Dental Implant Meta-Analyses 2024: From Navigation to Long-Term Survival
This article will examine several meta-analyses published in 2024. Some of these studies confirm findings that practitioners have observed in their own experiences, while others present less intuitive results. For example, attitudes towards antibiotic use in oral surgery have shifted. We sourced these meta-analyses from the PubMed portal, where 62 studies matching the “Dental Implants” query were published in 2024. While the quality of these studies varies, we selected a few of the most significant ones from research groups with established authority.
An Example of Statistical Analysis with Limited Practical Application
Some high-quality studies produce reliable data, but their results are impractical for real-world application. We’ve included one such analysis as an example of how time and resources can be spent in vain, even when all the conditions for a rigorous study seem to be met.
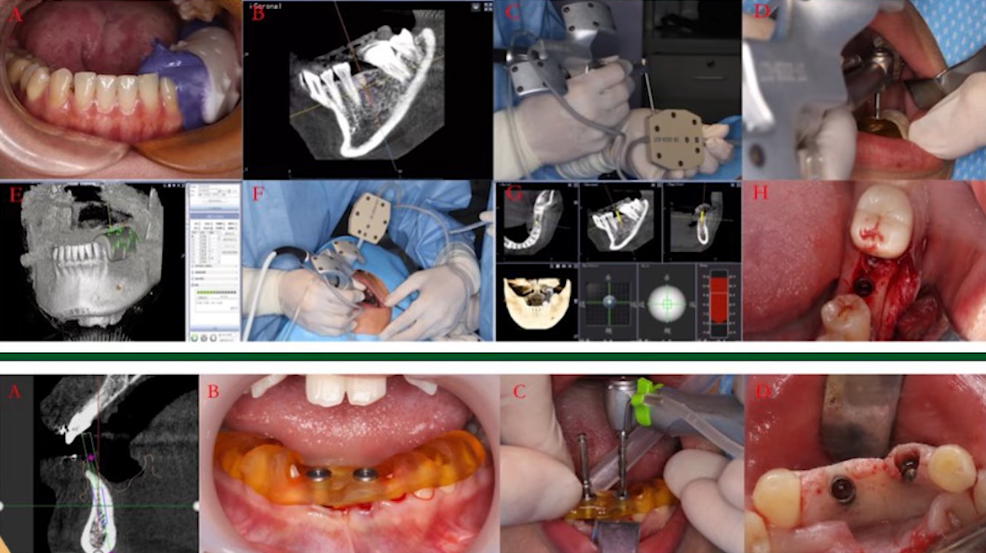
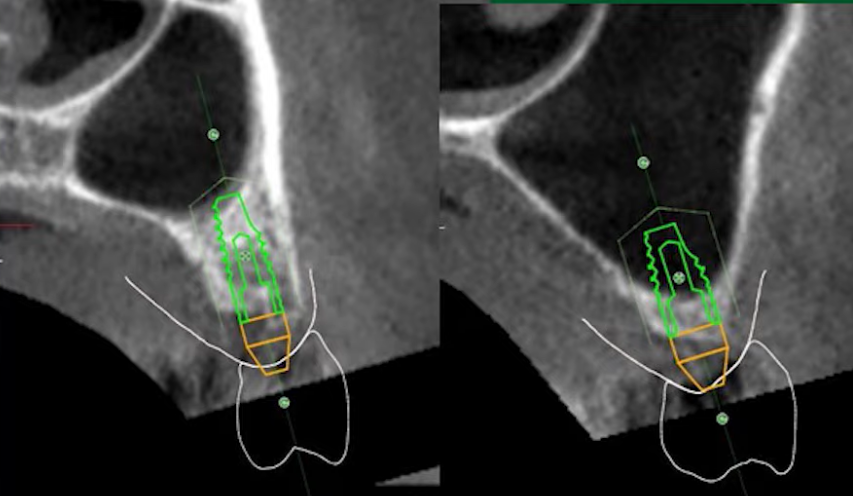
This particular analysis compares dynamic and static navigation in implant placement, aiming to determine which method is superior. The issue here is that nearly all the cited literature and references revolve around specific manufacturers of dynamic navigation equipment. This raises questions about the objectivity of the research.
