Soft tissue implant integration (part 1)
In this article we will start to review the aspect of patient's health, which is no less important than osteointegration, namely soft tissue integration. The formation of a gingival cuff from soft tissues is no less important than the stability of the dental implant in the bone.
Why soft-tissue integration is no less important than osteointegration
Let’s figure out why the stability and immobility of soft tissue around the implant are no less important than the stable fit of the implant in the alveolar crest.
Before we go further, we will define what soft-tissue integration is.
These are biological processes aimed at the formation and maturation of the structural bond between the soft tissue and the intragingival part of the implant. The structural bond is formed both at the epithelial and connective tissue level. During soft tissue integration, a strong and stable soft tissue cuff is formed around the implant that has cut through the soft tissue and entered the bone. The gingival cuff protects the sterile bone environment from the non-sterile oral environment.
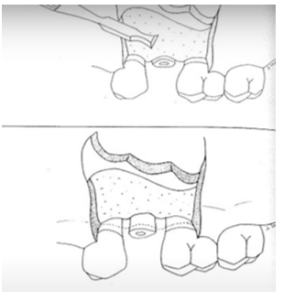
The structure of the tissue that forms around the dental prosthesis is very similar to that around a living tooth, see the illustration above. This is not surprising because the form follows the function. The living tooth and dental prosthesis perform the same function and, therefore, the purpose of the gingival cuff is the same. The body forms similar structures although there are significant differences, but let’s say that the gum cuff around the implant is inferior in strength and stability to the tissues around living teeth.
Next, let’s analyze how soft tissue attachments to a living tooth and to an artificial implant differ.
Key factors influencing the success of soft tissue integration
Let’s figure out how a healthy gum works to understand what problems you will face during implantation. It is the gum that covers the alveolar ridge, it is through it that the teeth erupt. The gum is the structure that protects the teeth and helps keep the mouth healthy. Each section of the gum has its own functions. The terminal (final) part, the so-called marginal gum, covers the cervical region of the tooth. In the gingival groove (sulcus), special substances are released that interact with the microflora of the oral cavity, but more on that later.
Below the marginal part there is a band of attached keratinized gingiva. It is dense and rigid due to keratin (fibrillar proteins) and provides stability to all soft tissue structures. Without a solid band of attached gum, the cervical part of the tooth cannot be healthy, the gum becomes unstable, and chronic inflammation occurs around the tooth.
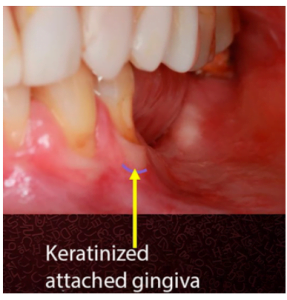
The photo below shows a healthy mouth where you can clearly see the keratinized part of the gum. In this case it is quite wide. It is slightly whitish and visually different from the pink mobile mucosa above.
There is no consensus on what width of the attached keratinized gingiva is the norm. But it is known that even a narrow band of 1 mm is sufficient to maintain the health of the cervical part of the teeth. Provided, of course, that personal hygiene is maintained.
In the following image, the patient has partial adentia and noticeable gum recession on the outermost teeth. However, even on the outermost tooth there is also a strip of keratinized gingiva attached, which indicates that the body is trying to preserve the soft tissue structure, even in difficult conditions.
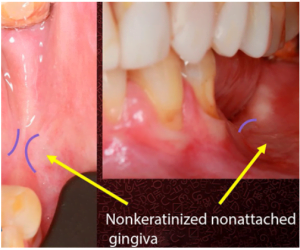
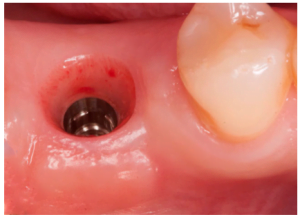
The situation changes in the area where the dentition is completely lost, the picture below shows that the keratinized gingiva is almost dissolved. Especially from the top view, it is clear that there is a barely noticeable strip of keratinized tissue surrounded by a mobile mucosa.
