A New Method for Soft Tissue Restoration in the Aesthetic Zone: Dermal Apron Technique with a Clinical Case Example
Installing an implant and a prosthesis simultaneously has always been a challenging task. These operations are most often performed in the area of the front teeth, where the main issues are the lack of bone and gum tissue in the implant and crown installation area. Even if the gums cover the crown at the time of installation, this coverage will not last long. During the healing process, the loss of both bone and soft tissue is inevitable. Therefore, in such operations, surgeons add a bone graft and a soft tissue transplant. The bone material can be either the patient’s own or an external material made from processed animal bone, most often bovine (xenograft) or human donor bone (allograft). In this article, we will briefly review a study published in ScienceDirect, which discusses one of the methods of soft tissue augmentation—the dermal apron technique, which is already demonstrating positive results in both clinical and aesthetic indicators.
Key Features of the Method
The dermal apron technique uses a combination of allograft bone and soft tissue to increase the thickness of the soft tissue around the implants. This approach reduces the need for more traumatic autogenous grafts, such as palatal harvesting, thereby reducing complications and increasing patient comfort.
The Main Advantages of the Method:
- Preservation of tissue volume: The use of a dual-zone graft increases soft tissue thickness.
- Reduced risk of complications: The absence of the need to collect autogenous tissue reduces the risk of postoperative complications.
- Improved aesthetic results: Thicker soft tissues better mask the contours of the implants, which is important for the front teeth.
Results of the clinical study
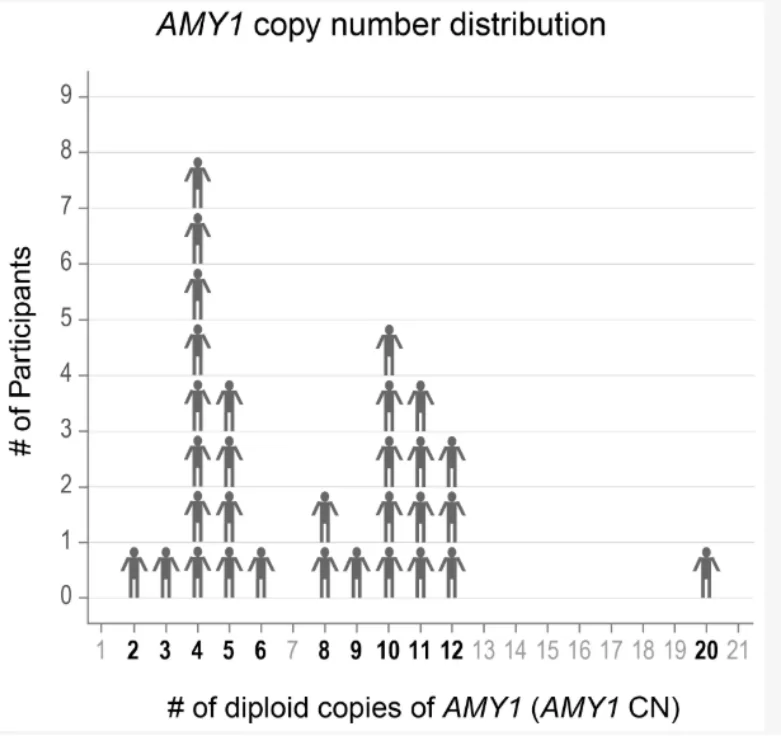
The study analyzed 30 cases: 15 patients who underwent the standard procedure without augmentation and 15 patients who underwent the dermal apron technique. The results show a significant increase in soft tissue thickness in the augmentation group.
| Indicator | Standard Procedure | Dermal Apron Technique |
| Thickness of soft tissue, mm | 2.10 | 2.85 |
| Healing time, weeks | 12 | 8 |
| Patient satisfaction level | 80% | 95% |
Description of the Technique
The procedure begins with the flapless extraction of the damaged tooth. Special instruments are used to preserve the alveolar bone. After the implant is installed, a bone graft is inserted into the hard tissue area, and a dermal allograft is inserted into the soft tissue area. A temporary crown with screw fixation is then installed.
The peculiarity of the method lies in the unique approach to the formation of soft tissues: the allograft is sutured under the mucous membrane, creating additional volume. This provides a more natural appearance and resistance to gum recession.