Here are the findings of that particular meta-analysis:
A total of nine studies were included in the final analysis, comprising four randomized clinical trials and five observational clinical studies. The meta-analysis showed that dynamic computer-assisted implant surgery (dCAIS) significantly reduced implant apical deviation (Mean Difference [MD] = -0.12, 95% Confidence Interval [CI]: -0.23 to -0.02, P = 0.02) and implant depth deviation (MD = 0.20, 95% CI: 0.34 to -0.06, P=0.004) compared with static computer-assisted implant surgery (sCAIS). However, there were no significant differences in implant platform deviation (MD = -0.01, 95% CI: -0.08 to 0.06, P = 0.74) and implant angular deviation (MD = -0.30, 95% CI: -0.78 to 0.18, P = 0.22) between the two methods. Egger’s test revealed no publication bias in the analyzed results (all P > 0.05).
In simpler terms, the conclusions suggest that dynamic navigation is superior to static navigation, but the improvement in accuracy is minimal, primarily affecting implant depth rather than its position relative to the existing dentition.
It’s important to remember that dynamic navigation requires specialized equipment, including sensors and beacons, to track implant position during placement.
The concept behind dynamic navigation is to precisely place the implant in its planned optimal location determined during the initial planning stage. The dentist sees the patient’s anatomical structures on a screen in real-time, with a graphic overlay indicating the planned implant position. The operator can then adjust their actions to minimize any deviation from the planned location.
An alternative to dynamic navigation is implant placement using custom surgical guides (templates). Researchers confirm that static navigation achieves a high level of accuracy.
However, despite the fact that dynamic systems have been available for over a decade, they account for only a small percentage of implantations. Approximately 98% of all implantations are still performed using static navigation techniques.
This demonstrates that the dental community has largely made its choice. Why switch to a complex and costly technique that only offers marginally better results when a well-established technique delivers stable results?
Studies like the one discussed here often face criticism due to potential conflicts of interest and could be interpreted as marketing efforts for dynamic navigation equipment manufacturers.
Readers are encouraged to find and review the original statistical analysis. Now, let’s move on to what we consider to be the top studies of 2024.
4th Place: Comparison of Immediate Implantation into the Socket with and without Periapical Pathology
This excellent study was carried out by colleagues from Lithuania, and despite the fact that this country is very far away, the materials and conclusions of this statistical analysis are valuable for practicing dentists worldwide.
Traditionally, periapical lesions have been considered contraindications for immediate implant placement.
This research team challenged that notion by collecting and analyzing relevant, high-quality studies.
We previously discussed in our article, “Low-Traumatic Tooth Extraction: How to Preserve Hard and Soft Tissues for Immediate Implantation,” that cystic granulomas and similar pathologies are not contraindications to immediate implantation. Experienced surgeons have long known that removing granulation tissue and the cyst membrane allows for safe implant placement. Now, this idea is supported by a comprehensive statistical analysis.
Key Findings:
Within the limitations of this systematic review and meta-analysis, the findings suggest that implants placed immediately in the sockets of extracted teeth with periapical pathology can be successfully osseointegrated over the long term.
We believe that immediate implant placement should be pursued in these cases since it is rare to encounter tooth extractions without some periapical pathology.
3rd Place: Is Routine Antibiotic Prophylaxis Warranted in Dental Implant Surgery to Prevent Early Implant Failure? – A Systematic Review
This excellent work by Swedish specialists changes a lot in how we structure the treatment process.
The study addresses a key question:
The routine use of antibiotic prophylaxis in dental implant surgery remains controversial. Although there is limited strong evidence supporting its use, antibiotics are often prescribed to mitigate the risk of infection, which could lead to early implant failure.
However, increasing antibiotic resistance is a serious concern, highlighting the need to reduce overall antibiotic use, including within dentistry.
This systematic review and meta-analysis aimed to assess the effectiveness of preoperative antibiotics in preventing early implant loss in otherwise healthy patients.
This study is impactful; the list of analyzed articles is notable for both its quantity and quality.
And here are the conclusions the Swedish group of scientists came to:
Based on this review and meta-analysis of high-quality randomized controlled trials (RCTs), the benefit of antibiotic prophylaxis in dental implant surgery is likely very limited. Given increasing antibiotic resistance, antibiotic administration should be avoided in the majority of implantation cases.
The results of this systematic review and meta-analysis may form the foundation for new and more precise clinical guidelines regarding antibiotic prophylaxis in dental implantology.
This is a robust study that demands our attention. It’s likely that protocols for antibiotic use in dentistry will be updated as a result.
