Guided Bone Regeneration (GBR) Part 3 Allogenic and xenogeneic and alloplastic transplants

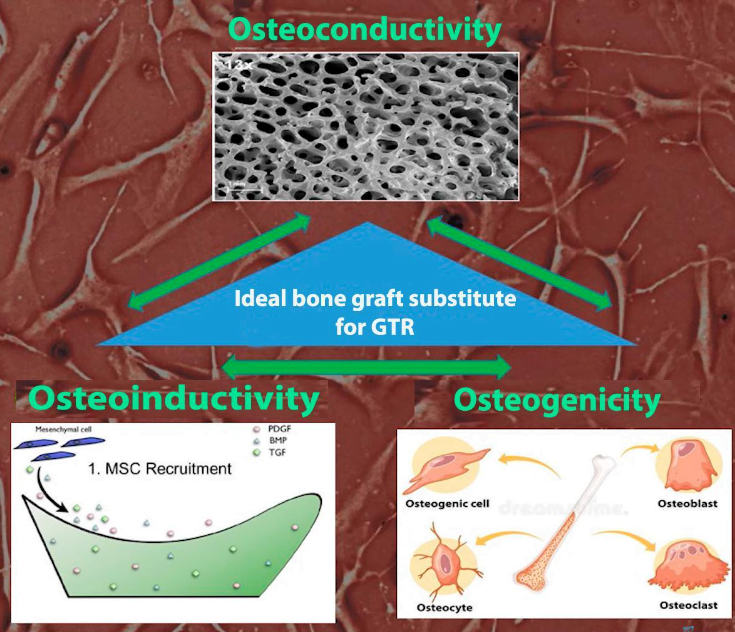
In the previous part of our series, we reviewed the advantages of bone material for NKR obtained from the patient’s body. We concluded that it is the “gold standard” in modern dentistry, because autologous bone maximally meets all three criteria of an ideal bone material:
- Osteoconduction – structural support for vascular formation and new bone growth.
- Osteoinduction – the content of proteins and other active factors that stimulate and support the proliferation and differentiation of precursor cells into osteoblasts.
- Osteogenicity – the content of living cells (osteoblasts or osteoblast precursors) that can form new bone if placed in the proper conditions.
In this article, we will examine why, despite all their advantages, autogenous bone cannot fully cover all the needs of modern dentists; and, what are the advantages and disadvantages of alternative sources of bone material such as:
- Allogeneic – bone materials taken from another person;
- Xenogenic – bone materials taken from animals;
- Alloplastic – artificial materials that mimic the structure and chemical properties of human bone.
Why Autogenous Bone, although the “gold standard,” is not enough
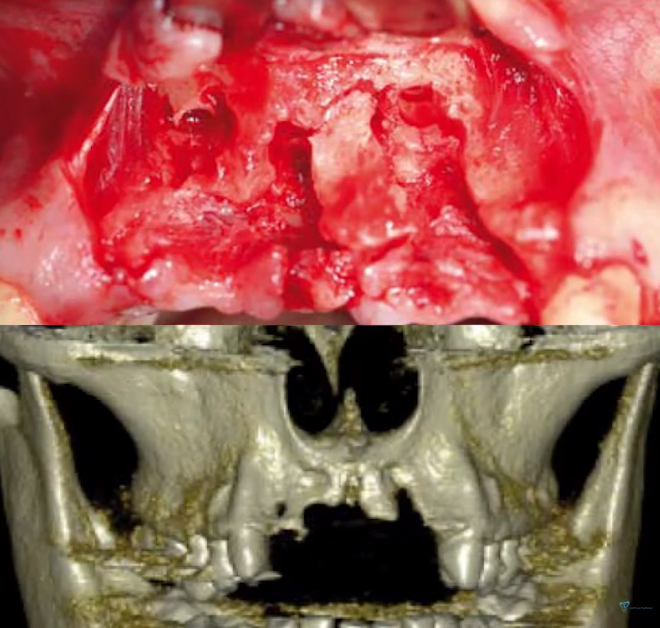
- For all the advantages of autologous bone material, it is difficult to obtain the right amount. There are not many areas in the oral cavity from where bone material can be extracted, and you need a lot of it, especially if the bone defects are extensive as shown in the illustration below.
- In addition, the collection of a large volume of autogenous material is a painful procedure and is associated with a risk of complications.