This is a real problem, because if implants are installed in this place, they will be surrounded by a soft mucous membrane with a large number of muscle strands.
Constant soft tissue mobility will lead to chronic inflammation.
The good news is that attached keratinized gingiva has the ability to regenerate, but only in the area of living teeth. Near the implant, processes of restoring keratinized gums can also occur, but are far from being in full. Therefore, it is always better when the volume of the keratinized gum is sufficient. More on this will follow.
As an example, let’s take the well-described experiment in the book by Lange and Linde, where the flap was rotated to the animals and sewn, as it were, in reverse.
That is, on top of the teeth was the area that was below and in fact is part of the unattached movable mucous membrane. The keratinized area was separated and moved down.
Experience showed that after the healing stage, a thin strip of attached keratinized gingiva was formed under the dentition. This confirms the importance of the attached rigid gingiva to the body.
Clinical significance of gingival reattachment and implantation prognosis
However, all of the above applies to living teeth. In the case of implants, the situation is much more complicated. As soon as the tooth leaves, the periodontal ligaments leave, and the whole complex of soft tissue functioning is rebuilt.
If an implant is installed instead of a lost tooth, the body will form a complex of soft tissues similar in structure and function to a living tooth, but a significant part of the structural elements and functions will still be lost.
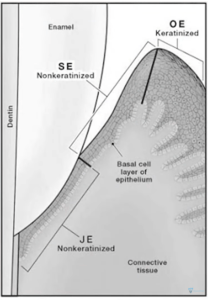
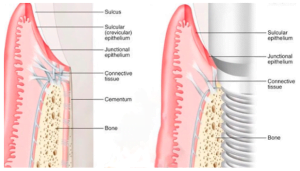
Let’s deal with this in more detail. For this we will move our attention from the outside of the keratinized gum to the depths, see the illustration below. We see that keratinization ends at the top of the papilla, which forms the gingival sulcus. The epithelium of the sulcus consists of necrotic or rather slightly keratinized epithelium.
There is an explanation – this part of the epithelium must be permeable to various antibodies, macrophage cells, protein compounds and other substances that the body excretes through the sulcus. Conventionally, this zone can be referred to as the immune system. After all, sulcus fluid performs chemical and antibacterial protection of nearby tissues.
Then we move on to the attached epithelial part of the gingival cuff. This site consists of more rarely located but wide epithelial cells. Here we will find special structures – hemidesmosomes. With their help, living cells are physically attached to the alien part of the tooth, it does not matter to enamel and dentin. These same intercellular formations are involved in the attachment of the epithelium to the implant surface. Epithelial attachments are also not keratinized.
If we go even lower, we will find the strongest part of the gingival cuff – the connective tissue joint. This structure forms both around the living tooth and around the implant, but is noticeably different in quality. The boundary between epithelial and connective-tissue attachment is quite clear and well-defined.
Connective tissue consists of a large number of differently oriented collagen fibers. In the case of a healthy tooth, the amount of collagen is about 60% of the total volume; the rest is intercellular matrix, water, etc.
It is also important to remember that the connective tissue cuff is always formed below the level of enamel, and attaches to the dentin or cementum of the root. The epithelial bond can form equally well with any surface: enamel, dentin, milled titanium.
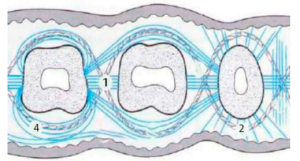
Let us analyze the structure of the connective tissue in the area of teething through the gum. Let’s highlight the four most significant types of fibers:
- Transseptal fibers that pass from one well to another. They slightly resemble ropes or a bandage. The transseptal fibers pass through each well and out to the next, see the figure below.
