In the first two parts of this article (Part 1 | Part 2), we established several important points about the soft tissue healing process and the causes of bone resorption, without which understanding of this part of the article would be incomplete. Therefore, we recommend that you read the previous parts, of course we will briefly remind you on what principles this or that conclusion is based, but the understanding may be incomplete.
What factors affect bone remodeling around the implant neck?
Let’s start with the following illustration, which shows the two implant placement options in comparison with a healthy tooth.
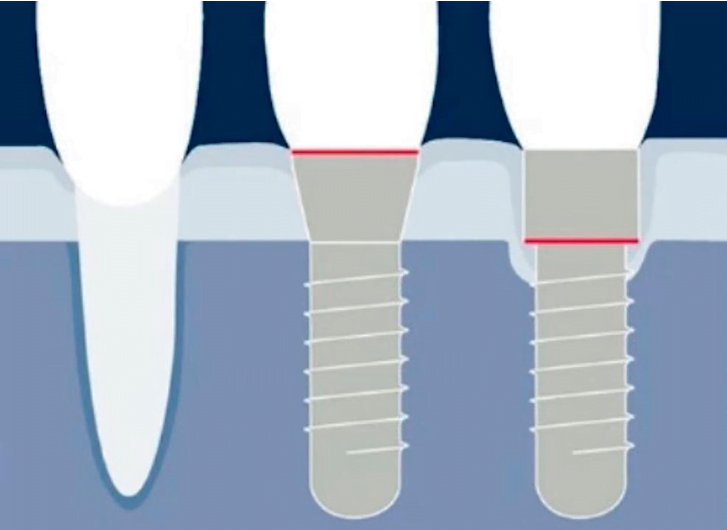
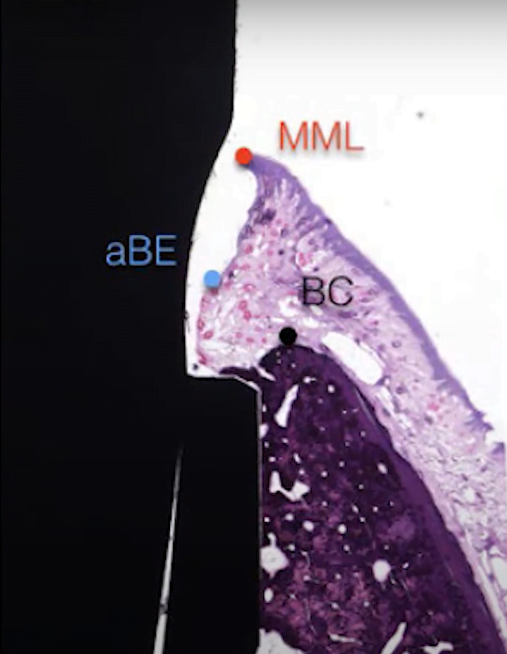
Implants differ in the depth of insertion into the bone and the location of the implant/abutment connection. In the first case, the implant is seated so that the implant/abutment boundary is at the level of the soft tissue. The second option is complete immersion of the implant into the bone. As practice shows, the formation of the gingival cuff in the first case is more similar to that of a healthy tooth whereas in the case of total immersion, there is a loss of bone tissue around the implant. We discussed this process in detail in a previous article. The body sort of makes room for full soft tissue integration because it is critical that the connective tissue attaches and forms an impermeable barrier below the connection line between the abutment and the implant.
Also, we already know that the parameters of the soft tissue connection in the tooth and denture, with all the external similarity, are markedly different in both structure and size. If the total depth of the gingival cuff for a living tooth is an appreciable 2.7-2.8 mm, for an implant it is 3.0-3.5 mm. The fact is that the epithelial part of the gingival cuff around a titanium implant is always larger. The structure of the junction at the level of the collagen fibers is also different. Around the living tooth there is a developed network of both longitudinal and perpendicular fibers, which securely hold the gum around the root of the tooth. In the case of an implant, only longitudinal types of collagen fibers are formed and the strength of the connection is noticeably lower. This is not so critical if the patient has a thick biotype with a massive keratinized gingiva, but if the original keratinized gingiva layer was thin, there can be problems with soft tissue integration.