- Autogenous bone transplanted to another location is quickly resorbed again. This is the dilemma: the bone material engrafts very quickly and with high quality, but the processes that originally led to a reduction in the width of the alveolar ridge are repeated.
Therefore, ways have been found to obtain bone materials that can simply be taken out of the jar in the right amount, prepared for use, and filled the bone defect. There are no problems with collecting the right amount of bone and painful healing for the patient. Let’s take a closer look at what other bone sources there are and how they differ.
Allogeneic bone materials
The treated bone from another person is usually of cadaveric origin, but there are variants of obtaining bone materials from living donors as well. For example, taken during joint replacement surgery, etc.
Back in 1965, a talented researcher named Jurist discovered that demineralized, dried (lyophilized) human bone tissue when placed in rabbit muscle tissue began to form an osteoid. After a couple of months there was an area with ectopic bone tissue in a place where it should not, in principle, be.
Over time, the production of bone material was put on stream. Because not only dentists need large amounts of bone material, but also orthopedists, trauma surgeons and other specialists who deal with a significant deficit of bone tissue. Therefore, lyophilized bone has quickly become a “star” in the medical materials market.
After processing, allogeneic bone material is almost completely devoid of osteoinductive properties and completely lacks osteogenic factors because all proteins, not to mention living cells, are destroyed. However, the main properties of bone material remain, namely osteoconductivity. That is, the allograft creates a structural matrix on the same basis on which our own bone tissue develops.
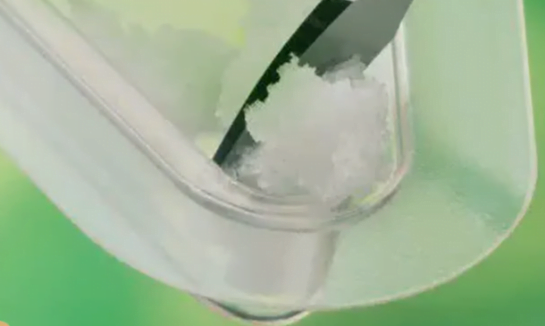
Bone material taken out of the jar is not ready for use right away. During processing, not only all protein structures and living cells are destroyed in it, but also almost all moisture is removed, which reduces the strength characteristics of the bone material. The residual moisture of the allograft from the jar is no more than 5%, so it must be soaked before use. This requires adding a small amount of saline to return the mechanical properties to an acceptable level.
In addition to standard allografts (deproteinized and lyophilized) there are also demineralized bone materials. If you treat the bone material with nitric acid, hydroxyapatite dissolves and you get a soft spongy material that retains its porous structure.
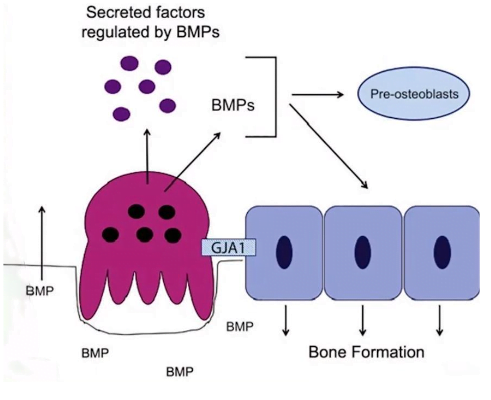
Demineralized bone material also has its own value. An interesting effect is observed – the demineralized preparation partially returns osteoinductive properties. In the process of demineralization, bone morphogenic proteins BMP2 are released from deep structures, which can attract preosteoblasts and other cells into the wound and accelerate the healing process.
In fact, this effect did not always manifest itself and there were quite a few contradictory studies, until a 2007 study by Dr. Schwartz’s group appeared. In which the dependence of morphogenic properties on the quality of bone material, namely on the age of the donor, was described.
The results of this study confirm that commercial allogeneic demineralized lyophilized bone materials vary in their ability to induce new bone formation. Some batches had no activity at all. This study suggests that the ability of demineralized bone grafts to induce new bone formation depends on age, but not on the gender of the donors.
That is, the younger the bone donor, the greater the ability to induce bone formation.
Unfortunately, when dentists buy a new drug it is almost impossible to know which donors it was obtained from, and the details of technological processes are a trade secret.
Therefore, we recommend using only proven bone materials that have demonstrated their effectiveness in practice.