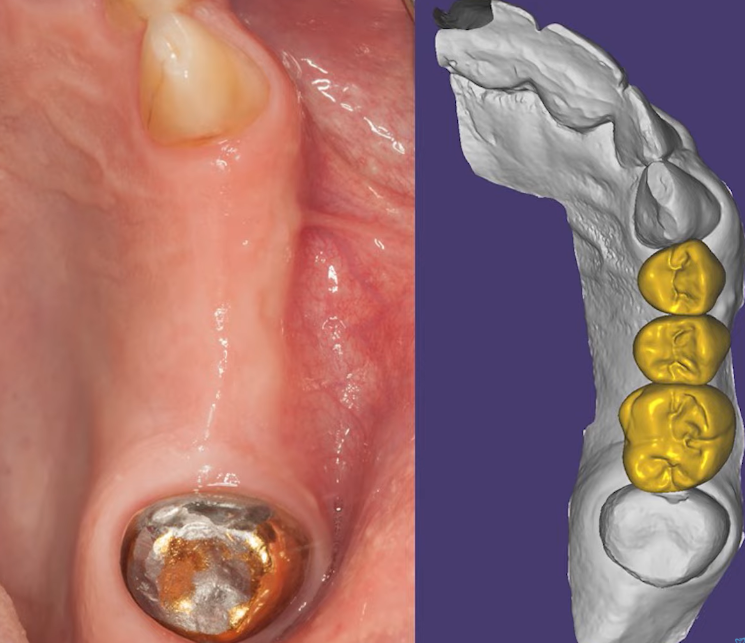
2nd Place: Implant-Supported Fixed Prostheses with Cantilever: A Systematic Review and Meta-Analysis
This topic has sparked many discussions. In most instances, we aim to avoid cantilever structures in prosthetics. Indeed, the use of cantilevers has been identified as a common mistake in implant-supported restorations in the corresponding article. However, cantilevers are often unavoidable. Traditional guidelines often suggest that an anterior cantilever is more acceptable than a posterior one. In terms of length, a cantilever exceeding 15mm is typically discouraged. While cantilevers can shorten the lifespan of restorations, such restorations can be quite successful. This new systematic review offers further insight.
Cantilever structures are most common in full-arch restorations and when there is insufficient space to place an additional support implant. For instance, when two premolars are missing sequentially, a single implant might be placed, with a cantilever prosthesis spanning both teeth. When restoring the area of the fourth premolar, anatomical restrictions, particularly an angled and curved canine root, are commonly encountered. When placing an implant there is a risk of damaging this root.

Damage to the root of an adjacent tooth when placing two implants next to each other Youtube/ Implantarium/ Rauf Aliyev
To mitigate this risk, practitioners frequently utilize the treatment scheme shown below:

Restoration of two teeth supported by one implant with a cantilever prosthesis (premolars) Youtube/ Implantarium/ Rauf Aliyev
These solutions are stable and have a lifespan comparable to single crowns. In this particular study, researchers have examined all types of cantilever structures, with the following results:
Conclusions of the study regarding cantilever structures in prosthetics:
When addressing the question: “Are cantilever structures supported by fixed dentures in dental implant treatment effective in partially edentulous cases compared to conventional fixed dentures?”, the study found that the likelihood of mechanical complications was increased.
However, the likelihood of negative impacts on implant survival, patient satisfaction, and peri-implant bone loss was low.
Implant-supported cantilever prostheses can be beneficial for patients, particularly in cases of insufficient bone tissue or anatomical restrictions where bone grafting would be required.
Notably, additional clinical data are needed regarding the influence of the number of implants, cantilever length, and differences between mesial and distal cantilevers.
Therefore, if the choice is between performing bone grafting and placing two implants or opting for a single implant and a cantilever prosthesis, the cantilever approach is a reasonable option.
