Is it necessary to use a Ti base? Different types of dental parts & digital impression
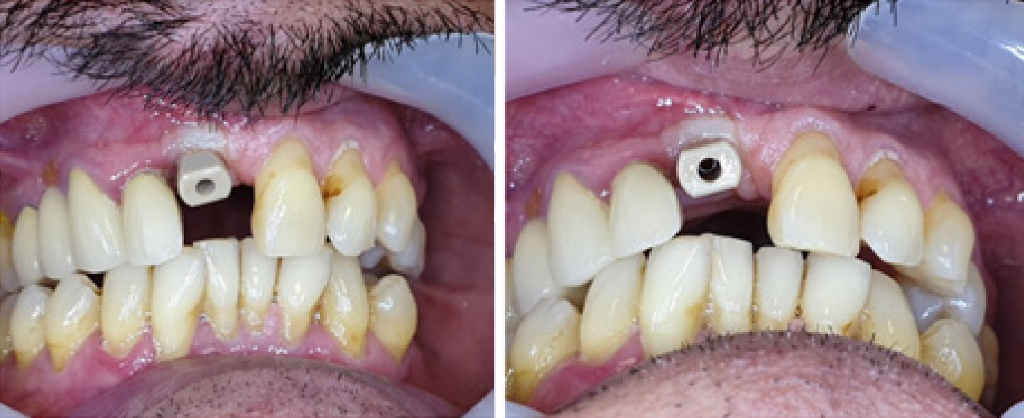
Analysis of the patient’s clinical condition
This case involves the restoration of a single anterior tooth. In such instances where the restoration originatesfrom the coronal aspect, the exclusive component suitable for use is the T-base abutments. These are specifically designed to support the prosthetic material in the fabrication of the final restoration, ensuring both functional integrity and aesthetic harmony with the patient’s natural dentition.
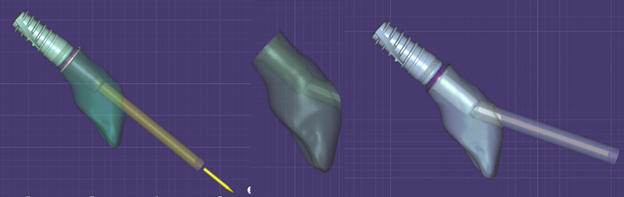
Various component types and their respective applications are demonstrated here. In the present scenario, the dentists have opted for a T-base with an angulated apex. This choice is evident given the buccal inclination of the implant, which positions the screw channel centrally within the tooth. Without altering the screw channel’s angulation, it would emerge centrally through the tooth. Therefore, the aim is to illustrate that altering the screw channel’s inclination towards the palatal region is not always necessary. Occasionally, when presented with a level smile line, the dentists can adjust the screw channel buccally rather than palatally. This adjustment ensures that the screw channel remains concealed when the patient smiles.
One may question the stability of a single-tooth restoration on a solitary implant. The response is affirmative; it will remain stable. However, it is crucial to note that immediate loading is generally discouraged for a single implant and tooth restoration. Should immediate loading be considered, a diminutive tooth that avoids contact during mastication is preferable. This precaution is due to the significant forces exerted upon the lone implant during various oral activities, such as eating, speaking, or chewing gum. Notably, immediate loading in anterior regions carries the highest risk of implant failure. In instances where a T-base is employed, it is imperative to select one equipped with a hex and an anti-rotational feature to prevent rotation between the implant and the T-base. A non-rotating T-base ensures the screw remains secure. Conversely, a round T-base on a single implant may rotate, leading to micro-movements that could loosen the screw, causing the crown to shift. If the crown moves and the patient applies force at an incorrect angle, there is a risk of damaging the implant or breaking the screw within it. Such occurrences can lead to numerous failures and, in some cases, may render the implant irreparable.
How to make a digital impression for a T-base abutment
Our discussion will focus on the methodology employed for capturing dental impressions. Utilizing an intraoral scanner, the dentists meticulously recorded the impressions. The scan abutment’s placement within the oral cavity is discernible, ensuring precision in the impression process.
This particular scenario presents an exemplary opportunity for practitioners to familiarize themselves with the in traoral scanner for restorative procedures. The presence of a complete set of teeth and a solitary scan abutment facilitates a straightforward scanning process, devoid of any interference between the scan abutment and adja cent teeth. Challenges often arise in instances involving a single implant closely positioned to a tooth, where the scan abutment may not fit properly, potentially leading to inaccurate impressions due to contact with the tooth or incorrect angulation of the scan abutment.
For novices utilizing intraoral scanners, this case serves as an ideal learning model. Most scanners, including older models, are capable of capturing impressions for a single implant. The latest scanners further simplify the restoration process through the use of integrated libraries, offering a user-friendly experience in mastering the intraoral scanner.
When capturing impressions for a single implant, it is imperative to perform the procedure at the implant level to ascertain the orientation of the hex. Single-tooth restorations hinge on anti-rotational elements to maintain stability. It is essential to incorporate an anti-rotational element, such as a hex, between the implant and the T-base. This implant features an internal hex, mirrored by the hex in the T-base, and subsequently, an anti-rotational element between the T-base and the crown. Given that the T-base is not uniformly round, anti-rotational elements are crucial between each component. Therefore, when employing a scan abutment, it must be used at the implant level and include a hex to ensure the correct orientation of the screw channel and prevent rotational discrepancies in the restoration.
