How good is injectable PRF combined with the technique of autogenous demineralized dentin graft injection in comparison to classical ARP methods (alveolar ridge preservation)
Today we will introduce you to an interesting study conducted by colleagues at the Faculty of Dentistry, Cairo University (Egypt). Dr. Odai Amer and his colleagues decided to test whether the combination of ADDG (autogenous demineralized dentin graft) and i-PRF (injectable platelet-rich fibrin) would be more effective than just ADDG. The following criteria were chosen to evaluate the efficacy:
- Reduction in alveolar ridge width – the smaller the loss the better;
- Reduction in alveolar ridge height-the less loss the better;
- Loss of volume and width of attached keratinized gingiva-the less loss the better;
- Postoperative pain level-the less pain the better;
- Histomorphometry – assessment of the level of newly formed bone, and its quality through residual fragment analysis.
Study design: double-blind, randomized, parallel controlled clinical trial with 1:1 allocation ratio to compare i-PRF and ADDG (test group) with ADDG alone (control group).
Summary of the study and key findings
Twenty-two single-rooted (non-molar) teeth of the maxilla were extracted as part of the study. The group of patients was divided randomly so that 11 of the post-extraction wells received ADDG combined with i-PRF and the remaining 11 wells received ADDG alone. All the selected patients were above 18 years of age, somatically healthy, non-smokers, and maintained and maintained good oral hygiene.
The extracted teeth of the patients themselves were used for the preparation of ADDG. The extracted tooth was thoroughly cleaned of any residual periodontal ligament, cementum, soft tissue attachments, caries or restorations. The pulp chamber was thoroughly cleaned. The tooth was then pulverized with a manual bone mill. To prepare the ADDG particles, the tooth graft particles were first demineralized by immersing them in 0.6 N hydrochloric acid for 30 minutes, then washed twice with saline solution and dried with sterile gauze. The graft was then placed in the well and the well was closed with a collagen membrane. The edges of the wound were fixed with a single cruciate suture.
Clinical steps of graft harvesting, demineralization, placement, suturing and 6 months of follow-up for the test and control groups. i-PRF withdrawal, mixture of ADDG with i-PRF in the test group. Biopsy harvesting steps using trephine bure and implant placement. Clinical Oral Implants Research/ clr.14372 /October 2024
For the ADDG + i-PRF group, the demineralized mixture was prepared in the same way, but before injection, platelet-rich fibrin, which was isolated from 10 ml of venous blood from the patients themselves, was added to the well. The i-PRF was prepared in a standardized manner:
- 700 rpm centrifuge
- processing time of 3 minutes in special tubes
Injected PRF was collected from the top of the tube, mixed with ADDG. The mixture was left for 10 minutes to acquire plastic properties (sticky ADDG). The prepared sticky mixture was placed in the wells, covered with a collagen membrane and the wound edges were fixed with a single crosswise suture.
After 6 months, clinical and radiological evaluations revealed:
- Ridge Width Reduction: 1.71 ± 1.08 mm (ADDG + i-PRF) vs. 1.8 ± 1.35 mm (ADDG)
- Ridge Height Reduction: 1.11 ± 0.76 mm (ADDG + i-PRF) vs. 1.8 ± 0.96 mm (ADDG)
- Keratinized Tissue Width Loss: Significantly less in ADDG + i-PRF (0.12 ± 0.34 mm) compared to ADDG (0.58 ± 0.34 mm), p = 0.008
- Postoperative Pain: Lower in ADDG + i-PRF group (p = 0.012)
- Histomorphometry: Comparable levels of newly formed bone and residual graft particles in both groups
Both ADDG + i-PRF and ADDG alone show commensurate results and similar efficacy for ARP. That said, ADDG + i-PRF is possibly associated with easier graft processing (sticky ADDG is easy to handle), less patient-reported pain, and improved preservation of keratinized tissue during healing. Further randomized clinical trials standardizing and testing different dentin graft particle sizes and the effects of ARP in post-removal molar wells are needed.
Mechanisms & Biological Pathways
The rationale behind combining i-PRF with ADDG lies in leveraging the osteoconductive scaffold of demineralized dentin with the bioactive growth factors in i-PRF.
- Demineralized dentin contains type I collagen and bioactive molecules that support bone regeneration.
- i-PRF, a second-generation platelet concentrate, releases key cytokines like TGF-β1, PDGF, and VEGF that:
– Stimulate angiogenesis
– Promote cell migration
– Modulate inflammation and pain
This combination is hypothesized to enhance soft tissue healing while maintaining similar bone quality as conventional grafting methods.
Implications for Professionals
This study offers several takeaways for oral surgeons, implantologists, and periodontists:
- Comparable Hard Tissue Results: Clinically and histologically, both ADDG and ADDG + i-PRF showed equivalent efficacy in alveolar ridge preservation.
