Torque or primary stability of the implant

Contents
So, the implant is placed in the bone. It is known that it takes a certain time (6 to 12 weeks) until complete osseointegration occurs and the bone adheres to the implant. Today let's look at how to achieve high implant survival especially in immediate restorative protocols. We will discuss what primary stability is and how much it depends on the patient's bone health.
What is the main condition for successful osseointegration
To heal the bone around the implant, as with any other bone injury, the bone fragments need to be placed in the correct position and fully immobilized. This is what casts are used for, and titanium structures are implanted for compound fractures.
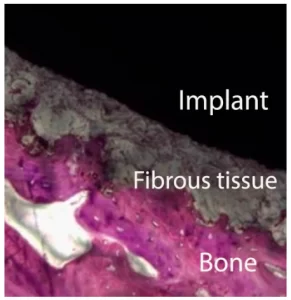
If this is not done, instead of bone fusion and the formation of a so-called bone callus, fibrous tissue forms between the bone fragments. Bone fragments heal, but do not adhere to each other, see the right image above. Because connective tissue grows very fast unlike bone.
Why implants don’t “take root”
When they say that the implant did not engraft, they often mean that a fibrous capsule has formed around the implant.
Such cases are not as rare as we would like. Integration is complicated by the fact that the titanium implant is still a foreign body, albeit with high biological compatibility.
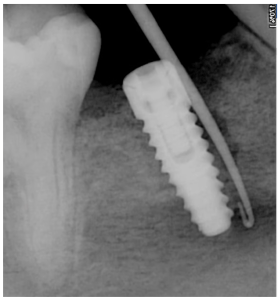
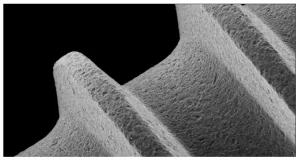
Yes, it is biologically inert and does not cause rejection or inflammatory processes, osteoblasts “cling” well to the rough surface. But at the border, the living bone/implant does not occur the same biological processes as when splicing the living bone. In a successful case, it is bone tissue that grows to an inert object, see the illustration below, where the implant and abutment with the crown are visible. That is, it is not the implant that takes root, but the bone.
Let’s see what actually happens when the osseointegration fails; the picture below shows the distribution of tissue in just such a case. You can see a layer of connective tissue between the implant and the bone. Instead of osseointegration, fibrointegration occurred.
When the implant is surrounded by soft tissue, it is an unfavorable surgical outcome. The correct terminology is to say that the bone has not engrafted to the implant, not the implant has not engrafted into the bone. There can be many reasons for failed integration, but next we will discuss the most important factor.
Lack of immobilization, i.e. implant mobility, most often leads to impaired osseointegration. This refers to primary stability, or rather the limit of micro-mobility of the implant, after which the risk of fibrous layer formation increases. There are many studies on this topic, but it took a long time to establish the number of microns by which the implant can deviate without causing problems. The most comprehensive and high quality studies on this topic have been done by the Schmuckler and Monkler group over the years, see examples of the best known papers.
Long-term studies have revealed that the very critical threshold of micromotion lies between 50 and 150 microns. If micromotion is above this level, then fibrous encapsulation predominates over osseointegration. That is, if the primary mobility is more than 150 microns, for example, 200-300 micrometers, then the risk of aborting the implant and fouling it with a fibrous membrane increases proportionally.
This is a good result of the study, but it is very difficult for practicing dentists to determine what micro-movement is in a newly placed implant. And this means that you need to focus on other indicators.
Why are the conditions for bone healing to an implant always different?
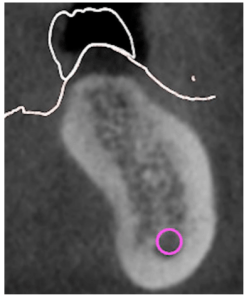
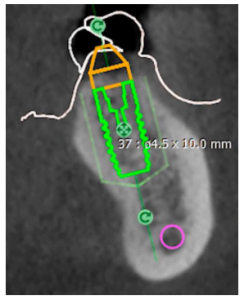
The fact is that the bone tissue itself is not homogeneous. In addition, the bone structure varies from patient to patient, with some jaws covered by a thick and very hard cortical plate, while the cortical part is thin and the entire bone is rather loose with a predominant spongy structure. Even in the same person, the bone structure of the upper and lower jaw can be different. The CT scan below shows that the bone structure is heterogeneous. The outer part is more dense, and the inner part is more loose. But even the structure of the inside is heterogeneous.
