How to evaluate primary implant stability: innovations and prospects
Today, we will briefly introduce a study from a group of Swiss researchers published in Clinical Oral Implants Research by Wiley. The study aims to improve methods for assessing preoperative primary stability (PS). Current techniques, such as implant insertion torque (IT) measurement and resonance frequency analysis (RFA), have shown limitations in accuracy, particularly when dealing with heterogeneous bone structures. Therefore, the researchers decided to investigate how to assess bone quality and predict the level of primary stability more effectively.
What is primary implant stability?
Primary stability (PS) is the ability of a dental implant to remain motionless immediately after placement, before the onset of osseointegration. Simply put, it represents the initial bone-to-implant contact; this contact is either reliable, providing retention, or it is not.
This characteristic is critical to the success of implantation, especially in modern immediate loading protocols, where a crown is installed almost immediately after implant placement.
Primary stability determines whether the implant will withstand masticatory forces in the first weeks after surgery or fail, leading to the failure of the entire procedure.
Clinically, PS is related to the density, volume, and structure of the bone surrounding the implant, as well as to the characteristics of the implant itself, including its shape, surface, and retention system.
Why predicting the level of primary stability is critical for implant success
Imagine trying to drive a nail into wood versus sand. A nail holds firmly in wood but not in sand. The same principle applies to implants: the denser and more structured the bone, the higher the chances of a successful procedure.
Insufficient primary stability can lead to:
- Micromovements of the implant, interfering with osseointegration.
- The need to convert immediate loading to delayed loading.
- An increased risk of inflammation and rejection.
High PS, on the other hand, allows for:
- Faster restoration of aesthetics and chewing function.
- Fewer treatment steps.
- Increased patient satisfaction.
Qualitative PS assessment prior to surgery allows clinicians to plan more effectively: selecting the appropriate implants, modifying the drilling protocol, and even refraining from immediate loading if the risks are too high.
Why classical methods for assessing stability are insufficient
Classical methods: subjective assessments, IT, and RFA
Currently, PS is typically assessed using three main methods:
- Implant Insertion Torque (IT): Measurement of the force required to screw in the implant.
- Resonance Frequency Analysis (RFA): Measurement of the vibration characteristics of the installed implant.
- Subjective Bone Assessment: Based on cone-beam computed tomography (CBCT) scans and the surgeon’s tactile sensation.
These methods provide an indication of stability, but they are applied after the implant is already placed, and they have other disadvantages:
- IT is highly dependent on the type of implant and drilling protocol used.
- RFA is influenced by implant shape and superstructure design.
- Subjective assessments by clinicians are often inconsistent and dependent on experience.
Thus, classical methods do not always provide an objective, reproducible, and reliable assessment of PS.
Limitations of classical methods in real-world practice
The situation is further complicated by the fact that:
- Different implant manufacturers use different IT and RFA scales.
- Patients have varying anatomical features, ranging from dense cortical bone to loose cancellous bone.
- Even within the same jaw, bone density can vary significantly.
Bottom line: clinicians often have to make decisions based on intuition, which increases the risk of errors and complications.
Therefore, the search continues for methods that allow assessment of potential primary stability before the procedure begins.
What the new study says
How the experiment was conducted
Scientists from Switzerland investigated whether it is possible to predict primary stability with high accuracy before implant placement.
To do this, they conducted a unique experiment:
- Samples of human jawbone were taken (from donors aged 82 and 86 years).
- Implants were placed in pre-selected areas using standard protocols.
- A series of mechanical tests were conducted to objectively measure the force that an implant can withstand before losing contact with the bone.
