefly examine such a case, which was described in the online magazine Wiley (Online Library), where you can read the full version of the study.
For comprehensive insights into modern implant protocols, see our related cases:
This and other cases demonstrate that immediate loading of implants in the aesthetic zone can be indicated and even recommended. Otherwise, after tooth extraction, partial loss of the height and edge of the buccal bone wall occurs within six months. Preservation of the buccal bone supporting the gingival tissue and alveolar anatomy is important for the preservation and restoration of the soft and hard tissues around the implant. Most importantly, the immediate implantation procedure ensures the stability of periodontal structures.
Description of the IDR method
Immediate Dentoalveolar Restoration (IDR), first described by Rosa et al. in 2013, is a one-step approach that involves atraumatic tooth extraction, immediate implant placement, and buccal bone reconstruction with autogenous bone and soft tissue grafts, as well as temporary prosthetics. This method has many advantages compared to conservative approaches:
- Reduction of total treatment time
- Decreased bone resorption
- Immediate restoration of aesthetics
- Preservation and even improvement of soft tissue profile
- Stability of soft tissue connections
Advantages of the IDR method
The Immediate Dentoalveolar Restoration (IDR) technique has several key advantages that make it the right choice when both aesthetics and functionality need to be preserved:
- Bone preservation
Placing an implant immediately after tooth extraction reduces the likelihood of alveolar bone resorption, especially in the area of the buccal wall, which is most vulnerable after tooth extraction. Autogenous bone material used in IDR has excellent osseointegration properties, promoting bone tissue regeneration. - Soft tissue aesthetics
Quick placement of a temporary crown and restoration of the bone structure help maintain the natural contour of the gums. This is especially important in aesthetically significant areas such as the anterior teeth. - Reduced treatment time
Traditional approaches to implant placement can take anywhere from several months to a year. In contrast, IDR reduces the overall treatment time, as all mandatory stages (tooth extraction, implant placement, bone and soft tissue reconstruction) are performed in one visit. - Minimal trauma
Atraumatic tooth extraction and minimally invasive surgical procedures contribute to rapid tissue healing and pain reduction. - Predictability of the result
Modern research confirms the success rate of the IDR method, reaching more than 95%. This makes it a reliable choice for patients considering both aesthetic and functional requirements.
Main steps of IDR procedure
The immediate dentoalveolar restoration procedure includes the following steps:
- Diagnostics and planning
A thorough clinical and x-ray examination allows us to determine the anatomical features of the alveoli, the presence of inflammatory processes, the condition of the soft tissues, and the amount of bone regeneration. - Tooth extraction
The tooth is removed atraumatically, preserving the surrounding tissue. Particular attention is paid to preserving the buccal wall, as it plays a key role in the aesthetic result. - Implant placement
The implant is placed immediately after tooth extraction, with adjustments to ensure a reliable primary stability. - Bone reconstruction
Bone deficiencies are addressed using autogenous bone material, which is taken from the patient’s own body (e.g., from the retromolar region). This ensures maximum biocompatibility and osseointegration. - Temporary prosthetics
A temporary crown is fixed to the placed implant, ensuring immediate restoration of aesthetics and protection of the regenerating area from injury. - Control and rehabilitation
The patient undergoes regular examinations to monitor tissue healing. After 4-6 months, the temporary crown is replaced with a permanent one, made to fit the final profile of the gums and dentition.
IDR use case
A 36-year-old female patient presented to the Department of Periodontology at the School of Dentistry of Aracatuba, UNESP, for treatment of tooth 24 on the left side of the maxilla. Her complaints included tooth mobility, pain during chewing, and bleeding both during chewing and spontaneously.
The tooth had previously undergone endodontic treatment, and a ceramic crown had been placed. A recent examination revealed:
A recent survey showed:
- Confirmed probing depth of 10mm in the buccal side
- Class 1 tooth mobility
- Periapical radiograph revealed an inadequate endodontic treatment and vertical bone loss on the mesial and distal of the tooth, and the bone height above the root apex was 8 mm. In addition, it was clear that endodontic treatment was not adequate.
After prosthesis removal, a vertical fracture in the mesial side of the teeth was observed. As a result, the tooth was declared hopeless. The treatment proposed to the patient was the IDR technique with simultaneous regenerative procedure, dental implant placement, and prosthesis provisionalization in a one-stage approach. The patient provided written consent for this treatment.