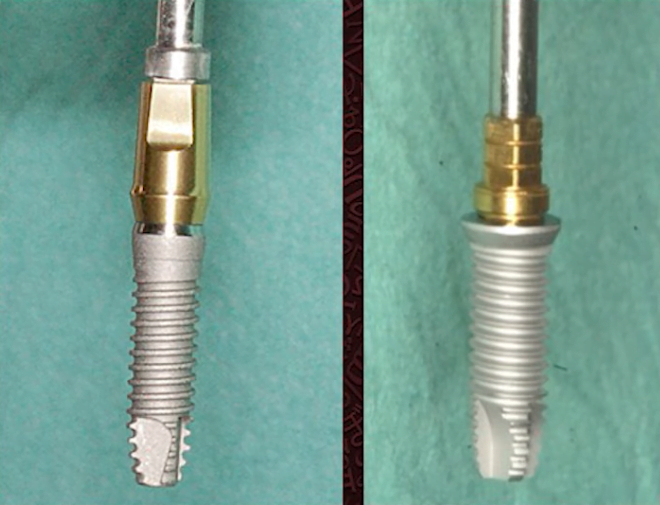
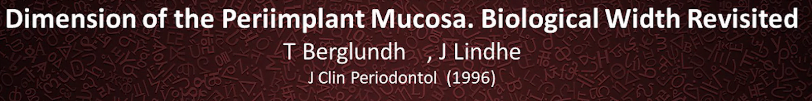
The fact that the implant/abutment interface is a critical point of reference has long been known. In addition to the technique of placing the implant at the gingival level, platform switching technology has emerged. Its essence is to increase the area for gingival cuff formation by a step between the implant edge and the base of the abutment. It is about the popular conical interface of the abutment-implant connection. What the platform switching looks like can be clearly seen in the illustration below.
Because the base of the abutment is narrower than the top of the implant, a step is created, which increases the contact area with the soft tissues. As a consequence, there will be less bone loss around the implant. However, the positive effect is less frequent than desired. Let’s look further into the reasons.
Why does platform switching sometimes not work at all?
From previous articles in this series we know that:
- The size of the switching shoulder of the platforms is important. The more significant it is, the better, because a connective tissue attachment needs about 1-1.1 mm, and an epithelial one needs almost two to 1.88 mm.
- Proper surface treatment is important. The connective-tissue portion of the cuff makes better contact with a rough surface, whereas a smooth surface is better for the epithelial portion.
For a long time, there were not enough quality meta-analyses to prove the efficacy of platform switching. Efficacy refers to the reduction of bone loss around the implant vertically. Moreover, there have been many articles stating that platform switching does not work.
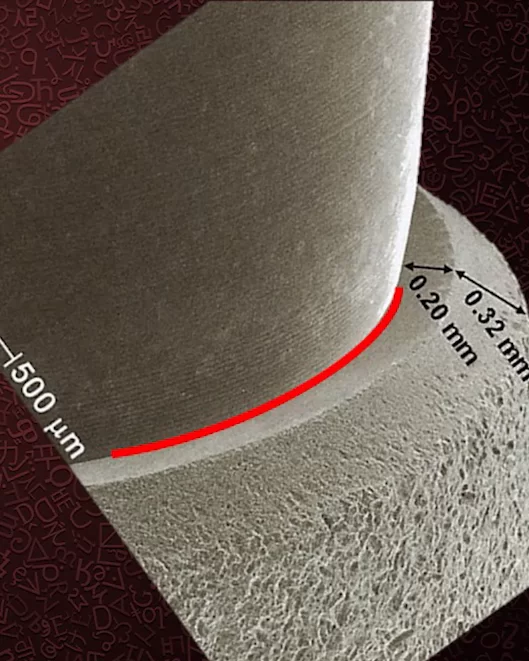
Let’s start with a rather old study from 1996, which is included in many textbooks as a reference.
