Periodontal Treatment vs. Implant Placement: Comparing the Success Prognosis of Both Approaches

In our previous articles on comparing implantation treatment to save a living tooth, we looked at the statistics for endodontic treatment versus implantation. Before that, we looked at how a dental implant differs from a living tooth in terms of functionality. In this article we will look into whether implants can solve the problem of periodontitis once and for all, how and why periodontitis affects the prognosis of implant treatment, what role does dental hygiene and cleaning play and how effective is periodontitis treatment and what are the chances of saving teeth in the long run.
What is periodontitis?
Let’s start with definitions. Periodontitis is an inflammatory disease of the supporting tissue complex, particularly the periodontium.
To be precise, periodontitis is an inflammatory disease of the surrounding and supporting tissues, both soft and hard tissues. The inflammatory process is associated with biofilm, that is, microorganisms attached to the root surface.
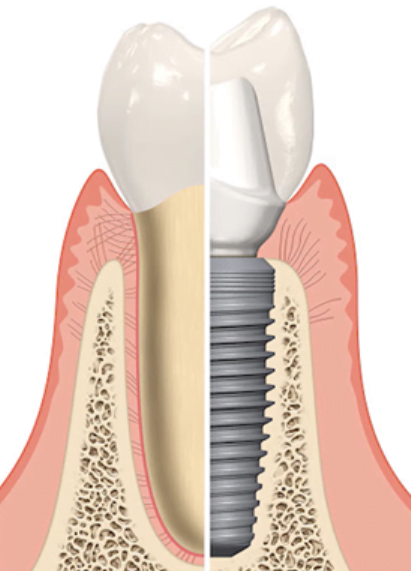
It is very important to understand the key influence of the microbiota on the development of periodontal disease. After all, if we look at teeth and dental implants, we see that they penetrate the soft tissues and the upper part of the tooth (like the crown placed on the implant) is in the non-sterile area of the mouth, while the tooth root or dental implant enters the sterile environment of the alveolar bone and the surrounding soft tissue.
Teeth are a unique organ, nowhere else in the body is there direct penetration through the soft tissues.
Wherever the body comes into contact with an aggressive (non-sterile) environment, be it the atmosphere, liquids or food, there is protection in the form of mucous membranes, or keratinized epithelium. These are the skin, the conjunctiva and cornea of the eye, the mucous membranes of the mouth, intestines, etc.
It is known that the entire surface of the human body is contaminated with a huge number of bacteria, viruses and fungi. Not all of them are dangerous and can cause diseases, but there are many pathogenic microorganisms. Nevertheless, the internal environment of the human body remains sterile.
There are a lot of microbiota in the oral cavity, and the hardest part is that the teeth are the only organ that penetrates the covering tissue and passes from a sterile environment to a non-sterile one.
When a person is healthy, the periodontium, which includes a complex of soft tissues (gingival cuff, periodontium, alveolar bone), serves as a protective barrier. Periodontal tissues also provide an immune response, not allowing the biological film to overdevelop and penetrate the sterile environment and thereby cause an inflammatory process.
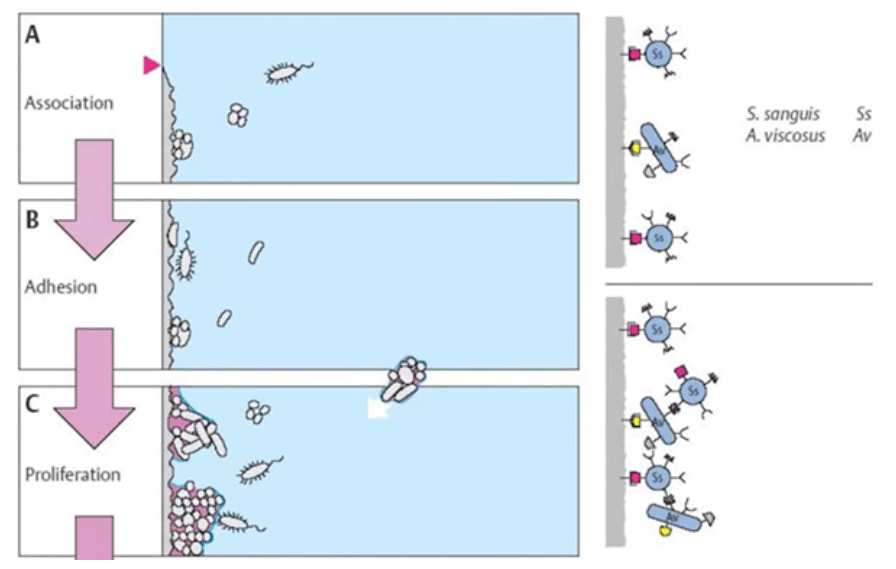
It is also known that both the newly erupted tooth and the newly placed dental prosthesis are covered by a thin film (pellicle) of proteins and polysaccharides during the first minutes. Microorganisms are immediately fixed on this film.