This means that if we perform all procedures according to the standard protocol, we will get completely different results in different bone densities. For this reason, a classification of bone types has been introduced, which we will discuss in detail next.
Classification of bone types
If you know in advance what type of bone you have to deal with, you can accurately predict the result. We will rely on the generally accepted 1985 Lekholm-Zarb classification. It’s convenient and clear. According to this classification, there are four types of bone. Of course, the boundaries between them are blurred, but it’s the best classification, which is used throughout the world. Bone density is well defined on a tomogram, and there is also a density scale. The units of measurement are named after its creator, the Hausfield units.
Let’s move on to the analysis of bone classes:
- D1 is a very dense bone tissue, most often found in the anterior region of the mandible. The illustration below indicates that the D1 bone density range is from 850 to 1200 units, but sometimes more. This type of bone gives good primary stability results and was previously considered ideal. But the bone of the first type is quite rare.
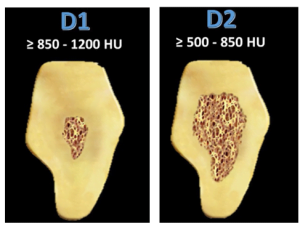
- D2 is also a dense bone with a value of 500-850 density units. The D2 bone is the most common in dental practice. Such a bone is found in the lateral sections of the lower jaw and upper jaw, as well as in the anterior section of the upper jaw. But in principle it can occur in any part of the jaw. If we return to our example from the picture, then this jaw can also be classified as type two, see the picture with the implantation plan applied.
- D3 is still quite dense bone with a well-defined hard cortical plate, but its thickness is much less. The main mass of the bone is made up of a rather soft spongy bone. The density of the third type of bone is in the range of 250-500 Hausfield units. An implant can still be inserted quite successfully in this type of bone, but care must be taken when selecting implants with small diameters.
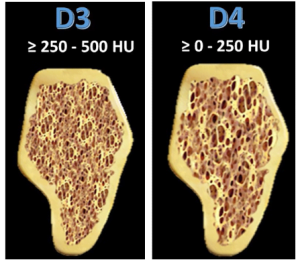
- D4 is the softest bone with a density of 250 units or less. Such bone is found on the tubercles of the maxilla. The compact plate is very thin and weakly expressed, by the strength in the most difficult cases it is close to cardboard. Sometimes it can be pierced with a probe during examination. It is very difficult to insert an implant into the bone of the fourth type.
Recall that the classification is very conditional, if we say that we are dealing with D2 bone, it does not mean that the thickness of the compact plate is necessarily 2 or 3 millimeters, and the cancellous part has a strictly defined structure. The living bone has an uneven and not always proportional distribution, which can be clearly seen in the illustration below.
The most important thing to remember is that bone is living tissue, with tremendous potential for regeneration. Going back to the mention that type I bone used to be considered the best option, but that is not quite true now.
Yes, it is easy to get good primary stability on D1 bone, but the process of osseointegration is also affected by the presence of an extensive circulatory system in the bone tissue (vascularization). The better the supply of oxygen and nutrients, the better and faster the process of osseointegration.
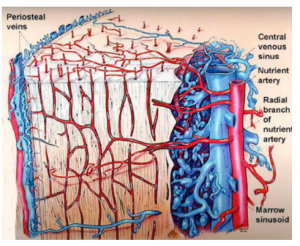
The fact is that there are fewer blood vessels in the bone of the first type, so you have to wait 12 weeks, not 6-8 weeks, for complete osseointegration. The bone of the second type has more blood vessels, more bone marrow spaces, and the bone transformation around the implant is faster.
What torque do we need for implant placement or what primary stability ensures success
We already know that the threshold level of implant micromotion is 150 microns, we also know that primary stability depends on the type of bone.