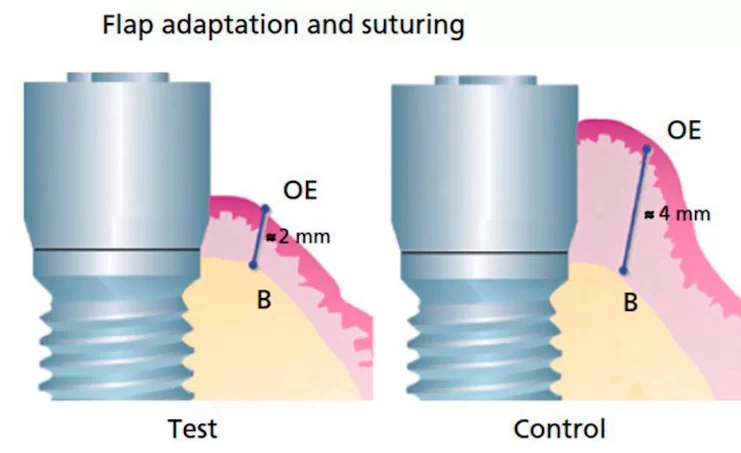
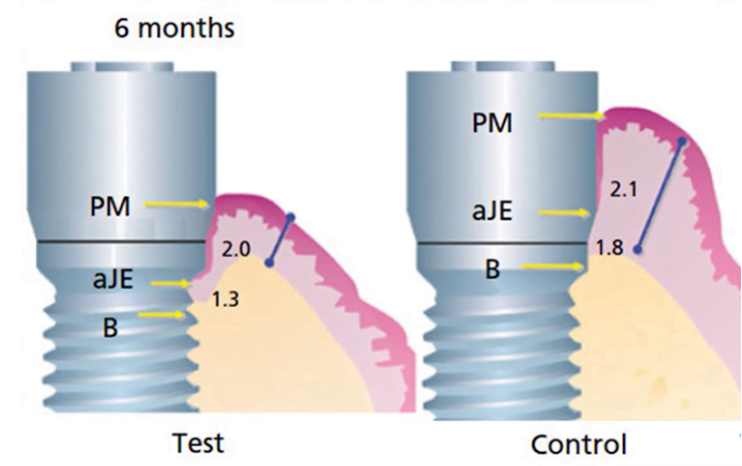
The study is based on a simple and illustrative animal experiment. The ridge was dissected and implants were placed. The study was performed on milled (smooth) Branemark implants. The thickness of the soft tissue flap over the bone was 4 mm. The flap remained the same in the control group. Whereas in the test group the flap thickness was artificially reduced to 2 mm, see illustration below.
After the implants were placed, the gingiva was sutured and the healing process proceeded without complications. However, when we compared the situation in the test and control groups six months later, we found that bone ridge remodeling occurred in the group where the thickness of the flap was artificially reduced. Around the implant there was a gap of almost 1.5 mm vertically whereas in the control group there was practically no bone loss, see the illustration below.
As we already know, the height of the gingival cuff around the implant is about 3.5 mm. So it turns out that if initially the soft tissue thickness was reduced to 2 mm, the body dissolved some bone tissue to make room for a full-fledged gingival cuff. If the soft tissue thickness is initially greater than 3.5 mm, there is almost no bone resorption.
Unfortunately, this classic study was forgotten and most of the first decade of this century was spent in heated debates about what actually causes bone loss in the first year after implantation. This is really the most important period afterwards when the bone and soft tissue remodeling process stabilizes and the bone loss slows down to a complete stop.