- Soft Tissue Advantage: The preservation of keratinized tissue width with ADDG + i-PRF may enhance esthetic outcomes, particularly in anterior maxillary restorations.
- Reduced Patient Discomfort: Lower pain scores suggest faster and more comfortable healing, a significant advantage for patient satisfaction.
- Practicality: Chair time remained consistent between groups, and patients expressed similar levels of satisfaction, supporting the feasibility of adopting i-PRF in clinical routines.
Study Overview
- Design: Prospective, randomized clinical trial
- Sample Size: 22 extraction sockets (11 per group)
- Interventions:
– Teeth were extracted, and dentin was processed into autogenous demineralized graft
– One group received i-PRF amalgamated with the graft
– Sites were sealed with a collagen sponge
- Assessments:
– CBCT scans at baseline and 6 months
– Pain scores, keratinized tissue width, patient satisfaction, and chair time
– Histological analysis of bone biopsies during implant placement
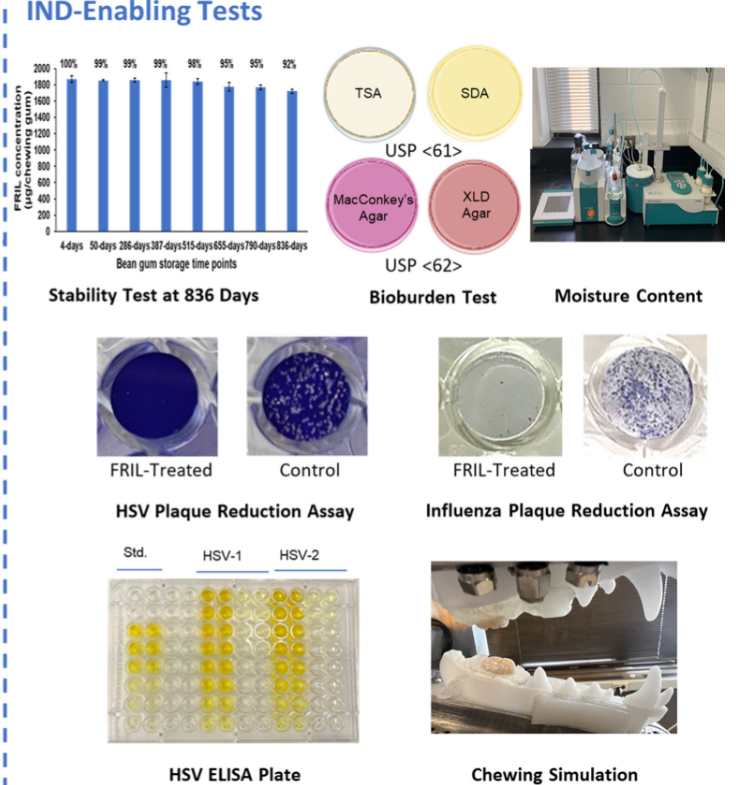
Data Visualization
Conclusion
The combination of autogenous demineralized dentin graft with i-PRF offers a viable, patient-friendly option for alveolar ridge preservation. While bone regeneration outcomes remain consistent with or without i-PRF, the addition of this injectable biologic enhances soft tissue maintenance and reduces postoperative discomfort, offering a competitive edge in aesthetic zone management. This strategy could be particularly valuable for clinicians aiming to optimize both hard and soft tissue outcomes without extending chair time or compromising bone quality.
FAQs
1. What is ADDG and how is it prepared?
Autogenous Demineralized Dentin Graft (ADDG) is made from a patient’s extracted tooth. The dentin is cleaned, ground, and demineralized to create a biocompatible graft material for bone regeneration.
2. What makes i-PRF different from other platelet concentrates?
i-PRF is an injectable form that releases growth factors over time, enhancing soft tissue healing and reducing inflammation. It’s easy to mix with graft materials and does not require anticoagulants.
3. Can ADDG + i-PRF be used in all extraction sockets?
This combination is particularly beneficial in the anterior maxillary zone, where aesthetics and soft tissue preservation are critical. Broader application would require further clinical validation.
4. Does using i-PRF add to the surgery time or cost?
The study found no increase in chair time. While i-PRF does require centrifugation equipment, its benefits in healing and tissue quality may offset the investment for many practices.
5. Is there any risk associated with i-PRF?
Since i-PRF is autologous (derived from the patient’s own blood), it carries minimal risk of rejection or infection. It’s considered a safe and effective adjunct in oral regenerative procedures.
Sources
Wiley Online Library – Does Injectable Platelet-Rich Fibrin Combined With Autogenous Demineralized Dentine Enhance Alveolar Ridge Preservation? A Randomized Controlled Trial – 21 October 2024