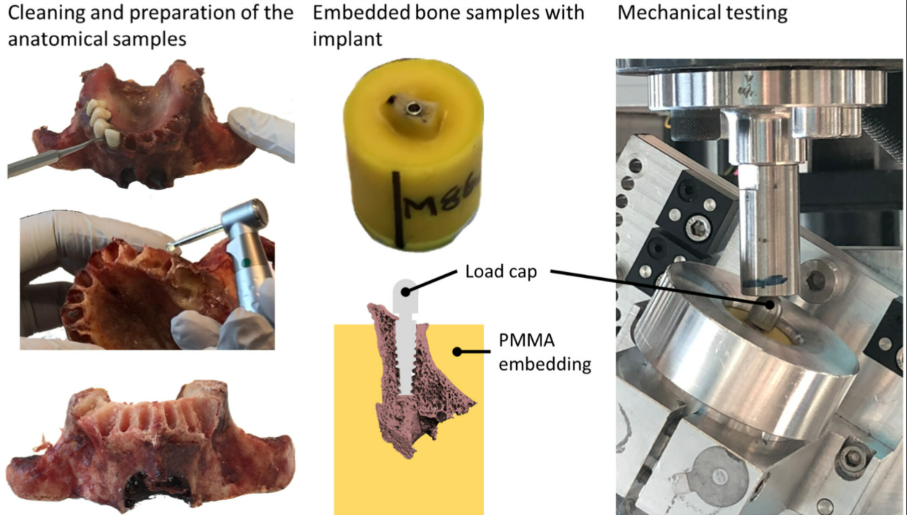
Left: Tooth extraction and flattening by milling of the anatomical samples, when a tooth has been extracted. Middle: In PMMA embedded bone sample that did not require milling. After pilot drilling, the anatomical samples were cut in segments for each implant site and embedded in PMMA, for final drilling, implant placement, and mechanical testing. Right: Setup of the mechanical tests /Clinical Oral Implants Research Wiley/ Patric Wili /clr 14386 /December 2024
- In parallel, computer models (Homogenized Finite Element Analysis – hFE) were built based on µCT scans to predict stability before placement.
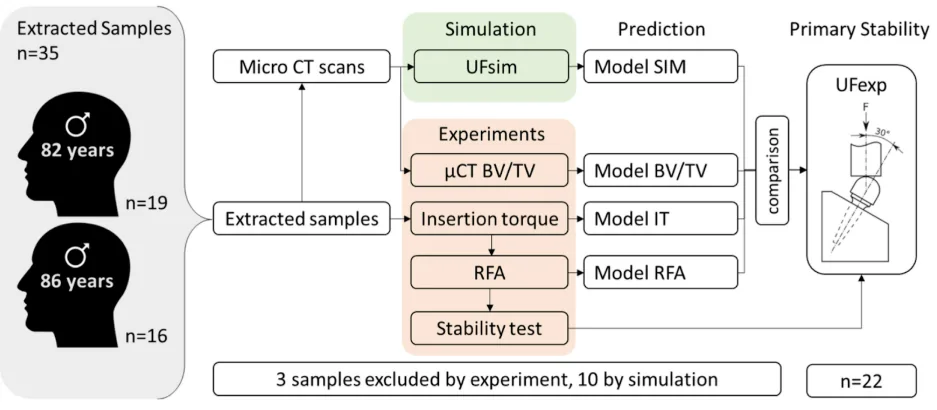
Overview of the sequence steps performed from the extracted samples of an 82-year-old human jaw (n = 19) and an 86-year-old human jaw (n = 16): from extractions and μCT scan, to experimental test and simulation prediction of primary stability. Only n = 22 samples were valid for prediction as 3 samples had to be excluded by the experiment and 10 by simulation /Clinical Oral Implants Research Wiley/ Patric Wili /clr 14386 /December 2024
What materials and methods were used
Main stages of work:
- Micro-computed tomography (µCT) to quantify bone tissue density (BV/TV) in the samples.
- Placement of implants, recording IT and RFA values.
- Mechanical loading of implants according to the modified ISO 14801 standard, defining the Ultimate Force (UFexp).
- hFE analysis for predictive failure force calculation (UFsim).
Technical details:
- NobelActive implants (3.5 mm × 13 mm) were used.
- The drilling sequence was strictly standardized.
- Mechanical tests were performed in several load directions.
Key findings: What will change your practice
New reliable UFsim metric
The results were impressive:
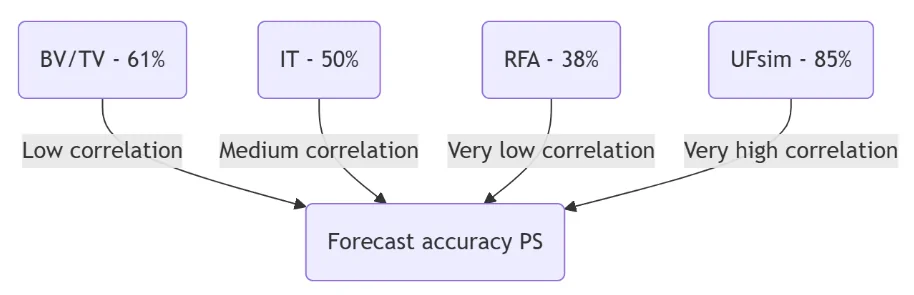
The estimated fracture force (UFsim) showed a very high correlation with the actual experimental force (UFexp), with a coefficient of determination R² = 0.85!