There were theories that excessive mechanical stress was the cause of bone loss. In contrast, it was argued that bacterial pump and the shape of the implant/abutment interface needed to be changed. This is the theory followed by the proponents of tapered connections. Indeed, in such connections, the abutment sits much tighter in the implant and there are fewer micro gaps through which bacterial fluids can penetrate.
Cone connection does have some advantages, but not as dramatic as their supporters and manufacturers claim.
Let’s go back to what has been established with absolute certainty to date. The height of the gingiva over the bone is a determining factor in remodeling. If it is sufficient, the bone is preserved in any type of connection. Conversely, if we see that the flap thickness is less than 3 mm, bone resorption around the implant is inevitable, even in the case of a tapered connection with platform switching.
In the late noughties of the 21st Century many specialists returned to the above-mentioned classic study and conducted a number of interesting studies on the same topic.
Experts decided to find out why there is so much conflicting data. In some studies, platform switching works and in some it doesn’t. The same is true for the different depths at which the implants are placed.
One of the key questions was what happens to resorption if you use the same implants but with different gum thicknesses? We are talking about the initial thickness of the soft tissue at the time of surgery. A pattern was found. The thicker the soft tissue layer and the thicker the keratinized gum layer, the less bone resorption around the implant. This agrees completely with the classic study from 1996. Let’s break this down in more detail.
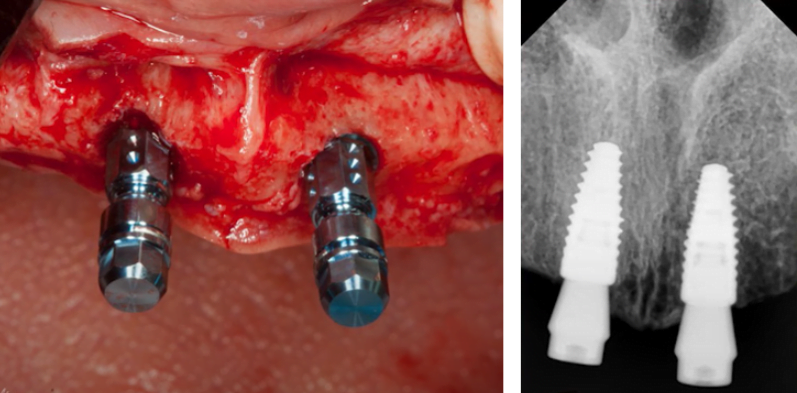
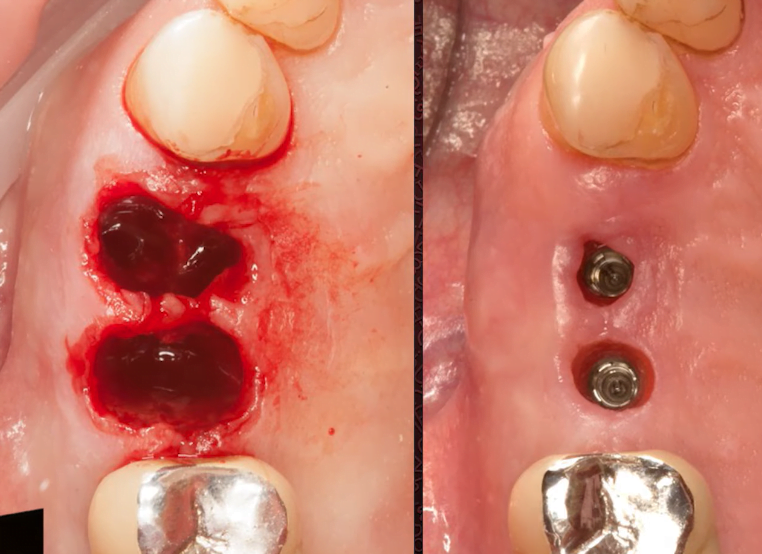
Look at the pictures below, here initially there was a fairly thick gum of at least 2.5 mm, two implants were placed nearby with slightly different seating depths, but with the same planar connection. A paired restoration was performed on them.
