Risk Factors and Contraindications for Dental Implantation
In this article, we will talk about things that are unobvious when assessing the risks of and contraindications for implantation. In most cases, dental implantation and restoration are needed by people aged 50 and older, and most of them have health problems such as hypertension to diabetes. You need to carefully examine their lifestyle and the range of drugs that the patient takes on an ongoing basis. You should also consult with the attending physician, and not interfere with the course of treatment, or reduce the dosage or withdraw the medication. This should be only done by the attending physician, whom you should familiarize with the degree of surgical treatment by the dentist. Here, we create a road map to make it easier for dentists to understand what to do with patients in different conditions.
Why It Is So Important to Take a Patient’s History before the Surgery
Let’s start with the recommended literature, authored by Dr. Patton. This is a manual for assessing risks in patients’ conditions. We recommend that you have this book. Its format is not important. What is important, however, is that you always have it to hand.
We interview the patient when he or she first visits, but it is equally important to examine their medical records and to contact of their family or attending physician. After all, the patient is not a specialist and cannot always adequately assess his or her condition, and sometimes he or she cannot report any important peculiarities because of ignorance or for reason that they don’t consider them relevant.
Detailed information on the patient’s medical history is essential before you draw up a treatment plan and schedule any implantation surgery.
Particular attention should be paid to those aspects of health that may affect bone healing. After all, placing a root implant and then an abutment with a crown is a complicated process, and if the patient has a high risk of rejection, it can cause osteonecrosis and greater life-threatening problems for the patient.
Only a systematic approach and close cooperation with the specialists on related diseases will enable a determination of the risks of the planned dental implantation and the relative and absolute contraindications.
There are several important factors:
- Hemostasis. How normal it is, whether there are risks of incoagulable blood and bleeding after surgery. Or vice versa, whether there is a risk of blood clots and thrombotic embolism. How the hemostasis changes when a patient takes medication.
- How well the bone will heal in the patient’s current condition. After all, the healing process is influenced by both the general patient’s condition and the course of treatment, especially related to radiation therapy.
- Susceptibility to infection and the ability to resist it effectively.
- The patient’s susceptibility and resistance to stress. Of course, with modern anesthesia, pain can be completely eliminated. Notwithstanding this, the patient comes to the implantation in great anxiety, and the patient’s mental state influences their blood pressure, heart rate, and even subsequent healing.
How to Quickly Navigate the Patent’s Clinical Findings
Since most of our dental colleagues are not specialists in somatic diseases, it makes little sense to classify risks and contraindications according to their areas, such as cardiac problems or problems with the endocrine system (for example, diabetes).
Therefore, we will use a different classification based on the ASA system (physical status classification system), which is presented in the following table:
| Designation | Patient’s Status | Indications/Contraindications for Dental Implantation | Notes |
| ASA 1 | Healthy | Oral and maxillofacial surgery without additional precautions is not contraindicated | It is important to ascertain if there is an allergic response to substances that will be used in the surgery |
| ASA 2 | Mild systemic disease | Dental implantation surgeries are not contraindicated providing for thorough control (stopping) of the underlying condition, for example, diabetes, hypertension, asthma, epilepsy.
There may be relative contraindications for disease exacerbation |
Smoking 10 or more cigarettes per day bring a healthy person to ASA 2 class. It is also applicable to compensated first-degree hypertension, mild obesity, mild diabetes, epilepsy, pregnancy, etc. |
| ASA 3 | Severe systemic disease | Dental implantation is not contraindicated only after consultation with an attending physician and when the patient’s condition is sustainably compensated by drugs.
The diseases include controlled hypertension, insulin-dependent moderate diabetes, and mild chronic obstructive pulmonary disease. Also patients suffered from myocardial infarction, cerebrovascular disease, or congestive heart failure more than 6 months ago |
Ischemic heart disease, asthma, chronic bronchitis, alcoholism, drug addiction, severe hypertension |
| ASA 4 | Severe systemic disease posing a permanent threat to life | Very rare, but these patients can be candidates for elective oral surgery.
Implantation should necessarily be performed only in hospitals. This group may include patients with uncontrolled hypertension, diabetes, or epilepsy; moderate and severe chronic obstructive pulmonary disease; unstable angina, myocardial infarction less than 6 months old, and with cerebrovascular disorders or congestive heart failure |
Severe diseases of the heart and pulmonary system, a recent (up to 6 months ago) heart attack or stroke, as well as severe kidney diseases requiring hemodialysis |
| ASA 5 | A patient will not survive without urgent surgery | Dental implantation is unacceptable | There are no cases where dental implantation is necessary before life-saving surgery |
| ASA 6 | Brain death | Dental implantation is unacceptable | The patient is actually dead |
Absolute and Relative Contraindications for Implantation
Let’s consider in more detail the risk factors that influence normal bone healing after the dental implant is placed:
- High dose of radiation to the head and neck. Such procedures are used in the treatment of cancer. Surgery during implantation can cause osteoradionecrosis. Prior to drawing up a treatment plan, you should:
– consult the attending oncologist and the local maxillofacial department;
– obtain a complete picture of radiation therapy. The risk of complications increases significantly when the cumulative radiation dose exceeds 45 Gy and a full course of oral cancer therapy usually involves from 33 to 34 doses of 2 Gy each. This results in a cumulative dose of 66 to 68 Gy, but there are exceptions.