With regard to bone type, we recommend using a mixture of cortical and cancellous bone in most cases. Especially when it comes to volumetric augmentations. In some cases cortical bone material can be used alone. Rarely, however, can bone material derived from cancellous bone be used.
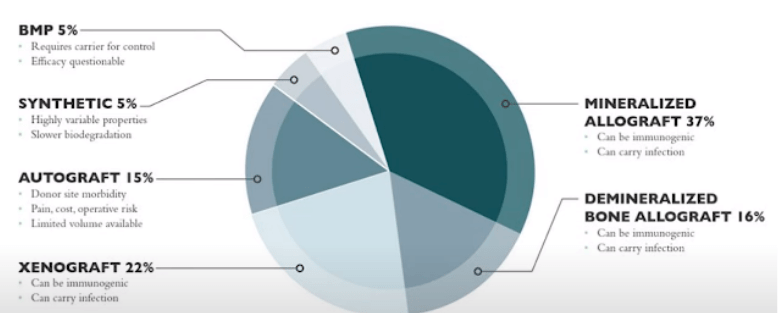
In the U.S. market, allografts account for almost half of the market for bone replacement materials in dentistry. That’s a lot, because the situation in Europe is very different. Until recently there was a ban on the use of allografts. Therefore, in Europe the technology of xenografts was actively developed, which we will talk about later.
Scientists all over the world are working on the problem of how to improve the allograft. Here are the first successes:
- A mixture of 70% mineralized and 30% demineralized bone is just now gaining popularity in the United States. This mixture has serious advantages because of its osteoinductive properties. Of course, it still cannot be a substitute for autogenous bone, but it is a much better solution than dried mineralized bone.
- Preparation of the bone nutrient medium we mentioned in the last article. To do this you need to add the patient’s blood to the already moistened bone material. Better yet, add autogenous bone together with the blood, because very often during the surgery some of the patient’s own bone material remains. For example, bone debris that was left on the coils of the drill when the implant was inserted.
- Adding platelet-rich plasma directly into the bone graft. In addition to improving the biological properties of the material – it is also convenient, because due to the consistency of the plasma from the bone graft you can make a sticky lump (sticky bone, as dentists say), which is very convenient to fill the bone even with a very complex configuration.
Safety and ethical aspects of the use of allogeneic bone materials
- Lyophilized and deproteinized bone materials based on human bone materials have been used for more than 50 years. During this time not a single case of infection or transfer of any type of infection has been recorded. The treatment methods are sufficient to exclude the slightest possibility of infection. There are still questions about the quality of the material, which depends on the age of the donor and not on the method of processing and preparation of the bone material.
- The use of allogeneic grafts does not contradict or prohibit the main world religions (Islam, Christianity, Buddhism, Judaism).
- Resistance to resorption of allogeneic bone preparations is higher compared to the patient’s own bone. Yes, allogeneic grafts also resorb, but it is much slower. This means that the osteoconductivity of allogeneic material is higher compared to autologous material. This leads to a practical recommendation that a 25-50% surplus of bone material should be placed during surgery. To compensate for future resorption.
Xenogenic bone transplants
Bone materials of animal origin (bovine, pig or horse bone) are also deservedly popular. The key advantages of xenogeneic materials are:
- There are no problems with harvesting bone material. Cattle are plentiful and any amount of bone can be put on the market.
- There are absolutely no legal, moral and ethical problems with obtaining bone tissue from animals.
- Xenogenic bone materials are almost not resorbed by the body, which means there is less risk of “shrinkage” of new bone tissue.
There are limitations. The main one is the outbreak of spongiform encephalopathy in cattle in the 1980s in Europe and parts of Asia. The cause was found to be the fact that sick animals were fed bone meal from other animals, and the prion protein pathogen of the disease was ingested. That is, the process of processing animal tissues into feed could not destroy these protein compounds. It is extremely difficult to destroy these proteins, special sterilization processes are needed. There are even recommendations to dispose of instruments that came into contact with infected tissues, because it was more expensive to sterilize these instruments than to buy new ones.
Once in the human body, these protein compounds cause Creutzfeldt-Jakob disease. This is currently an incurable disease with a 100% fatality rate. It is impossible to guarantee that there are no prions in the bone material of animals, even if the animal was healthy.
Therefore, all European countries have a rule that all bone materials of animal origin must be heat-treated at no less than 800°C. At these temperatures the prions are destroyed. This explains why there are no vacuum-assisted lyophilized and sterilized with antibiotics and cold xenogeneic grafts.