The second important goal of this series of studies was to establish how effective the concept of platform switching is at different initial gingival thicknesses. Here, too, there are some very interesting results.
For this purpose, an in vivo experiment was conducted on humans. Patients were placed next to two different implants, one with a planar connection and the other with platform switching.
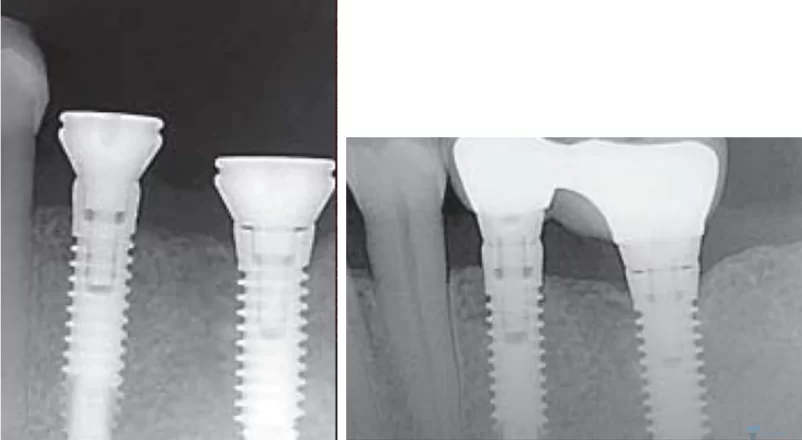
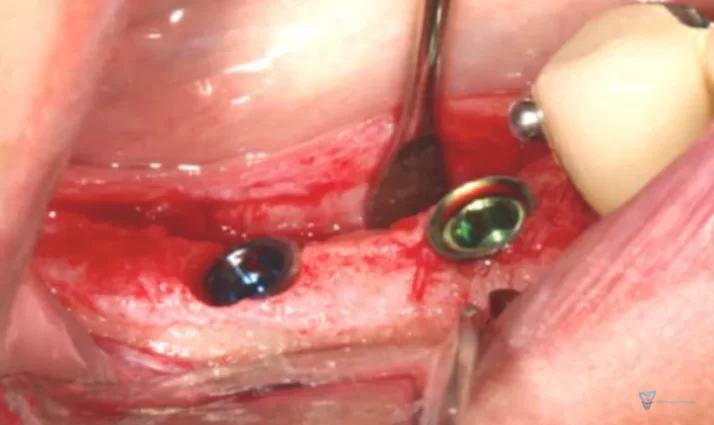
During the surgery, the height of the gum was measured before the implants were placed, as shown in the pictures below.
You can clearly see that in the first case (left photo) the gingival height is very small, only 1.5 mm. In the second photo the soft tissue thickness is more than 4 mm. The implants were placed in approximately the same positions.
The picture below shows the result of implant placement with a thin soft tissue flap. You can clearly see that one implant with platform switching and the other without and they are set in the same way. Specifically, the implant/abutment interface is at bone level.