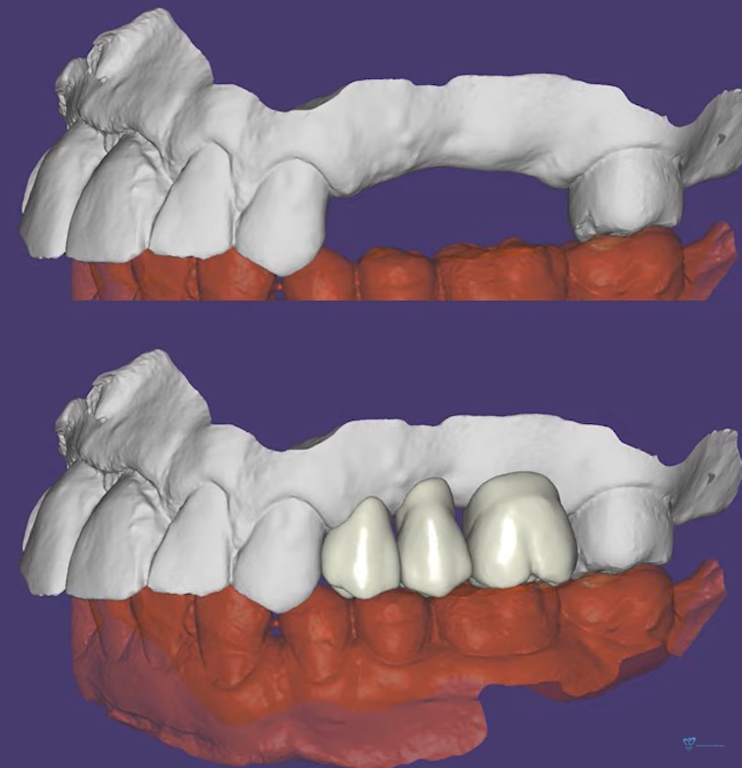
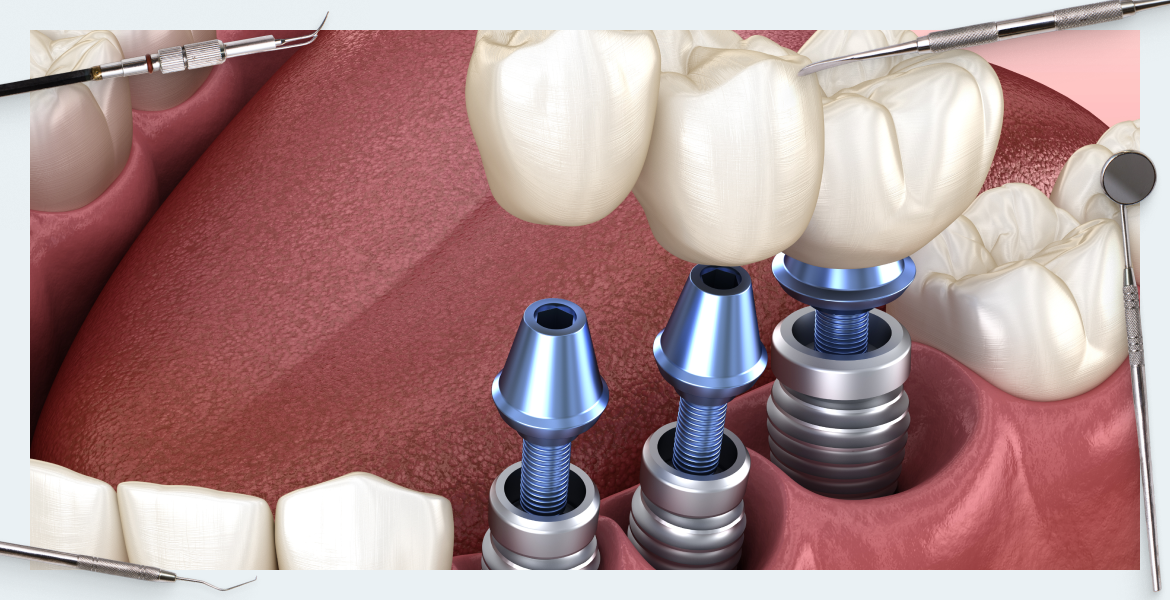
Let’s consider another example. A patient presents with a fractured tooth; previous prosthesis caused an overload.
In addition to the root fracture, there is notable bone loss around the problematic tooth.
All teeth were extracted, and after healing, the patient sought restorative treatment.
Condition of the jaw after complete healing and model of the prosthesis Youtube/ Implantarium/ Rauf Aliyev
Given this situation, it is logical to consider installing implants in the areas of the 24th and 26th teeth.
However, on a tomogram, it’s clear that the canine root is angled, which necessitates positioning the implant more towards the 25th tooth.
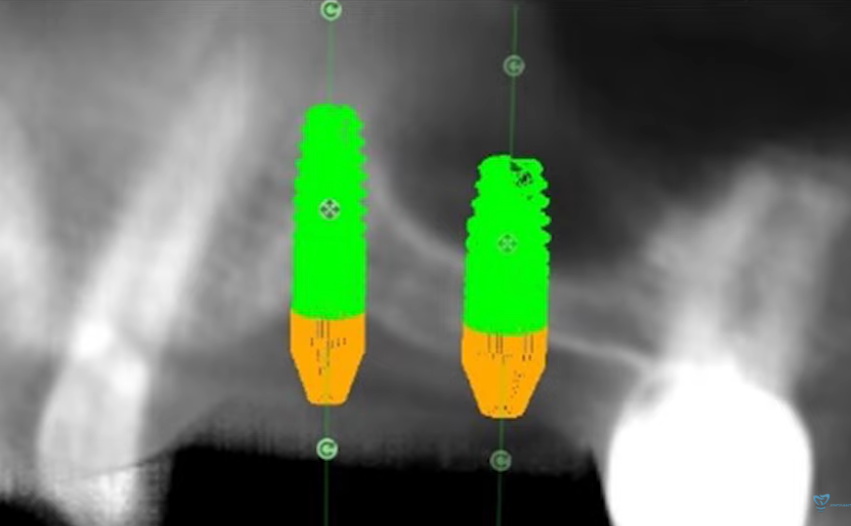
Planning the placement of implants taking into account the location of the roots of adjacent teeth Youtube/ Implantarium/ Rauf Aliyev
The treatment was implemented accordingly, as seen in the x-ray below. The final prosthesis has a cantilever extending towards the canine, however, the restoration is both aesthetically pleasing and highly functional.