Interesting results were obtained in the development of technology for obtaining suitable for transplantation bone materials in Switzerland. It has long been known that bovine or porcine femur is very similar to human bone in its structure. The Bern group was looking for a way to process the bone material that would enable the highest quality transplant to be obtained for medical use. In their research, it was found that some specimens resorbed very quickly, while others did not resorb at all. There were several samples with intermediate properties. At first, the research team wanted to discard the extreme results as unpromising, but Professor Schenk insisted on keeping all samples and conducting research to the end especially since the study had already been conducted on animals. Thanks to Professor Schenck’s intuition and foresight, the very sample of bone material that did not resorb at all became a commercial Bio-Oss product from Geistlich.
The problem of bone resorption is very difficult to solve, and it is specific to each person. For some people, the augmented bone resorption occurs after 1.5-2 months, for others after six months, and for others even after a year there is almost no loss of bone volume. That is why a universal product that solves the problem of resorption is exactly what the specialists have been waiting for. Obviously, only a product that does not resorb at all had such universal properties.
Interestingly, Bio-Oss is a so-called low-temperature product. The treatment temperature does not exceed 350°C. At first glance, this seems to contradict the requirement that all bone materials must be heat-treated to a temperature of at least 800°C, but the point is in the source of the original bone material. The fact is that bovine bone is shipped from New Zealand, where not a single case of spongiform encephalopathy of cattle has been reported. Therefore, the company was able to obtain permission to use a preparation made using low-temperature technology.
Many studies have been conducted to prove that Bio-Oss bone material is indeed pure, does not cause an inflammatory reaction and is suitable for use. Resistance to resorption was also confirmed, the osteoclasts that were adsorbed on the surface could not demineralize and destroy the structure of the bone material.
Many manufacturers have tried to replicate Geistlich’s approach and many have succeeded, to varying degrees. However, many manufacturers continue to use high-temperature treatment, so you can find very different preparations on the market. All of them have been tested and are suitable for use, nevertheless the effectiveness in clinical practice can vary significantly.
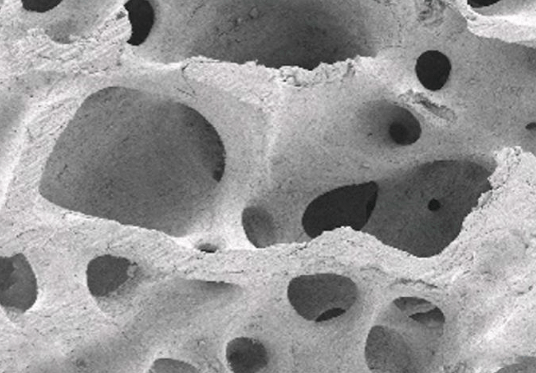
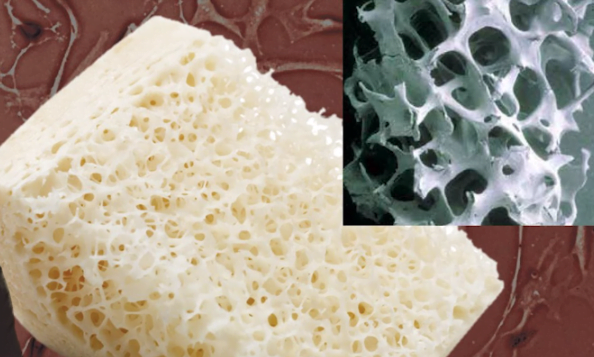
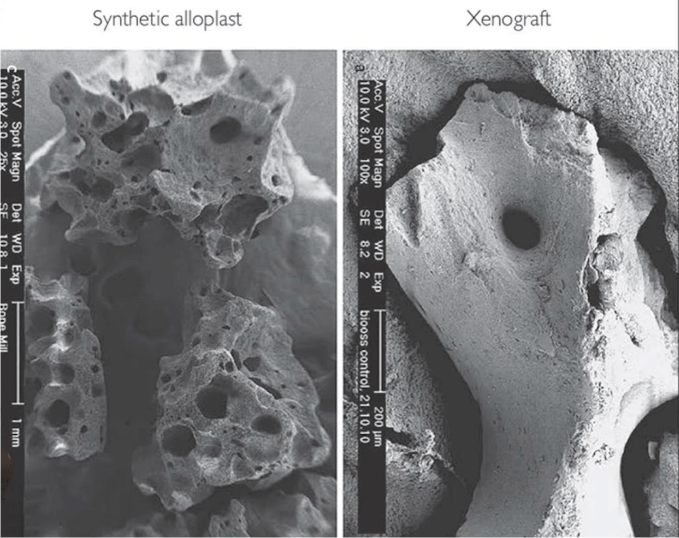
The main difference between the high-temperature and low-temperature material is that at temperatures above 800 ° C sintering and mineral structures in a vitreous form occurs. Because of this, one of the key properties of a bone graft is partially lost, namely, the porous structure of the bone matrix.