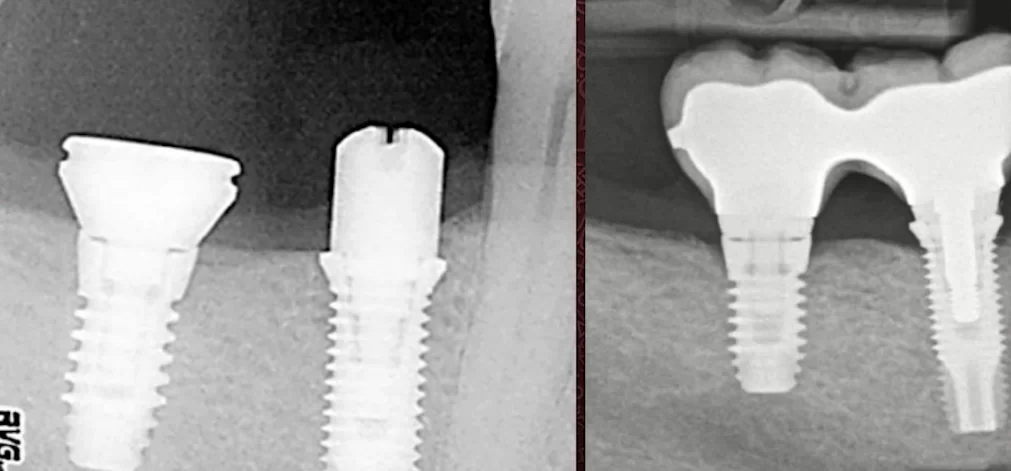
One year later, the radiographs were repeated and showed that there was significant bone remodeling in both cases. For clarity, we placed the images side by side so that we could assess the condition of the bone at the time of implant placement and 12 months later.
The conclusions are unambiguous. The concept of platform switching does not work if the initial gingival height is ≤2mm. However, that does not mean that the platform switching concept does not work at all.
What is the Zero Bone Loss concept?
This concept emerged from the aforementioned series of studies and boils down to recommendations on how to reduce bone loss to zero. There is also good news that the authors of the study have systematized their research as well as analyzed a large number of other studies and have published a book with the same title, see the book cover in the following illustration.
This book is full of practical advice and will be useful to both young and experienced professionals. Professionals will find confirmation of their own observations and new ideas to put into practice.
The concept of zero bone loss is simple. To reduce or eliminate bone loss around the implant neck, the thickness of the soft tissue above the bone needs to be as large as possible. It is good if the patient initially has a thick layer of gum over the bone, worse if the height of the gum is less than 2 mm. The good news, however, is that the condition of the gums can also be influenced. We’ll deal with that in a future post.
Before we continue, let’s summarize.
So, what determines the bone remodeling around the implant neck? As an example let’s take the tissue level implant, which is positioned as one of the solutions to bone loss problems.
- The distance from the bone edge to the inner border of the implant platform. This is a universal rule and applies to all implant types. The higher the implant/abutment connection is above the level of the bone ridge, the less bone is lost. If you place the tissue level implant at the level of the bone, the resorption will be greater, and vice versa, if you place the bone level implant so that the implant/abutment connection is above the bone ridge and closer to the gingival border, the bone remodeling will be less. We have discussed this principle in detail in previous publications.
- Gingival thickness: the greater the thickness of soft tissue above the implant, the less bone loss. After all, it takes 3.0-3.5 mm to form a complete gingival cuff and if the soft tissue thickness is insufficient, the body compensates by dissolving some bone tissue. We have already discussed this relationship in this article; see the image below for an illustration. The difference between the radiographs is about 12 months.
In the image we see a stable picture, but nevertheless bone remodeling did occur. Now we understand why it happened. It is not enough to bring the implant/abutment connection outside of the bone ridge; the soft tissue must be thick enough. This patient really had an original gingival thickness of less than 3 mm; and exactly 3 mm is the minimum necessary so that the body does not have to dissolve some of the bone to form the gingival cuff.
How do biotype, phenotype, attached gingiva, and gingival thickness relate?
Now let’s look at what determines marginal bone remodeling around the neck of a submerged (bone level) implant. Let’s look at one interesting clinical case. In a previous article we discussed the importance of keratinized gingiva for quality connective tissue attachment. We know that the quality of connective tissue around an implant is significantly inferior to that of a living tooth, and that the thickness and massiveness of the original attached keratinized gingiva is a determinant of successful soft tissue integration in the long-term.