In contrast, classical parameters such as:
- BV/TV
- IT
- RFA
showed significantly weaker relationships with actual stability.
Specific correlation numbers:
| Parameter | R² (correlation with real stability) |
| UFsim | 0.85 |
| BV/TV | 0.61 |
| IT | 0.50 |
| RFA | 0.38 |
Conclusion: hFE simulation based on µCT provides the most accurate PS prediction to date.
Comparison of UFsim with BV/TV, IT and RFA
The study also found:
- A high IT value does not necessarily guarantee high stability.
- RFA varies significantly depending on anatomy and implant.
- BV/TV is a useful guide, but can be misleading if other factors are not considered.
However, UFsim takes everything into account:
- Real bone architecture.
- Drilling geometry.
- Physical properties of the material.
Therefore, its accuracy is almost twice as high as that of traditional methods.
Diagram: visual comparison of the accuracy of the methods
Why is this important for every practicing dentist?
How to use this data when planning implantation
Knowing that UFsim based on µCT analysis provides the most accurate assessment of primary stability, clinicians can reconsider their approach to implant planning.
What this means for your practice:
- When planning immediate loading, clinicians can rely on objective calculations rather than subjective feelings.
- The choice of implant design and drilling protocol can be made more consciously, tailored to the specific patient.
- It is possible to predict in advance where a modified osteotomy protocol (e.g., wall resurfacing or use of osteotomes) will be required.
This technology makes treatment safer, more predictable and personalized.
Advice for practicing dentists
- Use CBCT to assess bone density during the initial consultation.
- Pay attention to areas with low BV/TV; careful preparation of the implant site is especially important there.
- If you have access to automated programs for calculating UFsim using CBCT data, integrate them into your planning process.
- Don’t rely solely on IT or RFA; consider them as supporting metrics, not the only measures of stability.
- If stability values are questionable, consider a delayed loading protocol and provide a gentle rehabilitation regime.
Benefits of the new approach in practice
Table: comparison of stability assessment methods
| Assessment method | Advantages | Restrictions |
| Insertion Torque (IT) | Quick measurement | Depends on the implant system, difficult to compare |
| Resonance Frequency Analysis (RFA) | Convenient for monitoring after placement | High variability, weak correlation |
| BV/TV (bone density) | Helps to choose implant position | Does not account for geometry and bone-to-implant contact |
| UFsim (hFE analysis) | Highest predictive accuracy, integrates anatomy and technology | Requires µCT or quality CBCT and calculation |
Advantages of hFE analysis for implantation planning
- Objectivity and accuracy.
- Individualization of the treatment plan.
- Possibility of selecting the optimal implant before the procedure begins.
- Reduced risk of complications.
- Improved prediction of success with immediate loading.
Limitations of the study to consider
Despite the impressive results, the study has some limitations:
- Small sample size (22 samples, 2 donors).
- Use of only one type of implant.
- The modeling did not account for biological healing after insertion.
- Current need for µCT for model building, which limits direct clinical applicability.
However, the data shows a clear trend: hFE analysis may become the basis for new standards in implant planning.
The future of implant stability diagnostics
In the coming years you can expect:
- Integration of UFsim calculation into implantation planning software based on conventional CBCT.
- Development of predictive PS models for different implant systems.
- Improved accuracy of immediate loading protocols.
The goal is for the surgeon to know what to expect and how to achieve maximum stability before touching the bone with a drill.
Conclusion: What does this mean for your clinical practice?
The study opens a new era in digital implant planning: one where stability can not only be “felt” with your hands but also precisely predicted and calculated in advance.
And although the technology requires further adaptation for widespread clinical use, the direction of development is clear: more precise, safer, and personalized dentistry.
To stay ahead of the curve, it is worthwhile to introduce the following into your practice now:
- Active use of 3D diagnostics.
- Accurate planning.
- A commitment to objective assessment at all stages of treatment.
It is expected that with the development of software and lower requirements for the quality of initial images (using CBCT), the implementation of this technology will begin within the next 3–5 years.
Sources
Clinical Oral Implants Research Wiley – Primary Stability of Dental Implants in Human Jawbones: Experiments & FE Analyses – December 13, 2024