The changes are not critical as long as enough pores of at least 300 μm remain.
The main advantage of xenogenic bone material is its resistance to resorption. It is superior to allogenic bone in this respect and certainly many times more resistant than autogenous bone.
This is confirmed by a 2018 study published by Drs. Boshard and Valentini.
It describes a clinical case in which fragments of xenogeneic bone material were preserved 20 years after sinus elevator surgery in which pure Bio-Oss bone material was used.
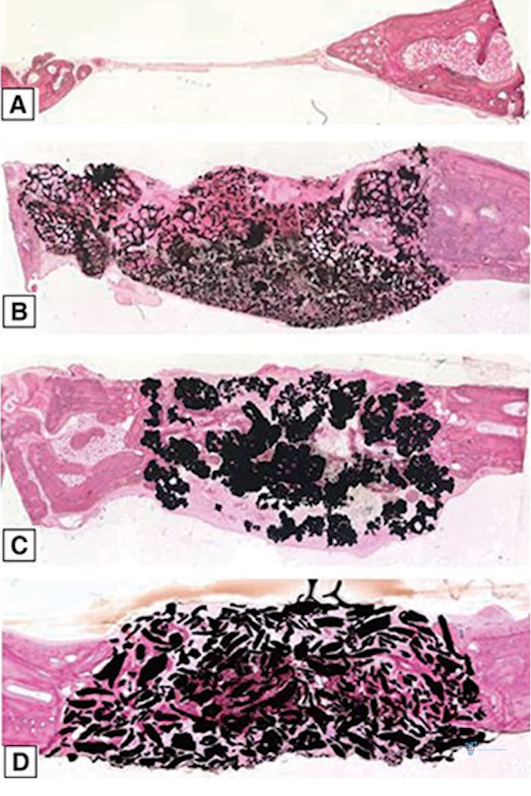
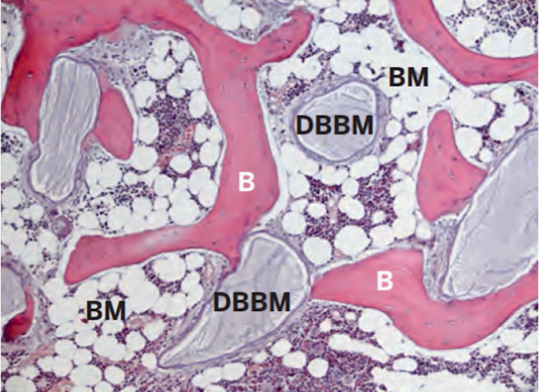
The histological picture was preserved and was taken 6 and 12 months after surgery. At that time, a column of bone tissue was taken for histological studies prior to implant placement.
Then the patient showed up 20 years later with peri-implantitis and a tissue sample was taken again for research. Only this time it was not taken transcrestally, but laterally perpendicular to the alveolar ridge.
The illustration below clearly shows how the condition of the bone tissue changed. The preparation after 6 months looks intensely purple and has the maximum bone graft content.
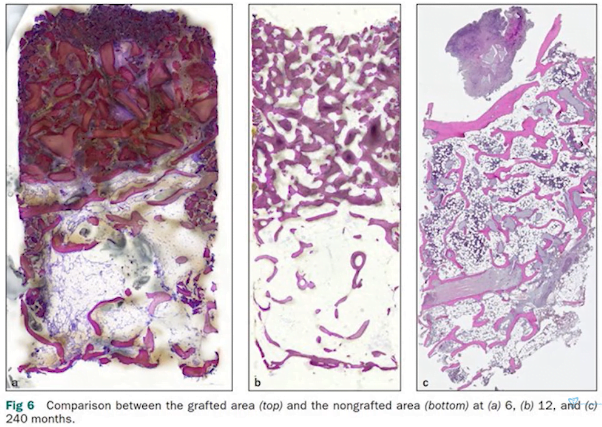
Histological specimens after sinus elevator surgery at 6, 12, and 240 months (20 years) after surgery.