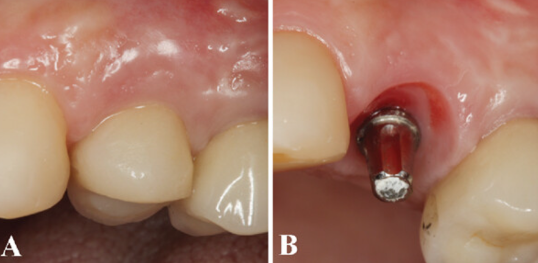
The first stages of treatment are shown in the photo below, including the removal of the crown.
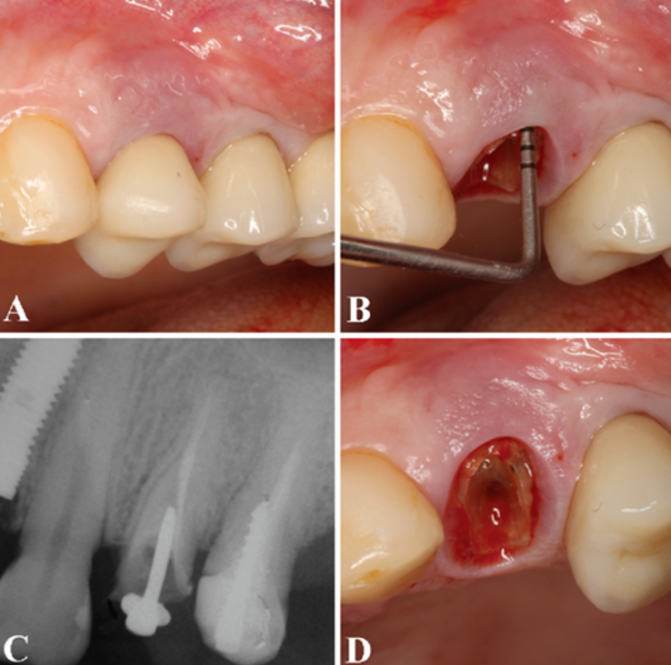
(A) The clinical examination showed class I tooth mobility, unsatisfactory endodontic treatment, and a ceramic crown. (B) The periodontal probing confirmed 10 mm of probing depth in the buccal side. (C) Periapical radiograph revealed an inadequate endodontic treatment and vertical bone loss on the mesial and distal of the tooth, and the bone height above the root apex was 8 mm. (D) After prosthesis removal, a vertical fracture in the mesial side of the teeth was observed, which indicated its extraction. /Wiley/Online Library/Gabriel Mulinari-Santos
Tooth extraction was performed under local anesthesia using an atraumatic protocol. The sulcus was incised with a 15C blade, and the root was removed using a periotome. During removal, the interdental papillae was preserved. After removal, the socket was curetted to remove granulation tissue.
Next, the implant was placed directly into the socket. The dimensions of the implant were ⌀3.5 x 13 mm, and the apical, palatal, and residual alveolar bone was sufficient for acceptable primary implant stability, with a torque of 42 Ncm. The alignment of the implant was slightly palatal, and the distance to adjacent teeth was at least 2 mm.

(A) After tooth removal, a dental implant (3.5 × 13 mm) was placed into the fresh extraction socket. The drilling sequence started with a spear drill, followed by a 2 mm cylindrical drill, and a 3.5 mm conical-shaped drill concerning the mesial, distal, and palatal spaces to accomplish adequate tridimensional positioning. (B) The implant placement was performed with a flapless technique preserving the interdental papillae. (C) Implant alignment was slightly palatal, at least 2 mm distant from the nearby teeth in the mesial and distal region, and the primary implant stability achieved was 42 Ncm. (D) A titanium cylinder was attached to the implant platform./Wiley/Online Library/Gabriel Mulinari-Santos
To compensate for the deficiency of bone tissue, an autogenous bone graft taken from the maxillary tuberosity was used. The harvested bone graft was placed into the defect area without the need for sutures. This is why the protocol for atraumatic tooth extraction using the IDR technique was chosen. If a flap of soft tissue had been removed, such a simple bone grafting procedure would not have been possible.