Based on the data obtained, it is clear that the trigger for periodontitis is changes in the composition of the microbiota, as well as changes in the body’s response to these dysbiotic shifts.
Moreover, caries and gingivitis are also caused by the activities of bacteria; different areas are dominated by different bacteria.
For example, if we take the microorganisms that are contained in the subgingival calculus and infest the gingival groove, it appears that it is dominated by Gram-negative and Grampositive bacteria, which are mostly obligate anaerobes. That is, they prefer an environment with minimal oxygen content.
This is an important point for understanding the causes of periodontal disease. If the microorganisms that cause inflammation are obligate anaerobes, then they must somehow obtain an oxygen-free environment. This is only possible if a bacterial film of considerable thickness is formed.
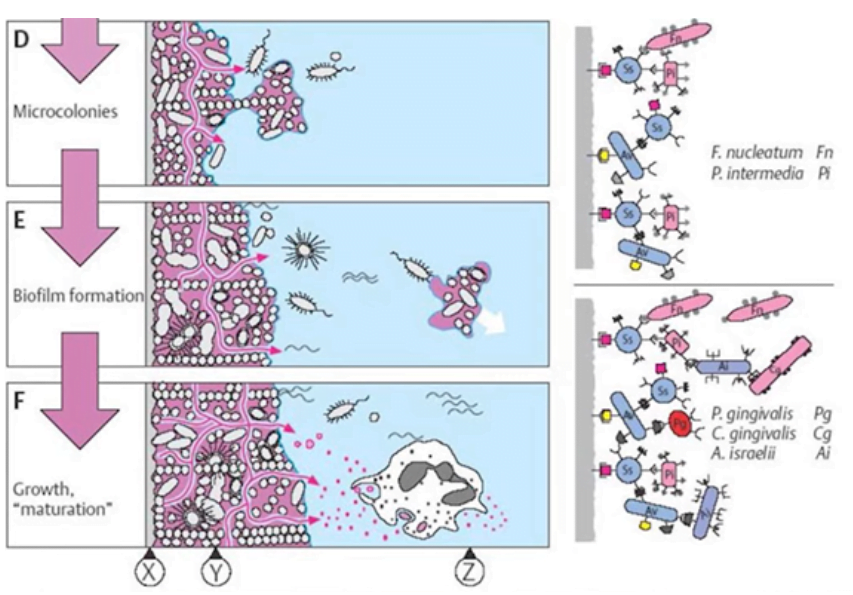
To understand the process, we will use an illustration from Lande and Linde’s book, sixth edition, 2015.
We see that at the very beginning, a pellicle is formed on the surface, and very quickly bacteria begin to attach to it. At first, these are mostly aerobic types of microorganisms.
As the biofilm thickens and matures, obligate anaerobes appear in its depth and eventually begin to dominate.
The key factors for the onset of periodontal disease are:
- The presence of a fairly thick biofilm on the surface of the tooth, and especially in the area of the gingival groove. This is why oral hygiene is so important, including professional tooth brushing to remove plaque and tartar.