The histology taken 12 months later also shows a crumb of xenogeneic bone preparation, but you can see light areas that are the patient’s own bone. Most interesting is the third preparation, which was taken 20 years after surgery. Look at the enlarged image of the histologic slice with notations.
- DBBM – Bio-Oss xenograft fragments;
- B – patient’s own bone;
- BM – bone marrow spaces.
The results of the study confirm that xenografts can be used to produce healthy and functional bone tissue that can last for decades without any limitations.
Other manufacturers cannot yet boast of such long studies, but since the structure and properties of most xenogeneic materials are similar, the results of application will also be similar. The main thing is for the material to reach the conditional point of nonresorbability.
Currently, New Zealand and Australian specialists are conducting research and experiments with the temperature regime. The main goal is to find out the minimum temperature at which the drug will be completely sterilized and the osteoconductive properties will be maximal. They found that lowering the temperature below 160°C makes no sense because the osteoinductive properties do not improve, but rather the tendency to resorption increases. The optimum range was determined to be from 160 to 400°C and, as we remember, the first company that started to use the low-temperature method was heat-treating the bone material at 350°C, which falls within the optimum range.
Let’s highlight the main things you need to know about xenografts:
- They have the highest osteoconductivity due to resistance to resorption. Bone grafts do not lose volume unlike allografts and especially autografts. In the photo below the xenograft particle is covered by osteoclasts, which cannot dissolve the bone material.
- Absolutely zero osteoinductivity and osteogenicity. It is erroneous to believe that allogeneic preparations are better. It is the same there, except for mixtures with demineralized components.
- When planning the surgery, you need to consider where the bone material will be placed. When it comes to a sinus elevator any bone material is suitable, and a xenograft is even preferable because it retains the original volume. This is due to the fact that this area has a well-developed vascular network and a lot of power sources on all sides. Another case is when the thickness of the alveolar ridge of the lower jaw must be increased on the vestibular side. There the bone material is in contact on one side with the cortical layer, which has few blood vessels. On the other side it is covered by a barrier membrane, through which some nutrients seep, but this is not comparable to the full nutrition through blood vessels. In such cases, new bone is actively formed on the surface of the bone graft, while in the depths there may be some osteoid with an incompletely formed structure. For example, Dr. Jensen et al. found that 32±9.5% of Bio-Oss particles remained intact 14-80 months after graft placement, and 70.3±14.5% of the particle surface was covered by bone. Which confirms that the center of bone grafts is not remodeled. There are several ways to improve the situation and give osteoinductive and osteogenic properties to an alien bone transplant:
- Creating a bone nutrient medium by adding the patient’s blood to the bone material was discussed in detail in part two of our series;
- Using a mixture of autogenous and xenogenic bone material. To understand the second method, let’s review the results of the experiment from 2020.

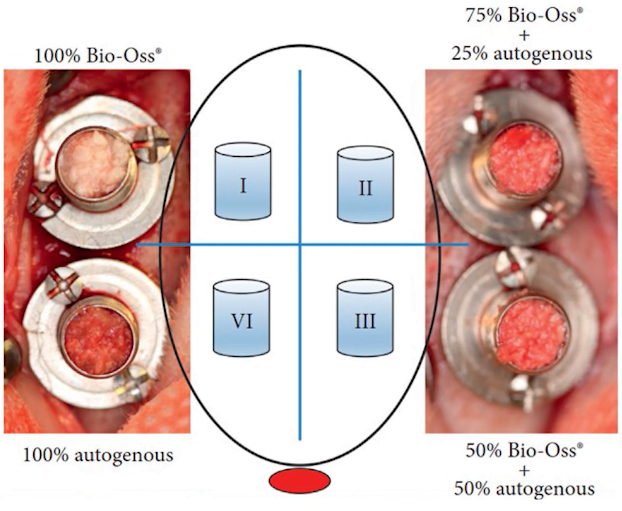
The study was performed on rabbits with hollow cylinders inserted into the bone with different combinations of bone materials.
- In the first one, there was 100% xenograft;
- In the second 75% xenograft + 25% autologous bone;
- In the third one, xenogeneity and autogeneity were 50-50;
- In the fourth, 100% autologous bone.