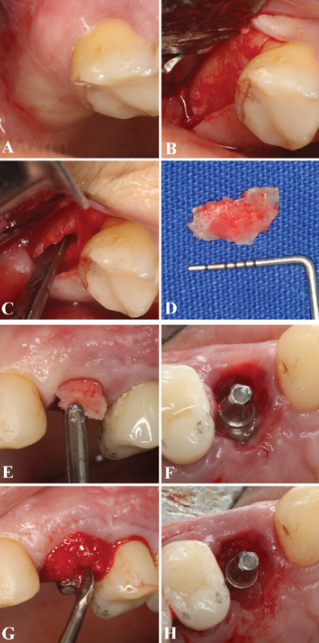
(A) The maxillary tuberosity was the region utilized to obtain the autogenous bone block graft. (B) After local infiltrative anesthesia, a vertical and crestal incision was performed following a full-thickness flap to access the right maxillary tuberosity. (C) A straight chisel (Quinelato, Rio Claro, SP, Brazil) was used to harvest the block bone. (D) The bone graft was customized according to the form of the bone defect, (E) and it was then inserted gently into the alveolar defect above the implant threads using the flapless technique. (F) Occlusal view of the fresh extraction socket with the dental implant positioned immediately after the buccal wall reconstruction with the tuberosity bone graft, allowing a reminiscent gap between the block bone and the implant. (G) The gap was filled with particulate bone harvested from the tuberosity and ground with a bone mill (Neodent, Curitiba, PR, Brazil) to guarantee the bone block maintenance and support. (H) Final occlusal view of the particulate bone completely inserted into the gap between the block bone and the implant./Wiley/Online Library/Gabriel Mulinari-Santos
Even before the bone graft was inserted, a titanium abutment was installed, on which a temporary crown made of PEEK plastic was placed. The crown was adjusted to avoid occlusal contact, thereby reducing the load on the implant, which had not yet undergone osseointegration.
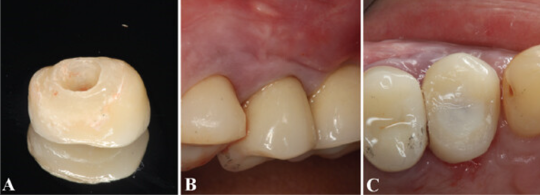
(A) After the surgical procedures, the provisional resin crown was customized. (B) Prosthesis adjustments were performed to guarantee a proper emergence profile. (C) The tooth incisal height was reduced to avoid occlusal contact during chewing and phonation./Wiley/Online Library/Gabriel Mulinari-Santos
6 months after implant placement, follow-up showed an excellent esthetic result, there was no gingival recession, no bleeding, and no abnormal probing depths.
The permanent crown was made according to a standard protocol, so we will not dwell on the description of the process; details can be found in the original article. We are more interested in how successful the treatment was, as shown in the pictures below.
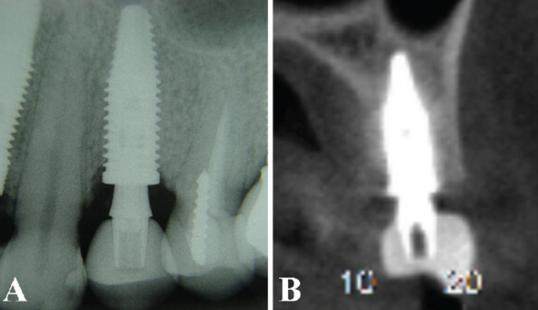
(A) The periapical radiography showed a complete implant osseointegration without signs of bone resorption. (B) The computed tomography scan showed no bone alterations in width and height surrounding the implant.
The 9 years of follow-up have shown an adequate width and thickness of gingival architecture and satisfactory esthetic result without apical gingival migration or probing depths. Moreover, periapical radiographs showed the ideal tridimensional position of the implant and the increased vertical bone gain without marginal bone loss. Thus, the functional and esthetic expectations of the patient were accomplished by the IDR technique.
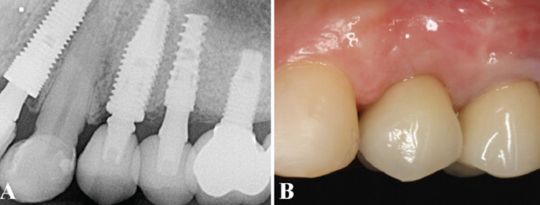
(A) Periapical radiographs after 9 years of follow-up showed the implant position and the vertical bone gain without marginal bone resorption. (B) The clinical examination revealed an adequate gingival thickness, without gingival recession or probing depths, confirming the satisfying esthetic result by the IDR treatment./Wiley/Online Library/Gabriel Mulinari-Santos
Conclusion
Immediate Dentoalveolar Restoration (IDR) is no longer experimental, yet many practitioners have not yet incorporated it into their practice. The purpose of this post is to demonstrate that the technique has been refined and that mastering the IDR technique is not overly difficult. Clients who need immediate assistance will be grateful and may recommend you to others in their social circle.
The effectiveness and accessibility of the method make it the standard in challenging situations involving the removal of teeth in the smile line.
Sources
Wiley (Online Library) – One-Stage Approach to Rehabilitate a Hopeless Tooth in the Maxilla by Means of Immediate Dentoalveolar Restoration: Surgical and Prosthetic Considerations – 10 February 2024