Case Study
A 44-year-old female patient presented with significant root resorption of an anterior tooth. A decision was made to use the dermal apron technique. Successful healing occurred within 12 weeks, and the soft tissue thickness increased from 2.0 mm to 3.7 mm, as confirmed by clinical and radiographic examinations. The pictures below show the initial presentation.

External appearance of the maxillary right central incisor with internal root resorption. Picture from a scientific journal: ScienceDirect
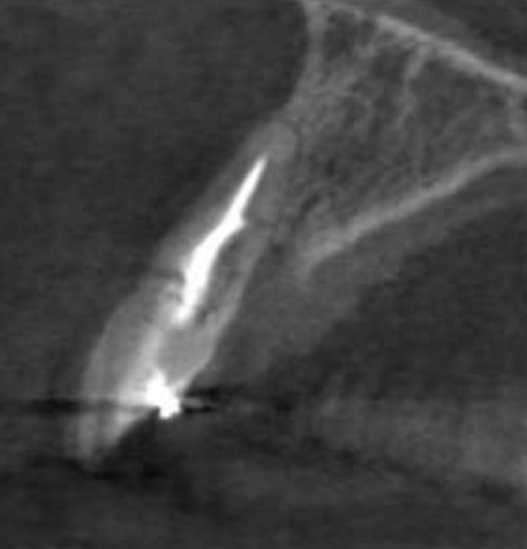
Cross-sectional view of the same tooth, demonstrating severe internal root resorption. Picture from a scientific journal: ScienceDirect
It was decided to extract the tooth and install the implant and crown simultaneously. The tooth was extracted atraumatically without cutting the soft tissues (flapless method), which preserved the thin outer bone plate. A 4.5 x 15 mm implant was installed in the socket with a 12° angle correction under the ridge. The picture below illustrates this implant installation technique.
Immediate (right after extraction) implant placement – the implant is shifted to the palatal aspect of the extraction socket. Picture from a scientific journal: ScienceDirect
The torque during installation, which ensures primary stability, was 75 N*cm. Next, a bone graft was placed at the gingival margin level to fill the space between the implant and the outer bone plate. The bone graft used was a mixture of cortical/cancellous FDBA and xenograft in a ratio of 4:1, as shown in the image below.

Bone graft placed in the socket – an abutment is installed in the implant on which the crown will be made. Picture from a scientific journal: ScienceDirect
A temporary screw-retained crown was then fabricated. Simultaneously with the crown placement, an allograft was placed around the crown support. The soft tissue graft was inserted into the subperiosteal space approximately 3-4 mm apical to the level of the facial crest bone. The abutment screw was tightened to 35 N*cm. The bite check showed that the temporary crown was out of occlusion and did not contact the anterior part of the lower jaw. The result of this stage is shown in the following picture.

Screw-retained provisional crown, out of occlusal contact is delivered and the dermal allograft successfully inserted, the upper edge of the dermal implant fixed with a suture. Picture from a scientific journal: ScienceDirect
After the operation, an X-ray was taken, which confirmed the successful placement of the temporary restoration.