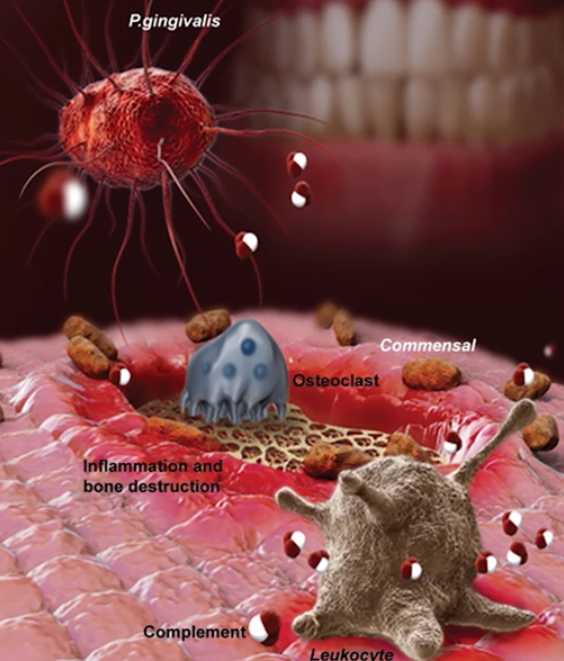
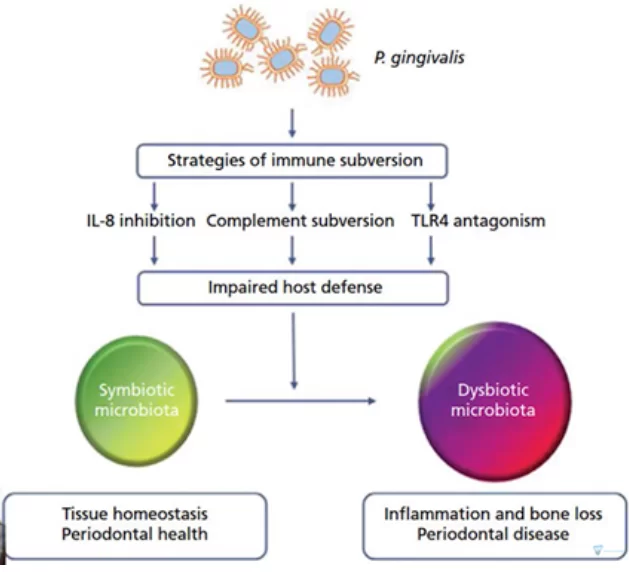
- The bacterium Porphyromonas gingivalis, which starts a chain reaction in the presence of a thick biofilm, is vital.
It is notable that this bacterium and its products of activity are not so dangerous on their own. There are more dangerous and destructive microorganisms in the biofilm, such as spirochaetes and actinomycetes, but it is Porphyromonas gingivalis, the “saboteur”, that makes a hole in the immune defense and starts the process of uncontrolled inflammation.
The antigens and other substances that Porphyromonas gingivalis secretes affect the cellular and humoral response of white blood cells. These substances also have a direct effect on bone tissue. Porphyromonas gingivalis essentially changes the immune response and the body’s response to this bacterial invasion. On the background of an insufficient immune response, other microorganisms are also actively developing and causing inflammation and tissue damage.
We also know that titers of Porphyromonas gingivalis bacteria exist in every person, but not all patients who do not brush their teeth regularly suffer from periodontal disease. For example, children never have periodontitis. Which means there are quite a few situations where the body gives off an adequate immune response. For an imbalance in the microbiota there must be certain conditions.
There are several riskfactors affecting the likelihood of developing periodontal disease to varying degrees:
- Age – the older a person is, the higher the risk. We know enough older patients who have never experienced a periodontal problem.
- Genetic predisposition has a noticeable impact. However, it’s also quite common that people don’t get the disease even though both parents had periodontal problems.
- Violations of hygiene regimen are a must, but not a determining factor. There must be both a substrate and enough time for pathogens to develop and the right concentration to mature. With perfect oral hygiene, the risk of developing periodontal disease is vanishingly small.
- Smoking cigarettes greatly affects the risk of developing inflammatory processes. Especially if years of smoking are superimposed on a genetic predisposition. This does not mean that people who smoke will necessarily get periodontitis. With proper oral hygiene, they won’t have any problems. Several risk factors must come together.
- Diabetes is a complex disease that is detrimental to all body systems and the oral cavity is a special risk group. Even so, it is not a verdict; with proper oral hygiene, periodontal disease will not develop. If proper care is not taken, the risk of developing periodontal disease increases many times over and the course of the disease will be much more severe.