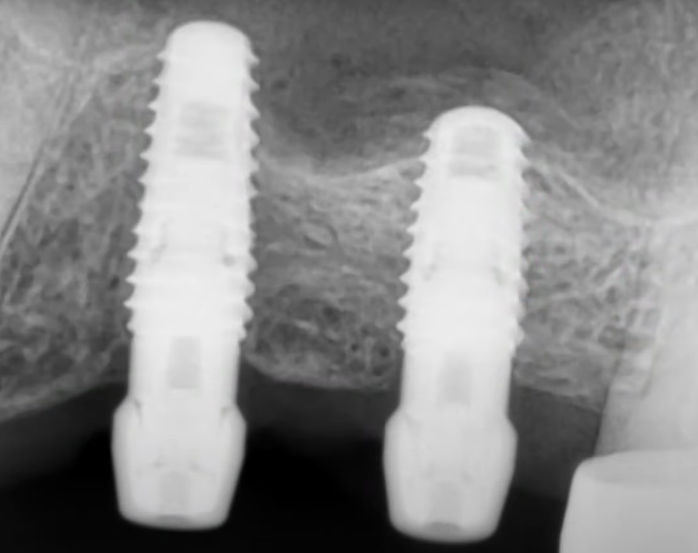
Implants on which the cantilever structure will rest were placed as planned Youtube/Implantarium/Rauf Aliyev
1st Place: How Far Can We Go? A 20-Year Meta-Analysis of Dental Implant Survival Rates
This work by German colleagues is exceptionally well-conducted and clearly presented. To date, there have not been prior meta-analyses based on 20-year observations. This study, therefore, is truly ground-breaking and deserves the top spot.
Findings:
Three prospective studies (n=237 implants) showed a mean implant survival rate of 92% (95% Confidence Interval [CI]: 82% to 97%), decreasing to 78% (95% CI: 74% to 82%) after replacement (n=422 implants). A total of five retrospective studies (n=1440 implants) showed a survival rate of 88% (95% CI: 78-94%). The reasons for implant loss were multifactorial.
These findings demonstrate that implant loss over the long term is influenced by multiple factors. Key causes of loss included periodontitis, diabetes, and smoking.
The German research team emphasized the importance of patient monitoring for long-term success. Many specialists have seen that patients generally attend follow-up appointments regularly during the first year post-prosthetics. Attendance then becomes less frequent in the following 3-4 years. After that, the most diligent patients may attend once every 1.5-2 years; however, after ten years, many stop coming entirely. Patients often forget the pain, problems, and financial investment they incurred to receive new teeth. When they feel healthy, patients are less likely to seek care from a dentist until a problem arises.
This study found that problems can develop after 7 or 10 years, even in the absence of previous complications. Routine examinations and professional hygiene care of the restoration can significantly increase the long-term survival of implants. Dentists must stress the crucial importance of preventive examinations.
Despite these challenges, this study provides encouraging news as it shows that long-term implant survival rates are high.
Let’s review the study’s conclusion and clinical relevance:
Conclusion:
This review summarizes 20 years of dental implant survival data, highlighting a remarkable success rate of four out of five implants. This figure underscores the need for ongoing follow-up care given that implant losses are multifactorial. Prioritizing quality standards is essential to avoid overestimating treatment effectiveness due to potential statistical errors. Although dental implantology is a reliable treatment modality, there is always room for improvement, including further high-quality research to assess implant success.
Clinical relevance:
This is the first meta-analysis that has systematically analyzed 20-year dental implant survival data. While long-term survival can be anticipated, follow-up care is imperative and should not cease after the implant placement, even after ten years.
Now, there is a scientific basis to answer patients’ questions regarding the reliability and longevity of dental implants. Even if a practitioner is relatively new to the field and doesn’t have years of follow-up experience, the scientific data supports this area of clinical practice.
That’s all for now; stay tuned for future publications.