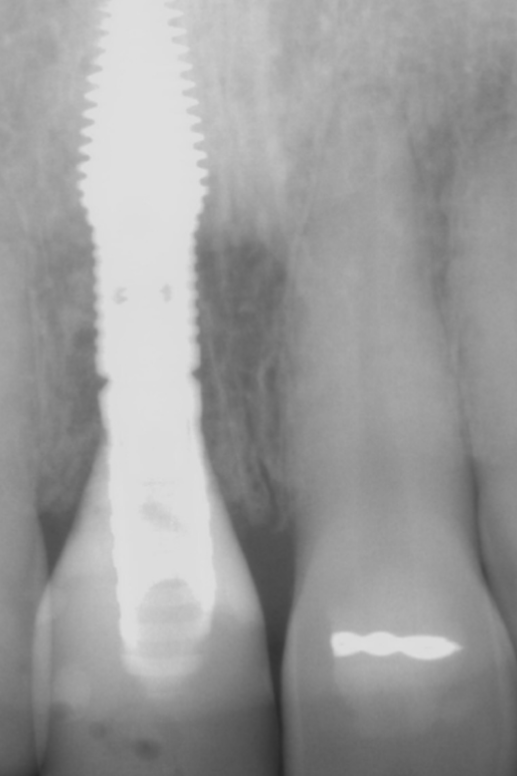
Post-operative radiograph confirming complete seating of the provisional restoration and the dual-zone bone graft is visible mesially and distally. Picture from a scientific journal: ScienceDirect
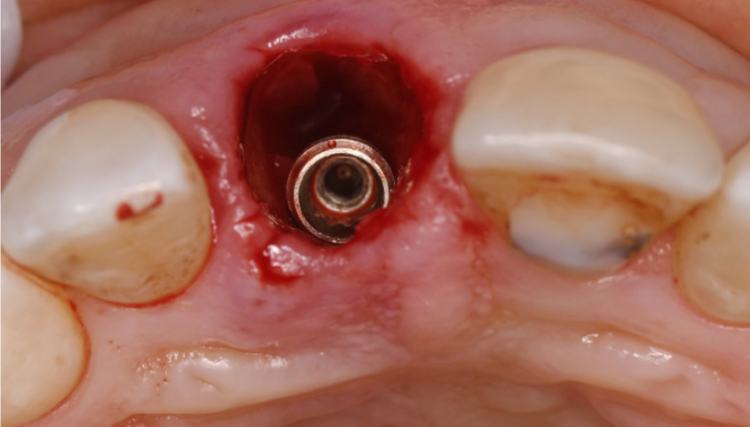
During the period of complete osseointegration and until the permanent crown was installed, the patient was instructed not to put any load on the anterior incisors for at least 10 weeks. After 12 weeks, the temporary crown was removed, and the implant stability was checked with an Osstell Beacon (Osstell), showing an ISQ of 68 in the facial and palatal directions. The soft tissues around the implant were well-formed, had sufficient thickness, and exhibited a scalloped morphology, as shown in the image below.
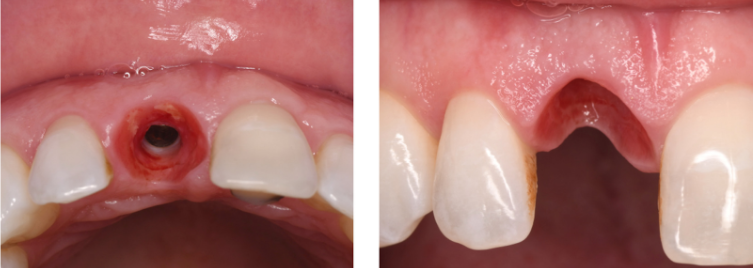
Healthy thick mucosa – the original scallop of the gingiva is preserved via immediate provisionalization. Picture from a scientific journal: ScienceDirect
For the permanent prosthesis, a custom abutment was made using CAD/CAM technology. A PFM crown was installed on the abutment outside the patient’s oral cavity using cement retention. Then, the abutment with the crown was installed in the implant and retained with a screw tightened to 35 N*cm. The restoration was completely successful in terms of aesthetics and functionality.
The final radiograph confirms the successful installation of the crown and the proper positioning of the implant in the bone tissue.

Radiograph at time of crown-delivery. The narrow coronal portion of the implant increases space between the implant and adjacent teeth. Picture from a scientific journal: ScienceDirect
Benefits for Professionals
The dermal apron technique offers several advantages for dentists:
- Predictability of results: The use of standardized materials and methods allows for achieving stable results.
- Reduced trauma: The absence of the need to collect palatal tissue reduces the level of complications and pain associated with the procedure.
- Improved aesthetics: Increasing soft tissue volume enhances the appearance of implants.
Conclusion
The dermal apron technique is a promising method in dentistry that can replace traditional, more traumatic approaches. The use of allografts ensures not only the preservation of tissue volume but also the improvement of aesthetic outcomes. Specialists who seek to improve the quality of treatment and patient comfort may consider implementing this technique into their practice. The full version of the study can be found at the link in the source.
Source
ScienceDirect – Update on the efficacy of the dermal apron technique: Increasing peri-implant mucosal thickness and tissue stability – September 2024