New Research Confirms the Importance of Precise Occlusal Balance in Dental Implantation
Recent research in dental implantology demonstrates that using thin occlusal paper (12 μm) can significantly improve the restoration of occlusal balance after implant placement.
According to a new study published in January 2025 in Heliyon journal [1], the proper selection of occlusal paper thickness plays a crucial role in achieving optimal occlusal balance in implant prosthetics.
Key Research Findings
A year-long study involving 100 patients revealed several important findings:
- Using 12 μm occlusal paper provides better occlusal balance compared to 20 μm paper
- Significant improvement in occlusal balance indicators was observed 3 months after restoration
- Recovery time has a greater impact on occlusal balance than the degree of occlusal tightness
Clinical Data
The study analyzed 100 patients who received posterior dental implant restorations between July 2022 and July 2023. Patients were divided into two equal groups: the observation group using 12μm occlusal paper and the control group using 20μm occlusal paper. Various clinical parameters were measured to assess the impact of occlusal paper thickness on implant restoration outcomes. The baseline characteristics and clinical outcomes of both groups are presented in the following tables.
Table 1: Comparison of General Data Results
| Index | Control group (n = 50) | Observation group (n = 50) | t/χ2 | P |
|---|---|---|---|---|
| Gender (male/female) | 27/23 | 24/26 | 0.360 | 0.548 |
| Age (years) | 44.34 ± 6.67 | 44.44 ± 6.74 | 0.075 | 0.941 |
| Implant sites (maxillary/mandibular) | 22/28 | 21/29 | 0.041 | 0.840 |
The baseline demographic and clinical characteristics were similar between the two groups, with no statistically significant differences (p > 0.05). This balanced distribution in terms of gender, age, and implant sites ensures that any observed differences in outcomes can be attributed to the occlusal paper thickness rather than underlying patient characteristics.
Table 2: Comparison of Clinical Indicators
| Index | Control group (n = 50) | Observation group (n = 50) | t | p |
|---|---|---|---|---|
| Peri-implant bone resorption degree (mm) | 0.36 ± 0.12 | 0.34 ± 0.13 | 0.943 | 0.348 |
| Periodontal pocket depth (mm) | 2.18 ± 0.21 | 2.16 ± 0.19 | 0.439 | 0.661 |
| Gingival index (grade) | 1.08 ± 0.40 | 1.12 ± 0.39 | 0.512 | 0.610 |
| Tooth looseness (scores) | 2.04 ± 0.53 | 2.00 ± 0.45 | 0.405 | 0.686 |
The clinical indicators were carefully selected to evaluate the impact of occlusal paper thickness on key aspects of implant success. These measurements included peri-implant bone resorption, periodontal pocket depth, gingival health, and tooth stability – all critical factors in assessing long-term implant outcomes.
Analysis of these clinical parameters revealed no significant differences between the 12μm and 20μm groups across all indicators (p > 0.05). This suggests that the use of thinner occlusal paper (12μm) does not compromise the biological and mechanical stability of the implant restoration, while potentially offering better precision in occlusal adjustment.
Research Results Visualization
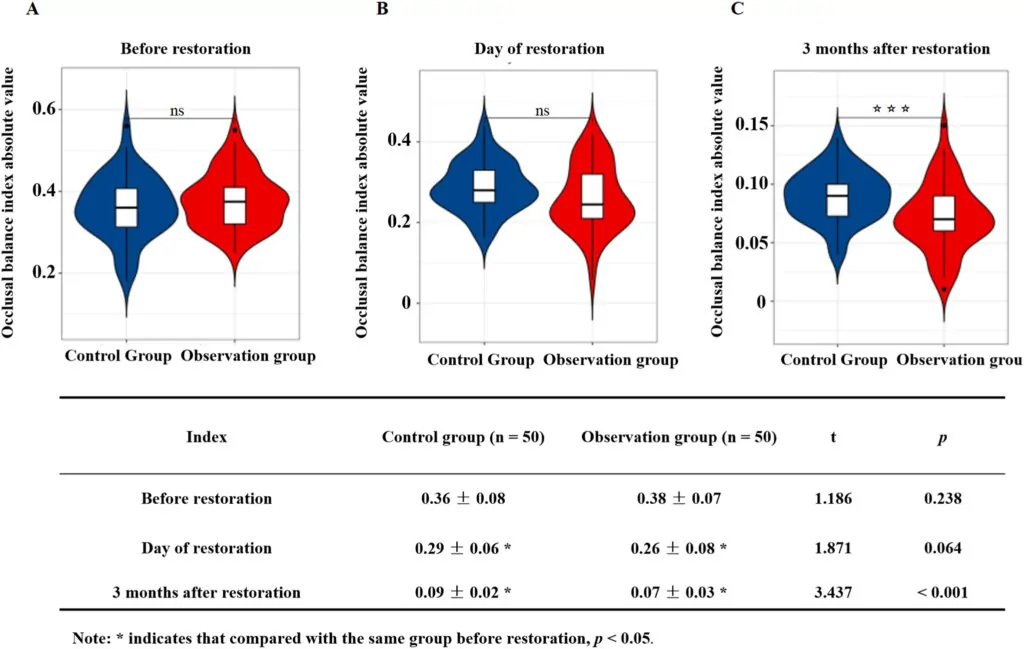
The absolute value of occlusal balance index in two groups before repair, on the day of repair, and 3 months after repair. Source: Heliyon journal [1]
Why This Matters for Dental Practitioners
The study results emphasize the necessity of a careful approach to occlusal correction during implantation. Precise occlusal adjustment not only improves the functionality of prosthetics but may also extend implant longevity.
These observations challenge the common assumption about occlusal paper thickness. Using 12 μm paper instead of thicker alternatives enables more precise adjustments, reduces adjustment sessions, and minimizes the risk of over-adjustment that can affect implant stability.
Clinical evidence demonstrates that the first three months after restoration are critical for achieving optimal occlusal balance. Regular follow-up appointments during this period are essential for treatment success and should be incorporated into standard post-implant protocols.
Practical Recommendations
Based on the research, several key recommendations for clinical practice emerge:
- Prefer thinner occlusal paper (12 μm) for more precise occlusal adjustment
- Conduct follow-up examinations 3 months after restoration to evaluate occlusal balance
- Consider that achieving optimal occlusal balance is a process that requires time
Additional Observations
Interestingly, the study found no significant differences between patient groups regarding:
- Peri-implant bone resorption
- Periodontal pocket depth
- Gingival index
- Tooth mobility
These findings indicate that varying the occlusal paper thickness has minimal impact on primary clinical indicators in the short term [1]. Additional research has shown that thicker occlusal papers (200 μm) produced larger contact marks compared to thinner ones (16 μm), regardless of the applied force [2].
Conclusion
This research highlights the importance of proper occlusal paper thickness selection for achieving optimal balance in implant prosthetics. Using thinner paper (12 μm) can accelerate the achievement of occlusal balance and improve overall implantation outcomes.
References
[1] The effect of occlusal balance and prosthesis on occlusal function of patients after dental implant restoration. Heliyon, January 2025. DOI: 10.1016/j.heliyon.2025.e41732
[2] Evaluation of the occlusal contact area of molar dental implants comparing two different thicknesses (16 μm and 200 μm) of articulating occlusal papers and forces (200 and 250 N): a pivot in vitro study. International Journal of Science Dentistry, 2022.