Further, we will analyze in more detail how to use the studied data on primary and secondary stability and the required torque in clinical practice.
How much torque is needed during implant placement for successful integration is an ambiguous question. If desired, you can find an approximately equal number of studies with completely different indicators. One part says that a very high torque is needed, d0 150 Ncm. For example, the following study states that torque up to 150 Ncm in dense cortical bone with unloaded healing does not cause bone necrosis or implant loss. And when implementing an immediate loading protocol, high torque increases primary and secondary stability.
While another group of studies argues that high torque is not necessary at all, and in some cases even harmful.
In this study there were 68 cases of implantation, with immediate prosthesis, the torque at insertion was 25 Ncm. Observations lasted an average of 5 years, the longest being 9.5 years. The survival rate was 95.5%, which is high.
Therefore, many specialists act on the basis of their own practice and successful clinical experience.
Let’s try to get to the bottom of this issue, because as often happens, the truth may be somewhere in the middle.
In order to reconcile both positions we will use the data of an excellent article from 2015.
They were able to obtain and systematize data that can be used in clinical practice. The goal of the study is to find a correlation between bone type, insertion torque and micromobility. The bone type can be determined from the CT scan, the torque is known at insertion. So with two values in hand, the third can be predicted. Namely, micromobility, which determines the probability of successful osseointegration.
This work was done on beef ribs and studied only mechanics, so it did not include questions of biological processes. But it nevertheless provides a better understanding of what a doctor needs to do to get a good prognosis for osseointegration.
In the study, implants with different torque were screwed into the beef ribs and abutments and crowns were placed in them. The crown was then loaded with a special dynamometer at a six degree angle with a force of 100 newtons. This roughly corresponds to the forces that occur in the mouth during chewing.
At the same time, the micromotion of implants installed with different torques was measured. As a result, figures were obtained that correlate with real clinical practice and are quite usable.
Let’s analyze the experiments in more detail. Beef ribs, which correspond to bone type D1, D2, were implanted with implants with a torque of 10 Ncm to 100 Ncm. Samples in which the required force indicators during installation were not achieved (less than 10 Ncm), or exceeded 100 Ncm, were rejected. Then the implant stability factor ISQ was measured. Why loaded the implant with the crown thus force of 100 newtons at an angle of 6°, which corresponds to the real load for the premolars. At the same time, micromotion was measured under a microscope. The division step of the microscope is 2 microns, which made it possible to make measurements very accurately.
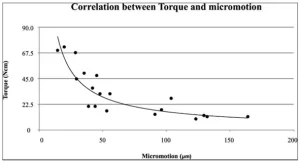
All implants were placed according to the manufacturer’s protocol. And that’s what we managed to find out, see the graph below.
There is an inverse relationship between torque value and micromobility under load. If we look at the curve, we will find that an increase in torque above 34 Ncm does not lead to a significant decrease in micromovement. The lower limit of good stability is set at 22.5 Ncm, if the primary torque is below 22.5 Ncm, this will significantly increase the stiffness.
Hence, the optimal torque value for implant placement is in the range of 23 to 35 Ncm. This data is supported by the ITI Treatment Guide, which states that the minimum torque value for the Implantation Protocol with immediate loading should not be less than 35 Ncm.
This conclusion is absolutely practical; the value of 11.57 Ncm is the threshold beyond which implant disintegration is almost guaranteed.
To summarize:
- A minimum torque threshold of 11.57 Ncm is obtained, at which micromobility is almost guaranteed to go beyond 150 microns. And fibrointegration instead of osseointegration will occur.
- If implants with torque greater than 35 Ncm are inserted, there will be no significant improvement in primary stability. Therefore, it does not make much sense.
- The resulting torque lower limit values are only valid for clinical cases of immediate restoration and loading. If the implant has a torque of less than 15 Ncm, it is better to cover it with a stopper and close it up tightly. If greater than 25, a gingival shaper may safely be placed without fear that tongue or food clod movements could somehow damage stability. There are clinical cases of extra-low torque. For example, when the bone is very soft, or when the hole for the implant is too wide.We hope this article helps you in your clinical practice, until further notice.