All of the above says that the main risk factor is biofilm. The main task of periodontists is prevention, which is to teach the patient how to properly care for his or her mouth, using not only a toothbrush, but also brushes and other cleaning products. The patient should learn to remove the biofilm on their own twice a day.
To summarize what we discovered: It takes a combination of several factors for periodontitis to develop, whether it’s the first attack or an exacerbation of chronic periodontitis. The most severe risk factors are smoking and diabetes, also in the risk group are patients of advanced age and with genetic predisposition. The main one is the substrate in which the pathogenic bacteria will multiply. The presence of a thick layer of biofilm and gradual changes in bacterial cultures are the trigger for the development or exacerbation of periodontitis.
How gum infection and inflammation affect the prognosis of any treatment
This article could be finished very quickly without even going into the details of the biological processes. Suffice it to cite the results of one of the most in-depth and qualitative studies. The data from this study suggests that the prognosis of success and survival rates for treated teeth and implants are commensurate. Professionals are, however, always short of unequivocal answers; they need to know why this is the case and what affects the outcome.
Back to the study, which was conducted by a team of specialists led by Italian periodontist Professor Giulio Rasperini, in collaboration with the University of Bern, Professor Giovanni Salvi and other colleagues.
They followed two groups of patients for 10 years. They enrolled 60 patients with implants and periodontal problems and 60 patients with implants but without periodontal problems. All implants were placed in the area of single defects, that is, surrounded by teeth on both sides.
These patients were monitored for 10 years and underwent quality periodontal control and hygienic measures.
These are the results obtained by the research team:
| 10-year survival rate | Patients with periodontitis 60 clinical cases | Patients without periodontitis 60 clinical cases |
|
Teeth |
100% | 100% |
| Implants | 80% |
95% |
As we can see in the case of adequate treatment and hygienic care, it was possible to save all teeth even in patients who had periodontal problems.
However, in the case of implants, the survival rate in patients with periodontal problems was noticeably lower, although the difference was not critical.
If there is a difference, there are reasons that cause it. So let’s take a closer look at what was going on in the implant-dental area and where the reason for the lower implant survival rate in patients with initial periodontal problems lies.
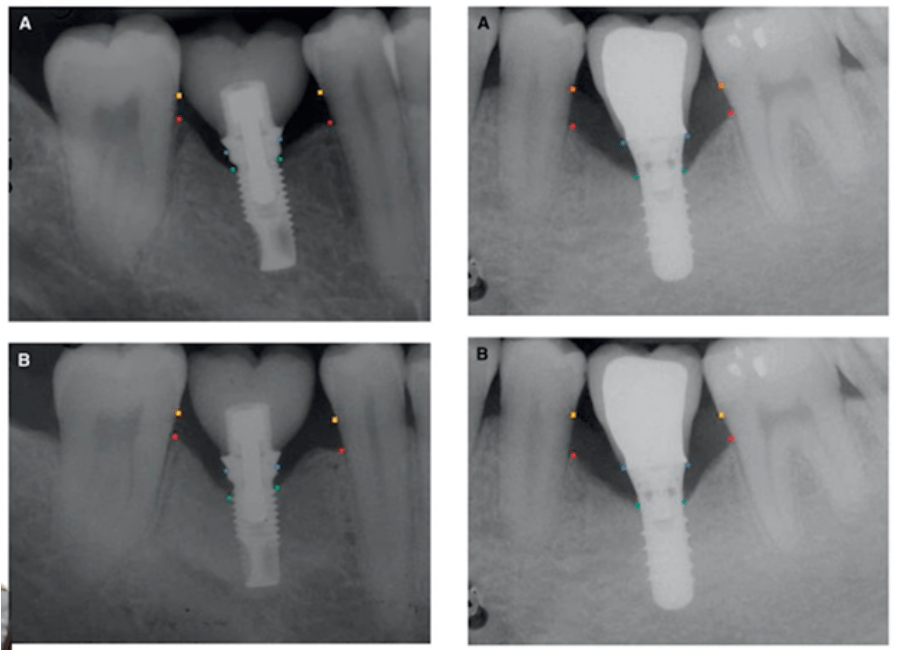
During the study, experts measured the height of the alveolar bone, measured the cement-enamel junction and the height of the bone peak in the implant area. All this was done using standardized radiographs.
Two different Branemark and Straumann dental implant systems were used for the study.
