Exploring the Role of Oral Bacteria in Idiopathic Pulmonary Fibrosis (IPF) Survival
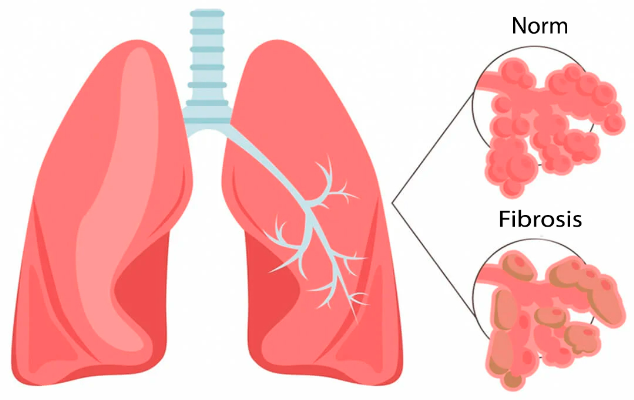
In recent years, the scientific community has delved deeper into understanding the intricate relationship between the human microbiome and various diseases. One such area of focus is idiopathic pulmonary fibrosis (IPF), a progressive and fatal lung disease with limited treatment options. Emerging research, including a study led by researchers from the University of Michigan and the University of Virginia, suggests that the composition of oral bacteria may play a significant role in the survival of individuals with IPF.
The CleanUP-IPF Study: Uncovering Insights into Lung Microbiome
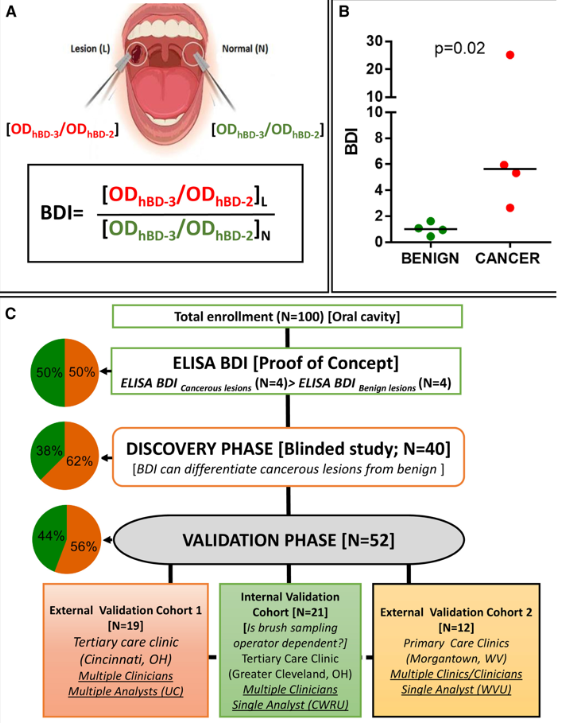
The CleanUP-IPF study represents a groundbreaking endeavor aimed at elucidating the complex interplay between the lung microbiome and IPF. Led by Dr. David O’Dwyer, Dr. John Kom, and Dr. Imre Noth, the study involves the collection and analysis of various biological samples, including cheek swabs, to discern alterations in bacterial populations among patients with IPF.
Surprising Findings: Streptococcus mitis and IPF Survival
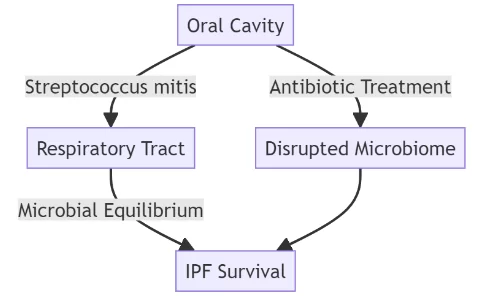
Utilizing advanced genetic techniques such as 16S rRNA analysis, the research team uncovered a compelling association between a specific bacterial species, Streptococcus mitis, and IPF survival. Contrary to conventional wisdom, patients with IPF who harbored higher levels of Streptococcus mitis in their oral microbiome exhibited better lung function, milder disease progression, and increased likelihood of survival.
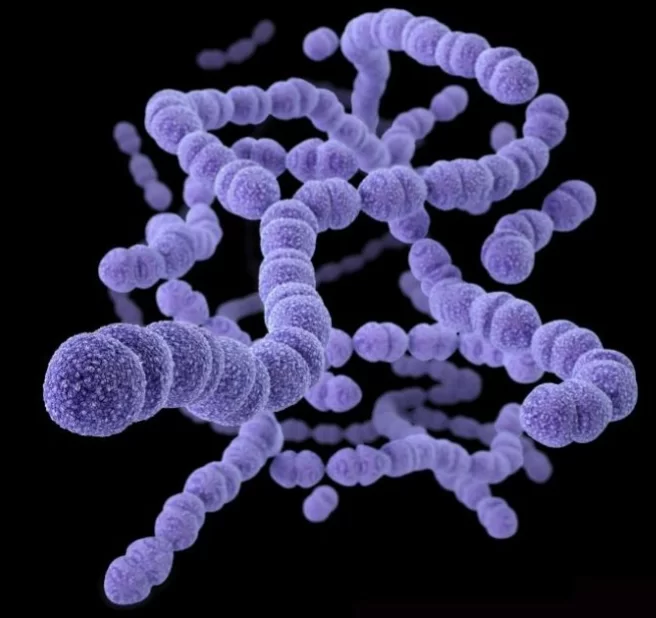
Streptococcus mitis: The Guardian of Oral Health
Notably, Streptococcus mitis emerges as a key protagonist in the narrative of IPF survival. This bacterial species, primarily found in the oral cavity, acts as a formidable guardian against potential microbial threats, including those implicated in periodontal disease. By maintaining a delicate balance within the oral microbiome, Streptococcus mitis effectively curtails the proliferation of pathogenic bacteria, thereby safeguarding oral and, subsequently, respiratory health.
Antibiotics and the Disruption of Microbial Equilibrium
However, the protective role of Streptococcus mitis appears to be compromised in IPF patients who have undergone antibiotic treatment. The administration of antibiotics disrupts the delicate equilibrium of the oral microbiome, potentially diminishing the beneficial effects conferred by Streptococcus mitis. Consequently, these individuals may experience exacerbated disease severity and compromised survival outcomes.
Future Directions: Unraveling the Complexity of Oral-Lung Microbiome Crosstalk
Moving forward, further investigations are warranted to unravel the intricate crosstalk between the oral and lung microbiomes in the context of IPF. Future studies should endeavor to characterize the diverse bacterial populations inhabiting both environments and elucidate their respective contributions to disease pathogenesis and progression. By elucidating the underlying mechanisms governing microbial interactions in IPF, researchers can pave the way for novel therapeutic interventions targeting the microbiome.
In conclusion, the emerging evidence implicating oral bacteria, particularly Streptococcus mitis, in IPF survival underscores the intricate interplay between microbial communities and human health. By elucidating the role of the oral microbiome in respiratory diseases, such as IPF, researchers can potentially identify novel therapeutic targets and interventions to improve patient outcomes.
Sources
- Science Daily – Bacteria in the mouth linked to pulmonary fibrosis survival – February 7, 2024;
- ATS Journals – Commensal Oral Microbiota, Disease Severity and Mortality in Fibrotic Lung Disease – February 6, 2024;