The good news is that after a while, especially under stable remission, the risk of complications from dental implantation is reduced. Therefore, radiation therapy can be considered a relative contraindication to surgery in the oral and maxillofacial area. - Osteoporosis itself slightly increases the risk of complications. Previously, osteoporosis was an absolute contraindication, but the available statistics disproved the idea. The real reason for the increase in the risk of complications in dental implantation is antiresorptive drugs (biophosphonates). Osteoporosis is also a relative contraindication to dental implantation. It requires a consultation with the attending physician. He or she may decide to reduce the dose or suspend the medication, but the timing is equally important. The point is that drugs tend to accumulate in the bones and have a very long gestation period.
- Types of diabetes that are difficult to manage glycemic control. When blood glucose levels spike, bone healing is very slow, and there is a serious risk of post-surgical infections. These patients are poor candidates for dental implantation, and it is very difficult to form and heal the margin around the healing cap properly. If specialists can choose a course of treatment and stabilize the patient’s condition for at least several months, this reduces the risk of complications. So this case is also included in relative contraindications for dental implantation.
- Immunosuppressive therapy is used in the transplant of organs, severe rheumatism, some types of autoimmune diseases, and some other conditions. Immunosuppression also increases the risk of post-surgical infections. But this depends on dosage and course of administration. With low doses, the risk of complications is also low. However, the risk rate should only be assessed by the attending physician.
- Diseases that may influence treatment compliance and oral hygiene. These are disorders of the nervous system, from schizophrenia to Downs Syndrome. These conditions are not always contraindications. There are enough statistics of successful dental implantation for people in these categories. Here, more than anywhere else, you should consider each individual case separately. Many patients are not able to care for their own oral cavities, but such patients can be considered candidates for dental implantation if there is someone to help with the care of their implants.
- A list of medications taken. It is an unobvious risk factor that can be a contraindication or a change in treatment guidelines.
It is important to know how medicines taken on an ongoing basis can influence:
- local and general bone healing;
- the complexity of dental implantation surgery; and
- their interaction with pre- and post-surgical drugs.
We have already mentioned some drugs at risk; now let’s take a closer look at them:
- Antiresorptive drugs in high doses, primarily biophosphonates. They are used against osteoporosis, metastases, myelomatosis, etc. Patients on such therapy have an increased risk of losing implants and developing osteonecrosis. The most difficult thing is that drugs in this group accumulate in bones with a long half-life (more than 10 years). Therefore, high doses and long-term administration is an absolute contraindication for oral and maxillofacial surgery.
- Immunosuppressive drugs are used against cancers and in chemotherapy, in transplantation of organs. Including corticosteroids in high doses. If such drugs are taken, the risk of post-surgical infections and loss of implants is increased. High doses are an absolute contraindication for dental implantation. The good news is that when patients complete treatment and recover their immune function, they leave the high-risk group.
- Antithrombotic therapy. It is often administered to people with cardiovascular disease. However, surgery increases the risk of post-surgical bleeding. To remove a patient from the risk group, you can adjust the therapy and lower the dose or stop the medication. You should not, however, withdraw the prescription of drugs on your own. In fact, it is much easier to cope with bleeding in the mouth than with thromboembolism (vascular blockages) that can develop when antithrombotic therapy is withdrawn. Many of these drugs are also incompatible with antibiotics and non-steroid anti-inflammatory drugs. This, too, needs to be clarified and discussed with the specialist to amend the treatment plan.
Risk Factors Determining the Condition Caused by the Patient’s Lifestyle and Behavior
- Smoking tobacco (more than 10 cigarettes a day). This increases the risk of peri-implant pathology and implant loss. The risk increases, but not critically Smoking is not a contraindication.
- Alcoholism is not only a systemic malfunction of all organs and systems but also a cause of non-compliance with treatment, poor oral hygiene, poor nutrition, etc. Here, a patient is close to an absolute contraindication for dental implantation, since complications after surgery and delayed medical treatment may endanger the patient’s life.
- Drug addiction is similar in risk to alcoholism, but has even more complex consequences and is an absolute contraindication for dental implantation.
- Patient’s refusal to follow a doctor’s advice on oral cavity care. In severe cases, when you can neither teach nor persuade a patient, it is an absolute contraindication for dental implantation. However this situation can be changed. After a while, the patient can change his or her behavior independently or under the influence of psychotherapy or a hygienist.
Allergic Responses to Dental Implantation and What Titanium Allergy Is
Allergies can influence the success of the surgery. In this article, we want to broach the subject of titanium allergy and take this issue off the table. This is a question most often asked by patients. Fortunately, they ask it less frequently now. In fact, the likelihood of titanium allergy is negligible. Of course, there are documented cases, but these are one-off cases that you can count on one hand. This is so rare that the likelihood can be compared to the development of an air allergy (several cases have been documented).
The most commonly defined allergic response to titanium is poorly diagnosed complications of other origins (peri-implant pathology, mucositis, etc.).
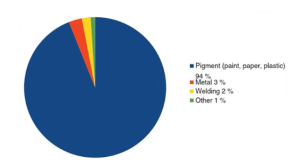
Indirect evidence of rare and unlikely titanium allergy is shown on the diagram below.
It makes it clear that the use of titanium (most often in the form of titanium oxide) is common, and we come into contact with titanium-containing substances every day. From colorants to suntan creams, you can find titanium everywhere. So with all due respect, we can say that titanium allergy is most often a misdiagnosis.
However, when taking the initial history, it is critical to conduct a real analysis and identify allergens for a specific patient, antibiotics, painkillers, etc.
We hope that you will find it easier to identify the risks and build a more effective treatment plan for dental restoration.