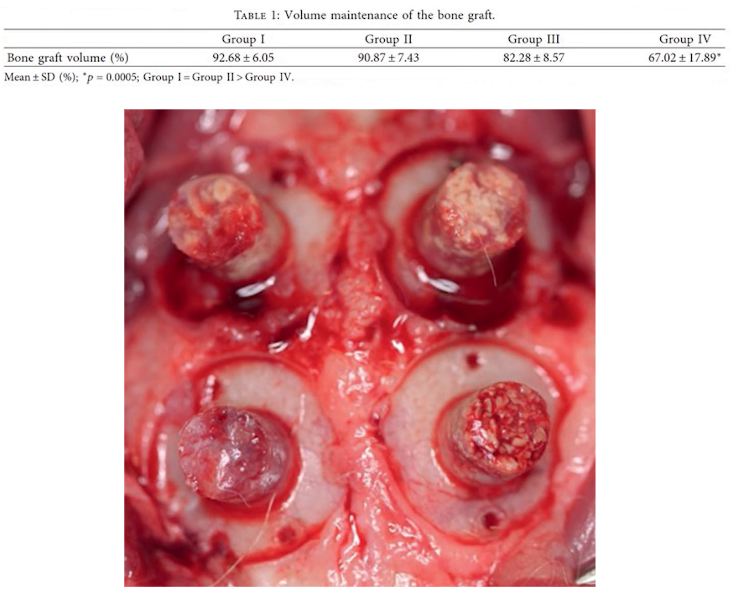
As a result, the greatest bone volume loss was in the case with 100% autologous bone, and the minimal bone volume loss was in the case with pure xenogeneic graft, see the table below.
Therefore, it is recommended to make a mixture of autogenous and xenogeneic bone in case of volume defects in the lower jaw region. This once again confirms the recommendation from our first article – collect the patient’s autologous bone. Even a small portion of autologous bone (25% or more) added to the bone material will significantly improve bone quality, and the xenogeneic graft will preserve the volume of the augmentation.
Even if this is not done in simple cases, the overall strength and response to trauma of xenograft-based bone is commensurate with the patient’s native bone.
How allogeneic, xenogeneic, and alloplastic transplants are derived –
How they differ and what they have in common
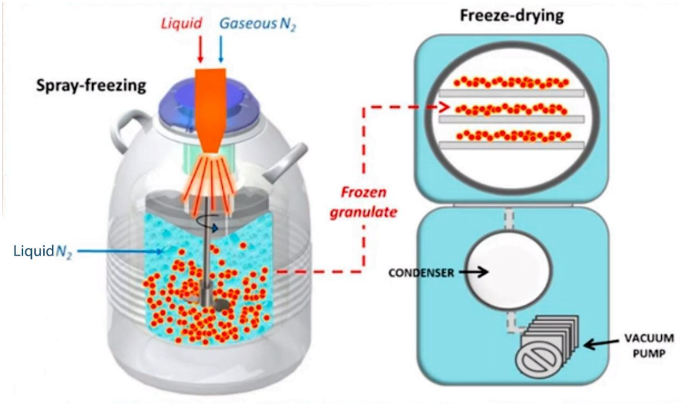
Allogeneic bone must be processed properly. The main step is the lyophilization process, also called sublimation. Let us briefly understand the essence of the process.
- The isolated bone block is crushed and treated several times with antibiotics. For this purpose, it is placed in a concentrated solution, which is renewed several times.
- Then there is a low-temperature treatment (-50-70 ° C) with liquid nitrogen.
- Then comes the vacuum drying stage, during which almost all the moisture is removed. At the same time the drug is not exposed to high temperatures.
As a result of these manipulations, living cells and complex protein compounds are destroyed and only the mineral part of the bone remains. This is the goal of allogeneic bone processing. As a result, only the mineralized spongy structure remains, completely free of antigenic properties. For this purpose all protein structures are destroyed.
Cortical bone material and cancellous bone material are available separately, but in most cases mixtures of cortical and cancellous bone material are suitable for guided bone regeneration. The particle size of the bone material also varies, for dentistry the particle size of 0.5-1 mm is the best.
Xenogenic bone material is obtained in a completely different way. We won’t go into details, but the essence of the process is as follows:
- Mechanical grinding, washing.
- Alkaline treatment.