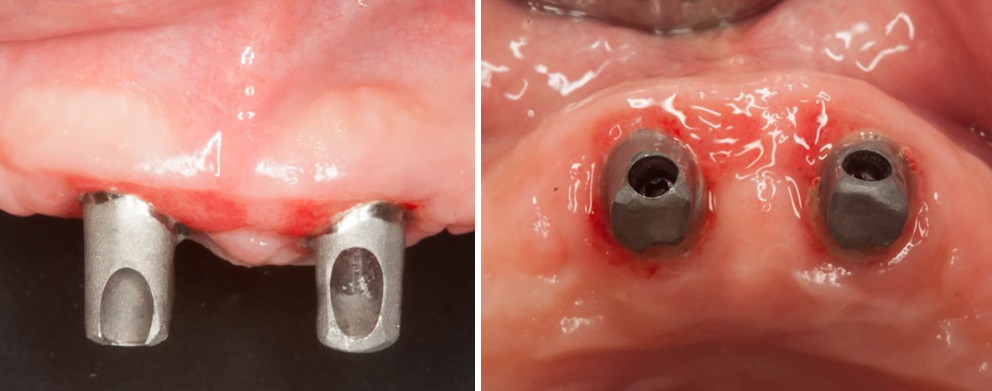
If you look at the image below, you can see that this patient retained a significant amount of attached keratinized gingiva. At first glance, these appear to be ideal conditions for excellent implant results in the long-term.
However, at the intraoperative stage we can see that the palatal section of the flap is quite thin, only about 2, maybe even less than 2 millimeters. At the same time, the radiograph shows that the implants are placed at the level of the bone ridge, and one is even lower (subcrestally).
That is, initially we saw a fairly wide ridge with a significant amount of attached gingiva especially on the vestibular side, but the thickness of soft tissue above the bone ridge appeared to be insignificant.
It is important to recall the biotypes of the gingiva. We have parsed that this is something predetermined at the genetic level and there is even a correlation with the appearance of the person. For example, astenics (people of thin build) usually have thin bones; the shape of teeth is triangular oblong with a small amount of attached keratinized gum of the pistons type. Conversely, people of dense build, broad and chunky, and the shape of the teeth are close to square. The keratinized gum has a straighter shape and the amount of attached gum is much larger.
Reality, however, tells us that there are no hard rules and each case should be considered individually. This is confirmed by our example, because according to all external signs the patient belongs to a massive biotype. Indeed, we can see a sufficiently wide and massive alveolar ridge, a significant amount of attached keratinized gingiva on both sides of the alveolar ridge, but the thickness of soft tissue over the bone plate is small. Generally speaking, we encourage you not to get attached to a biological phenotype because there are techniques that allow you to change the amount and structure of soft tissue, which we will talk about later. Now let’s return to our clinical case.
The following images show the fitting stage of the abutments and again we can clearly see that the width of the bone ridge has a good margin, we can see the massive keratinized gingiva on both sides. All this gives hope for a favorable prognosis in the long term.
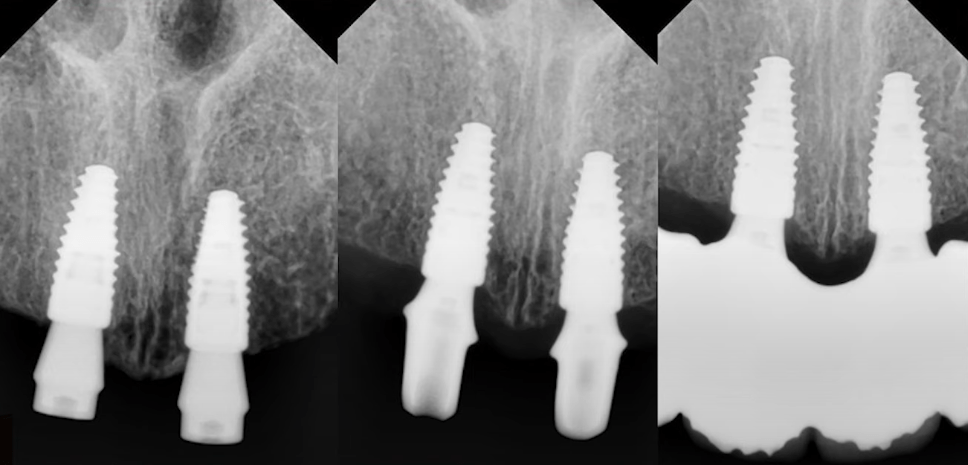
However, if we look at a series of radiographs taken at different times from the time the implants were placed until one year after surgery, we can see that bone remodeling did occur.