- Dentogingival (dentolingual) fibers, which begin in the thickness of the gums and are fixed to the surface of the tooth through the so-called intercellular cement. They come in three subtypes:
– crown;
– horizontal;
– apical. - Dentoperiostal (dentoperistal) fibers that connect the neck of the tooth to the periosteum (periosteum of the alveolar crest). The image is not displayed because it is not visible in this projection.
- Circular, semicircular collagen fibers. They surround the tooth around the perimeter, running both parallel to the tooth and diagonally.
In the following figure we see a comparison of the gingival attachment of a living tooth and a root implant. In both cases, the body forms a similar anatomical and structural attachment. The gingival cuff is composed of:
- the gingival sulcus (sulcus);
- epithelial accession;
- connective tissue accession.
This structure is created around a living, transplanted tooth or dental implant.
As can be seen from the figure, in the case of attachment to a dental implant, the amount of collagen fibers is less than compared to a living tooth.
More than that, only circular, seven-circular collagen fibers are formed around the root implant from all the biological diversity. Whereas sulcus and epithelial attachments are completely similar. This is an important fact, and we will return to it later.
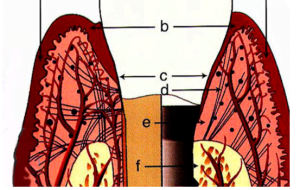
Now let’s compare what happens to the bone and soft tissues after implantation. See the illustration below.
- Of the three sources of blood supply, we lose the periodontium, and this is one of the most powerful sources of nutrition. Accordingly, we lose the anastomoses between the roots of the tooth and the bone of the alveolar ridge. This means that there is no connection of blood vessels from several sources, and the nutrition of soft tissues in this area is poorer.
- Connective tissue attachment is much simpler and more primitive. In the case of a living tooth, there are collagen fibers that attach directly to the tooth. Some fibers go deep into the gum, some are attached to the periosteum, some run parallel and cover the tooth like a ball of string. In the case of a root implant, only the latter variety of parallel fibers remain. These fibers surround and compress the implant to form the connective tissue part of the dental cuff.
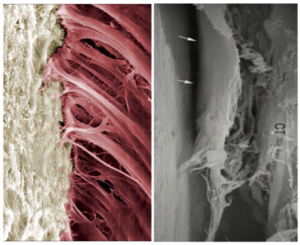
The photo below clearly shows the difference. On the left is a live tooth, where you can clearly see the strong connection of a large number of collagen fibers to the root cement. On the right you can see the structure of collagen fibers around the implant. You can clearly see that this tissue can easily peel off and detach from the implant surface.
Soft tissue integration studies are currently taking place and there are encouraging results. There are confirmed observations that in some cases thin collagen fibrils are formed. They are perpendicular to the implant surface and resemble dentolingual fibers. This is not quite the same as what can be seen on a living tooth, but research is ongoing. Read more about this in the next article in the series on soft tissue integration.
Significance of gingival keratinization – gingival biotype and what it affects
Back to the theme of the attached keratinized gingiva. We already know that the connective tissue attachment of the implant is several times worse in functionality and stability compared to a living tooth. This means that the function of stabilizing soft tissues around the implant falls on the attached gingiva. Therefore, it is important that it is wide enough and well keratinized to provide adequate stability. The photo below shows an attached gingiva that is high-quality both in density and width.. This means that the stability of the implant is likely to be be very high.
The dense and wide gingiva provides mechanical stability to the entire soft-tissue complex. It is currently the only source of stability for the normal functioning of the gingival cuff. In general, without a good quality attached gingiva, there can be no good prognosis for long-term implant survival.
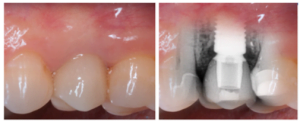
Notice in the illustration below, in the first photo it is hard to detect exactly where the implant is located. We see a wide, well-developed keratinized gingiva.