These are the conclusions from an in-depth study:
- Bone loss due to resorption is always less around the teeth compared to implants over the entire 10-year follow-up period. Whether the patient suffered from periodontal problems or not. In numbers, this difference looks like this:
– Teeth – bone ridge height loss 0.44±0.23 mm;
– implants 2.28±0.72 mm.
Therefore, provided that periodontal disease has been treated with a prophylactic hygiene regimen, the long-term prognosis for teeth is at least as favorable as that for dental implants. These observations are also true for teeth with reduced periodontal support. Therefore, great caution should be exercised when prescribing tooth extraction with periodontal problems in favor of implants. Yes, when implanting into bone that has been subjected to an inflammatory process, the risk of implant loss is slightly higher, but the prognosis for successful survival is also quite high. - Smoking cigarettes is extremely detrimental in the long run to the survival rate of both teeth and dental implants.
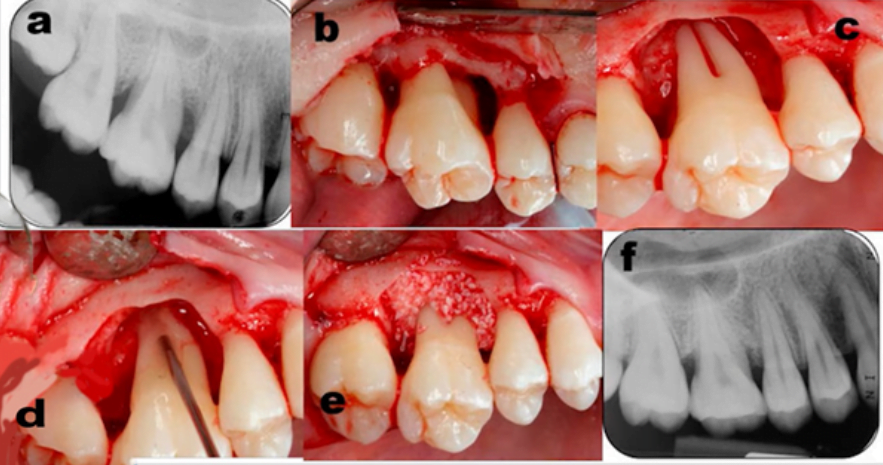
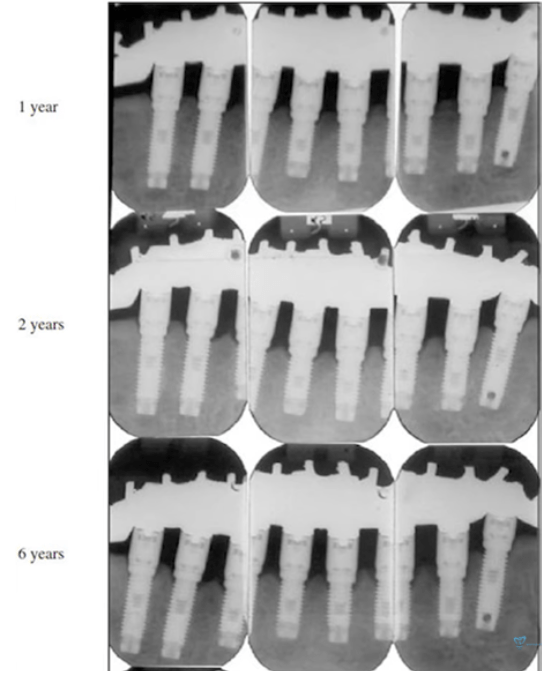
Before implantation became widespread, techniques were developed that allowed successful treatment of periodontal problems. With proper care and patient education, it was possible to save teeth. Moreover, it was possible to observe bone and soft tissue recovery, see images below.
Even very difficult cases have been successful, see pictures below. There are many long-term studies that show that periodontitis is not a verdict and in many cases success can be achieved in the long run of a decade or more.
Unfortunately, there is a recent trend that if the problem is a little more serious than a cavity, dentists suggest extracting the tooth and placing an implant.
What happens in periodontitis and can almost hopeless cases be treated?
Let’s look at a specific clinical case. Here is an image of a patient who was still quite young (about 40 years old), somatically healthy, but his medical history was aggravated by smoking at the time of treatment.