- Thermal processing at a pressure of 800 to 1200 ° C.
- Drying and packing the material.
Allogeneic and xenogenic bone materials and religious prohibitions
It is worth mentioning that collagen membranes for directed bone regeneration are made from porcine dermis. There is a clear determination by the clergy of Islamic countries and Israel that these materials are approved for use in these countries as pure medical preparations that improve human life.
The same applies to xenogenic bone materials derived not only from bovine bone, but also from pig bone.
There is a certain group of specialists who adhere to holistic principles in medicine. They prefer to use autogenous and allogenic bone materials and do not recommend using xenografts. There are a number of studies that have not found evidence of the effectiveness of holistic medicine compared to traditional medicine. However, this currently continues to be quite popular.
Alloplastic bone preparations
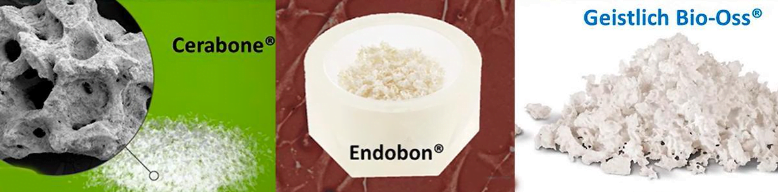
In detail, successful directed bone regeneration simply requires hydroxyapatite with a porous structure of a suitable configuration. It can be obtained from many sources, for example, sea corals are a source of xenogenic bone material, although not very common.
Hydroxyapatite can be synthesized and obtained in unlimited amounts, and there are such preparations, such as BoneCeramicTM, which contains 40% – β-tricalcium phosphate and 60% hydroxyapatite.
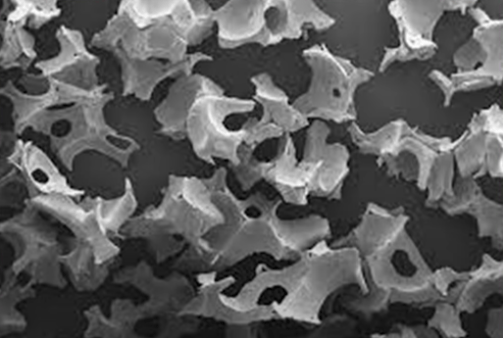
The main challenge is to create a microporous structure similar to natural bone. It is a feasible task for chemists and technologists. Of course, if you look under a microscope, you can see the differences from the materials of biological origin, but nevertheless alloplastic bone material has osteoconductive properties.
When alloplastic materials first appeared, it was pure hydroxyapatite, and its properties resembled xenograft after high-temperature treatment. That is, it practically did not resorb, had good osteoconductivity and complete absence of osteoinductivity and osteogenicity.
However, during research it was discovered that the addition of β-tricalcium phosphate gave an excellent result and the growth of new bone tissue accelerated. It is certainly not osteoinductive as in the case of autografts. Scientists do not yet fully understand how it works, but the fact remains. However, β-tricalcium phosphate dissolves very quickly, so a mixture of β-tricalcium phosphate and hydroxyapatite is considered a successful option.
These are working preparations that are successfully used all over the world. Nevertheless, their structure is different from biological bone preparations, which can be clearly seen in the photo below.
Their properties are inferior to those of biological bone preparations, so they still occupy a small part of the market. However, this is a promising industry and in the future there will certainly be new methods and technologies that will improve the properties of alloplastic materials.
Summary – what improves the properties of allogeneic and xenogeneic grafts and accelerates the formation of new bone?
We did not include alloplastic bone materials in the results because they occupy an insignificant share of the market. Once again, we remind you that all bone materials, except autogenous, have only osteoconductivity. To improve the properties there are several methods to “revitalize” these bone materials.
| Method | Allotransplants | Xenotransplants |
| Adding the patient’s blood to the mixture – nutrient bone medium | Works well | Works well |
| Adding platelet-rich plasma not only speeds up healing, but also makes the clump of bone material sticky, which is important when filling defects with complex configurations | Works well | Works well |
| Adding autologous bone | Works well if you add at least 25% of the total transplant volume | Works well if you add at least 25% of the total transplant volume |
| Adding the demineralized part of the bone material to the mixture | Improves material properties, partially returns osteoinductive properties | Not applicable because after heat treatment all protein structures are destroyed |
We hope this article was of interest to you. See you in future publications.