The second image of a radiograph that shows that the bone ridge is quite far from the implant-abutment line. The image was taken two years after placement, during which time the alveolar ridge was noticeably resorbed and a hole was formed around the implant. In spite of this, the implant performs perfectly. The fact that this implant case can be considered clinically successful is largely due to the healthy and dense keratinized gingiva.
It is also important to consider the patient’s biotype by the type and location of keratinized tissue.
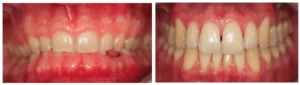
The photo below shows well-defined biotypes. In the first photo, the so-called thick or as it is also called the flat biotype (flat). There is always a lot of keratinized tissue, and, as a rule, the width of the alveolar crest is larger. Also, in this biotype, the gum papillae are not very high, and the teeth look square.
The second photo shows a subtle or festonated biotype. The keratinized gingiva are smaller here, the teeth seem to be bare above and more often have a triangular shape. The gingival papillae between teeth are much higher compared to the thick gingival biotype.
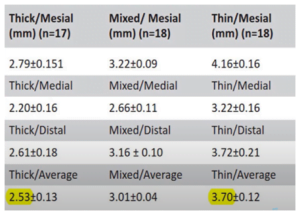
The gingival biotype is directly related to gingival cuff height. Look at the results of research conducted in 2013.
The situation with soft tissues in all projections was assessed here, and the following pattern was noticed – with a thick biotype, the total height of all gingival cuff structures is always less. With a thin one, the total height of all gingival cuff structures is higher – the difference is more than a millimeter, see the table below.
This is most likely due to the greater massiveness of the dense keratinized gingiva with a thick biotype. That is, to achieve the same functions in terms of stability and strength, a lower height of supracrestal tissue attachment is sufficient.
This information is just to show how wrong it is to use average gingival cuff heights. Everything is individual and there are many factors to consider. The biotype is one of the most important factors and must be taken into account when we prepare the implant bed and prepare for the restoration. It is important to understand that when we are working on thin tissues, we need to leave more room for the soft tissue cuff to form.
If there is not enough space, the body will free up space for the gingival cuff due to the bone of the alveolar crest. How exactly the body starts the process of local resorption of the alveolar crest will be analyzed in the next article from the cycle devoted to soft tissue integration.
What is “Biological Width” and why the term is no longer used
In literature and articles, the term – biologic width – is still used. This term refers to a complex of soft tissue attachment including:
- gingival sulcus (sulcus);
- epithelial accession;
- connective tissue accession.
In this article, we have often used the term gingival sulcus as it is more intuitive. The term itself cannot be considered entirely unfortunate, as it was used in operations to restore broken teeth. Dentists were advised to free up space to that very biological width (2.7-3 mm) to form a soft-tissue connection. For clinical indications, it was recommended to remove part of the alveolar ridge to provide space – the biological width.
However, today the term is considered not to be entirely successful and largely counterintuitive, even despite explanations and transcripts. Therefore, in 2017, a new formulation was officially proposed by the International Periodontology Group: supracrestal attachments.
The new term is exhaustive and understandable, and applies equally to the soft tissues surrounding a living tooth and to the gingival cuff around the implant.
In the next article we will look at how supracrestal attachments form and develop during the healing process, how the location of the implant abutment line affects bone resorption and what role the soft tissue attachment has in this.
Until future publications.
-
30 X Straight Multi-Unit Abutment D-Type Conical Connection Regular & Mini Platforms
Original price was: $960.$816Current price is: $816. Buy Now -
30 X Straight Multi-Unit Abutment D-Type Internal Hex Regular Platform
Original price was: $960.$816Current price is: $816. Buy Now -
30 Х 17° and 30° Angled Multi-Unit Abutment D-Type Internal Hex Regular Platform
Original price was: $2,040.$1,428Current price is: $1,428. Buy Now -
50 X Straight Multi-Unit Abutment D-Type Internal Hex Regular Platform
Original price was: $1,600.$1,200Current price is: $1,200. Buy Now