The picture is depressing, and seeing this clinical situation, all the arguments about trying to save teeth and treating the patient break like waves against rocks.
It would seem that in such cases there is nothing left to save and a full restoration on implants is needed. For example, all on 6® or all on 4®.
However, as we mentioned in an earlier article comparing the prognosis of dental and implant survival, that dental treatment and implants are not competing technologies, but complementary. Here is a sample study that confirms this.
Implants are a great method of restoration when a tooth is already missing, but if a tooth is present, it should only be removed if all other treatments have failed.
To return to our clinical case, we have a chronic form of periodontitis with pus and extensive pockets.
As we already know, periodontitis cannot progress without a substrate in which pathogenic microflora develop. From these facts, a controversial concept was born. If periodontal disease is a disease of the tissues that support the tooth, then if there is no tooth, there is no problem. This concept has permeated the dental community and prescribing extractions has become much more common than necessary.
Let’s look at the weaknesses of this, we would say, harmful concept. Indeed, if all the teeth are extracted and no implants are placed, you can forget about periodontal disease forever. However, the whole point of treatment is to restore the dentition. It doesn’t matter if it’s dental and soft tissue treatment or placement of dental implants.
If a patient with periodontitis gets implants, but doesn’t change his habits and lifestyle, he will develop peri-implantitis within a short period of time and with no less intensity than before he suffered from periodontitis.
Although these are different diseases and the treatment approach is also different, the prognosis for periimplantitis is much worse than for periodontitis.
A large number of studies support this concept. We can find early studies when roughened implants were not yet used. A milled surface is known to be less prone to biofilm formation due to its smoothness, but the result is the same. Studies have confirmed time and time again that if a patient had a history of periodontitis and did not have proper oral control and regular biofilm removal, sooner or later the patient would develop peri-implantitis.
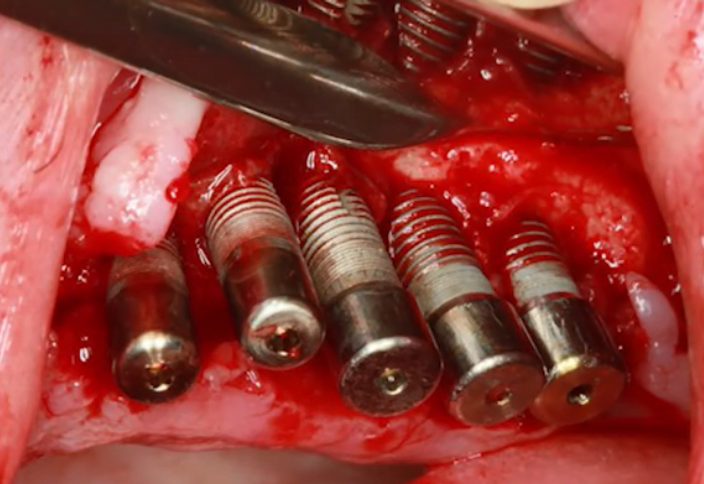
Here are the results of one of the best studies from Drs. Bergland, Lekholm and colleagues:
This group studied patients over a period of 10, 15 and in some clinics 20 years who had all their teeth extracted and had dental implants and fixed dental restorations placed.
As a result, it was found that:
- The percentage of implant loss in patients with a history of periodontitis was much higher.
- Some of the successful cases where everything was fine in the first 6-7 years lost up to 50% of bone ridge height in the next 5-7 years, see pictures below. Many dentists know from experience about this 6-9 year cut-off after which a whole cascade of problems with previously quite successful implants occurs.
You have to understand one simple thing, with the removal of the teeth the microflora did not go anywhere. Everything that was in the mouth in the form of biofilm on the teeth especially in the root zone also develops well on implants, crowns and abutments with the same rate of intensity and consequences.
There is also an opinion that if you remove all the teeth, wait until the mucosa is completely healed and only then place the implants, you can avoid problems with inflammation of the bones and soft tissues. However, that’s not the case either as another study by the Bern School refutes this concept.
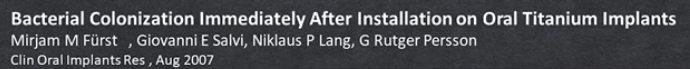
Researchers on patients (in vivo) found that all of the same microbiota that causes periodontitis were on the implant surface within 30 minutes of the implant completion.
