Why soft gums are more prone to inflammation – new research results
Recent research has revealed a correlation between gingival stiffness and the behavior of gingival fibroblasts, which play a crucial role in the formation of fibers responsible for anchoring teeth.
Gingival Stiffness and Inflammation
Studies conducted by scientists at Tohoku University have shown that soft gingiva can hinder the development of gingival fibroblasts, subsequently leading to inflammation and difficulties in forming gingival fibers. Their findings were published on January 24, 2023. Fibroblasts play a key role in maintaining and repairing gingiva. Several types of collagen fibers support teeth and serve as a cushion. Only a few varieties of collagen threads regenerate and attach to dental implants.This often leads to gaps appearing between the teeth and dentures over time. Therefore, dense, well-keratinized gingiva that is attached to the bone is always a good prognosis for the long-term survival of implants.
However, fibroblasts also participate in the body’s immune response to pathogens. In addition to processes of restoration and maintenance of the gingiva, they also generate inflammatory biomolecules that can destroy gingival fibers. Assistant Professor Masahiro Yamada of Tohoku University’s School of Dentistry believes that soft gingiva prone to recession leads to inflammation and suppression of gingival fiber production in such patients.
In contrast, individuals with thick or stiff gingiva exhibit lower susceptibility to gingival recession, characterized by gingival recession and tooth root exposure. Although various factors contribute to gingival recession, such as gum disease and excessive tooth brushing, gingival stiffness has emerged as an important biological factor in preventing inflammation and maintaining healthy gingival fibers.
Comparison Table:
| Aspect | Soft Gingiva | Stiff Gingiva |
| Fibroblast Development | Hindered | Normal |
| Inflammation Likelihood | Increased | Decreased |
| Gingival Fiber Formation Difficulty | High | Low |
| Gingival Recession Susceptibility | Higher | Lower |
| Intracellular Anti-inflammatory System | Suppressed in fibroblasts | Activated in fibroblasts |
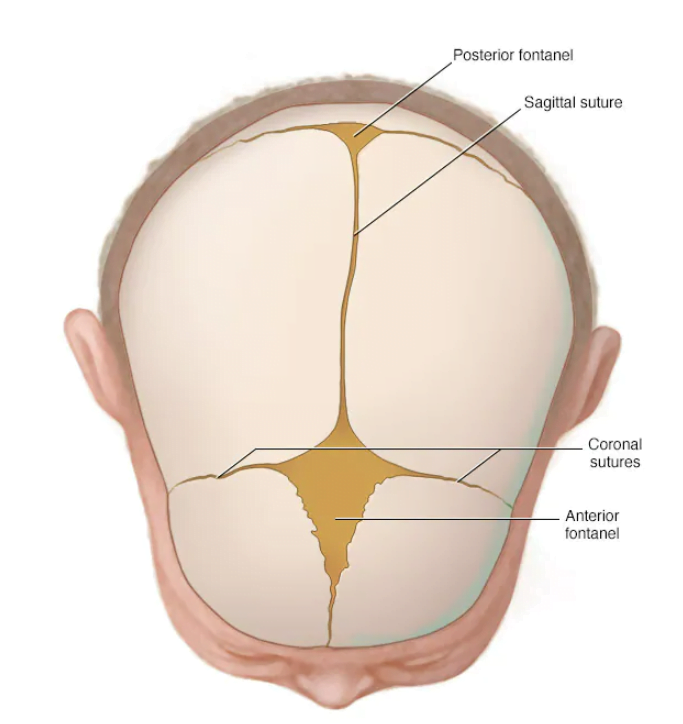
Recall that specialists distinguish two innate gingival biotypes based on the type of gingiva:
- thin biotype – where the layer of attached keratinized gingiva is within 1.5-2 mm;
- thick biotype, where the layer of attached keratinized gingiva is thick and wide, 3-4 mm.
The images below show samples of gingival biotypes by thickness. Attached keratinized gingiva has a characteristic shade. It is lighter and appears more resilient and taut compared to the surrounding tissues.
Thin gingival biotype – characterized by high scallops and teeth appearing triangular
Thick gingival biotype – teeth appear square, and the gingiva is thick and massiveAlthough there is no direct correlation between biotype and gingival health, people with a thin biotype are more likely to lose the keratinized area and develop soft gingiva, increasing the risk of inflammation and impaired collagen fiber synthesis.
How the study was conducted
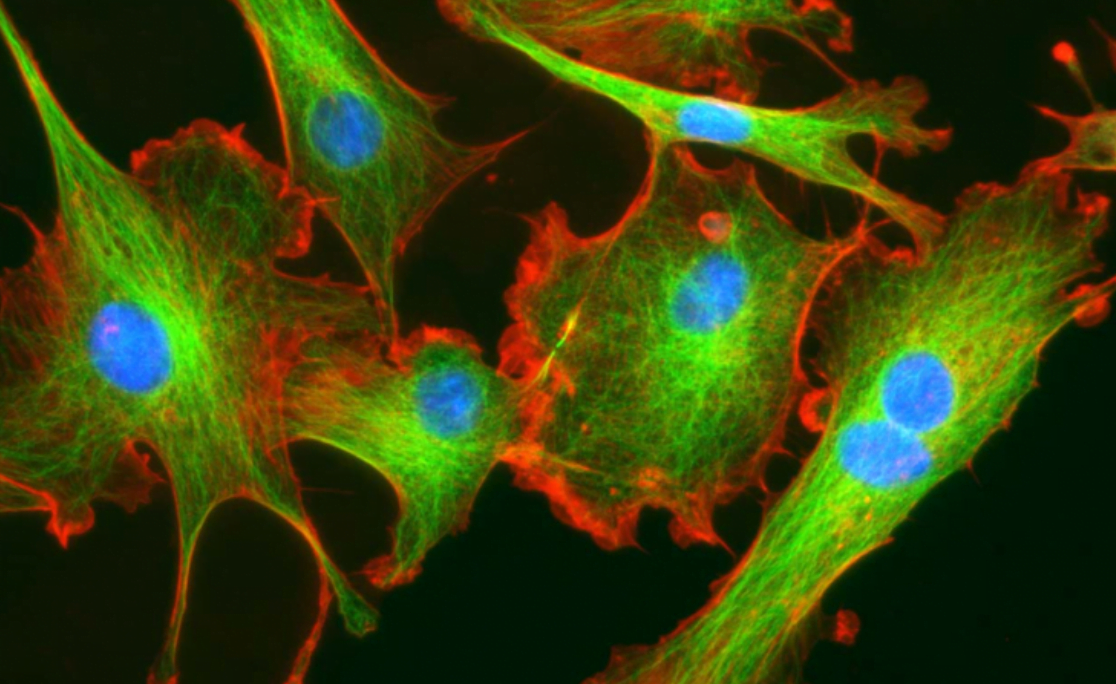
Researchers created an artificial environment that simulated conditions of soft and stiff gingiva. When cultivating fibroblasts in different environments, they observed:
- The environment simulating stiff gingiva activated an intracellular anti-inflammatory system in gingival fibroblasts, preventing inflammation.
- The environment simulating soft gingiva suppressed the fibroblastic anti-inflammatory system, increasing the likelihood of inflammation and leading to reduced collagen synthesis.
Prognoses and achievements in the field of biomaterials and microdevices
It is expected that the research from Tohoku University will accelerate the development of advanced biomaterials for local inflammation control or microdevices that mimic the microenvironment of dense gingiva to suppress inflammatory conditions. This is highly significant because inflammation can lead to gingival recession, potentially causing tooth sensitivity, pain, and even tooth loss.