Presented here is the provisional crown, specifically a PMMA crown, which has been fabricated atop the T-base. Notably, the screw channel traverses centrally through the tooth. The buccal inclination coupled with the tooth’s angulation, which runs parallel to the implant, results in an apparent enlargement of the screw channel. This enlargement is attributed to the elliptical cut of the screw channel. As demonstrated in the left simulation, an angular cut of the screw channel yields an elliptical shape, thereby increasing the surface area of the screw channel. This presents a considerable challenge as it necessitates the concealment of the enlarged screw channel, either by masking or closing, to prevent it from being visible.
In this particular instance, the screw channel is positioned centrally within the tooth. Our objective was to achieve an angulated screw channel; however, due to spatial constraints, angulating it further palatally was not feasible.
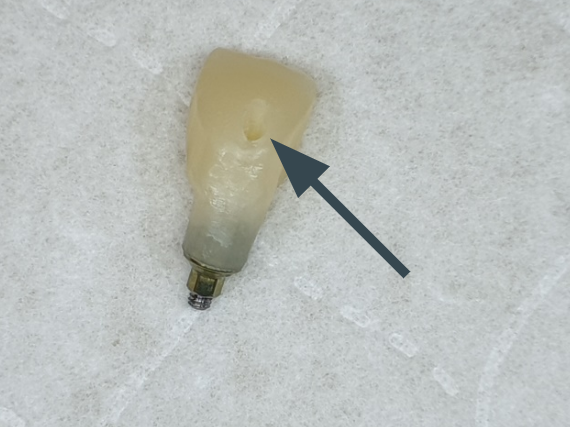
Temporary crown showing the screw shaft
Modeling the exit of the screw channel in the crown
Instead, the dentists opted for buccal angulation, which elevates the screw channel, resulting in a reduced surface cut. This strategic angulation ensures that the screw channel remains unnoticeable in patients with a low smile line, thereby preserving the aesthetic integrity of the restoration.
Over time, the material used to seal the screw channel may require replacement due to potential pigment absorption and minor color alterations. Such changes are inconsequential for patients with a high smile line, as the screw channel is not visible unless the lip is elevated.
Addressing the queries we’ve received about component selection: educational restorations necessitate different parts depending on the case specifics. For instance, T-bases are utilized in certain scenarios, while multi-units are preferred in others. It is essential to discern the appropriate part for each unique restoration challenge.
Multi-unit abutments are designated for bridge cases rather than single crowns due to the absence of anti-rotational elements in straight multi-units. These straight multi-units lack the necessary anti-rotational interface between the abutment and the implant, which could theoretically allow for rotation and subsequent unscrewing.
Conversely, angulated multi-units typically incorporate a hex, providing an anti-rotational element that secures the abutment to the implant, preventing unscrewing. However, the upper portion lacks anti-rotational features, which could lead to the crown unscrewing from the multi-unit. Therefore, T-bases are the exclusive choice for single crowns.
T-bases come in two variants: one with a hex that serves as an anti-rotational element between the implant and the T-base, and another with a round surface that allows rotation relative to the implant. The latter is unsuitable for single crowns but is utilized in cases with parallel implants to construct bridges. Additionally, the T-base design includes a cut on the upper part to accommodate buccal inclination without interfering with the crown’s placement within the dental arch.
The D-type multi-unit is a standard option that accommodates both straight and angulated configurations, allowing for uniform sleeves and screws across different heights.
Returning to our case, the temporary restoration is observed, where the crown color has not achieved the desired perfection. This highlights the importance of precision in both component selection and the restoration process.
The provisional crown, made of PMMA, features a screw channel sealed with composite material. Despite the potential visibility of the screw channel under intense illumi nation, it is designed to be inconspicuous when the patient smiles, ensuring aesthetic harmony.

Finished temporary restoration showing the sealed screw shaft
The strategic positioning of the screw channel buccally, rather than palatally, and its elevation, are deliberate to maintain invisibility even during the patient’s highest smile. The crown’s placement does not align with the arch due to slight interference from the lower teeth; however, the design remains consistent. The intention is to reposition the crown slightly palatally to align the teeth and enhance the aesthetic outcome. This is facilitated by the T-base’s cut corner, which allows for palatal movement of the crown, achieving a level alignment with the adjacent crowns and optimizing the visual appeal. The cornea crown is designed so that the screw channel is nearly imperceptible, further contributing to the restoration’s aesthetic success.

Installed crown where the screw channel is almost invisible
In the forthcoming years, perhaps within a five to tenyear span, it may become necessary to replace the composite material sealing the screw channel. However, for the immediate future, this aspect of the restoration will remain unnoticeable. Even during instances of smiling, the screw channel is designed to be concealed. The final adjustments to the crown, facilitated by the available buccal space, allowed for a palatal shift. This repositioning ensures that both teeth achieve a nearly identical level, enhancing the overall symmetry and aesthetic appeal, despite the original teeth not being on the same plane.
The reflection in the final work subtly reveals that the surface is not perfectly flat, yet this does not detract from thevisual outcome.