To summarize this case, we have the following picture:
- Implants with switching platforms with a shoulder size of about – 0.5 mm were used.
- The diameter of the implants is quite large, 4.1 mm.
- Bone remodeling with partial resorption did occur. The reason is the initial insufficient thickness of the soft tissue above the bone ridge.
- The long-term prognosis for implant survival remains favorable because the bone loss is moderate, and the massive bone and significant amount of attached keratinized gingiva help stabilize the implant.
It is important to understand that bone remodeling processes associated with a lack of soft tissue thickness occurs in the first 8-12 months. Thereafter, the structure and ratio of bone and connective tissue remains practically stable. Our clinical case confirms this dependence because neither the degree of keratinization, nor gingival attachment, much less platform switching implants can affect the degree of resorption if the initial soft tissue thickness over the bone plate is insufficient.
To summarize, let us list the factors that affect marginal bone resorption around the neck of bone level implants.
- Distance from the bone ridge to the border of the implant/abutment connection. Exactly the same as for tissue level/non-implants;
- Gingival trauma associated with suprastructure replacement. Any fitting of an abutment, removal of gum shapers for placement of transfers, etc. – worsens the situation and forces the body to form a connective tissue attachment below the level of injury. Tissue level implants have no such traumatic effect; and
- The thickness of the gingiva above the alveolar ridge level at the implant site.
Significance of all the above parameters at different stages of treatment
Let’s summarize and list the factors that influence bone loss around the implant neck in order of importance.
- The position of the implant/abutment interface relative to the bone plate. The higher the attachment interface, the less bone loss around the implant neck See the illustration below
.
It’s all about the formation of the gingival cuff, which consists of two types of attachments:– At the level of the epithelium; and
– At the level of connective tissue (collagen fibers).As we already know, the connective-tissue attachment is always formed apically above the implant/abutment interface. It is this connection that causes bone remodeling if the implant/abutment connection line is too close to the bone plate boundary. This is why a supracrestal implant fit causes the least resorption. The formation of the gingival cuff is also influenced by:– Implant surface type – microporous and roughened surfaces work better; and
– Platform switching – allows for less bone remodeling under certain conditions. This is due to the additional space for soft tissue attachment. This space provides the stepping stone between the implant and the base of the abutment. - The thickness of the gingiva above the alveolar ridge bone plate. If it is less than 2 mm, 1.1-1.6 mm bone loss around the implant neck is inevitable. However, other favorable factors may enable the implant to remain stable and further remodeling to stop.
- Volume and quality of the attached keratinized gingiva. This factor has the greatest impact on the long-term outcome. If the patient has sufficient soft tissue volume with good keratinization, then after minor remodeling in the first 8-12 months, the condition will stabilize. Such a restoration lasts for decades without any problems or complaints.
.
 .
.
Well-keratinized gingiva attached to the bone stabilizes the gingival cuff around the implant. Even if a significant amount of bone is resorbed (1.5 mm or more), a strong and stable gingival cuff will prevent problems such as gingival recession and exposure of the titanium portion of the prosthesis. If it is insufficient, chewing and tongue movements will result in soft tissue migration around the implant. This can lead to trauma and chronic inflammation, gingival recession, loosening, and even loss of the implant.
In fact, bone remodeling around implants is not a verdict and with good hygiene and soft tissue conditions, the prognosis for implant survival will be favorable.
We hope this article was helpful. In the next articles we will discuss the bacterial pump theory and the tapered connection between the implant and the abutment.