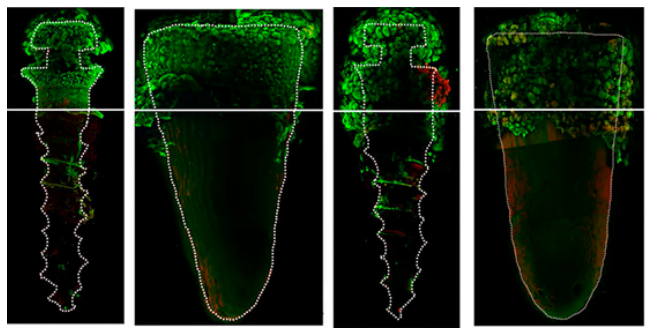
Not only that, there is another demonstrable study that shows the intensity of biofilm development on the titanium implant and tooth.
The study was conducted in vitro, but otherwise it would not have been possible to see all the processes so clearly. A titanium micro-implant and a fragment of an extracted tooth were chosen for comparison. A certain analog of the epithelium was created, and the oral environment was reproduced as closely as possible. An electron microscope was used to observe how the biofilm structure changed over time. The illustrations below show that in the first 24 hours, the biofilm developed more actively on the tooth fragment. However, after 48 hours (right pair of pictures) you can see that the intensity of microflora development on the titanium implant overtakes the natural tooth, including the depth of biofilm penetration below the conventional gingival level. Therefore, implants must be cared for much more carefully than teeth.
Some patients believe that replacing teeth with implants will solve all problems and that dentures do not need to be cared for. Often it was poor care that led to tooth loss, and if the patient does not change his habits, he will face more problems in the form of peri-implantitis.
Let’s return to our clinical case, when there seemed to be nothing left to save and implants were needed.
In consultation with the patient, a treatment regimen was established with all of the above information in mind. What we had at the beginning:
- The patient is fairly young and somatically healthy.
- There is a significant periodontitis lesion with pus.
- Mobility of all teeth is in the 3rd-4th degree.
- His medical history is complicated by smoking.
The first thing to do is to convince the patient to stop smoking. As we already know, it is one of the leading risk factors. In this case, smoking aggravates the course of the disease, but in this case, the patient has given up smoking.
The good news is that quitting smoking is possible and the body will respond positively quite quickly. In any case, quitting smoking is a solvable problem, unlike diabetes. In this case, too, it is possible to adjust the puncture treatment and reduce the impact of diabetes on the course of inflammation.
Also in many studies it was noted that against the background of chronic stress, exacerbation of the course of periodontitis was observed. Therefore, it is definitely necessary to draw the patient’s attention to this and possibly recommend working with a psychotherapist.
The second important factor is oral hygiene. It is necessary to carry out explanatory work. Teach the patient how to take care of his teeth. The main thing is to make sure that the patient understands why to do it and knows how to do it correctly. In this case, success was achieved with this patient.
In general, in the modern world, hygiene is more or less good only in the developed countries of Europe, the United States and developed Asian countries such as China, South Korea, etc. For the majority of the population hygiene is not only inaccessible, there is no explanatory and educational work.
Even in developed countries, we need hygienists and periodontists to be the first to meet patients. Observe them from childhood, long before any problems occur so we don’t have to discuss the cost of this or that implant platform.
Back to our patient. Smoking cessation, good and regular dental hygiene as well as supportive treatment helped to get rid of tooth mobility, eliminate inflammatory processes and a few months later did a dental restoration. You can see the result in the picture below.
To summarize:
- If we are dealing with teeth affected by periodontitis, we are extremely likely to get implants with a peri-implant problem if we don’t get the periodontitis under control before we remove the tooth.
Of course in advanced cases immediate extraction of the tooth is necessary. So we need to work with patients in the time between extraction and placement of the dental implant. - If you take the biofilm development under control and prevent the development of dysbiosis, it does not matter as much what method of restoration will be chosen in the future, crowns or implants. The chances of successful treatment in the long-term increase dramatically.
We hope you found this article interesting. We also want to point out that we have articles available in our ‘tooth extraction’ section. Until future publications.