Plasma Therapy (PRF Clots): Indications and Contraindications
Contents
In our articles on sinus lift and prosthetics, we have repeatedly mentioned PRF clots, which are used to accelerate wound healing. But we haven’t gone into detail about what it is, how to obtain a PRF clot, and how many tubes are needed for a particular wound. The time has come to correct this omission.
Why Plasma Therapy Works
Plasma therapy uses the patient’s own blood, from which red blood cells are removed via centrifugation. The remaining plasma and living cells, such as platelets and leukocytes, along with the fibrous protein fibrin, are used to accelerate wound healing.
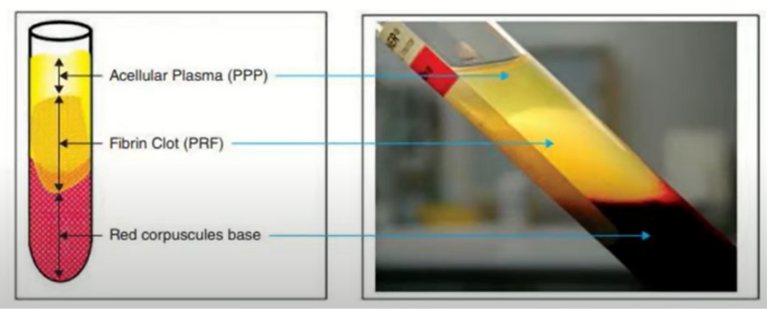
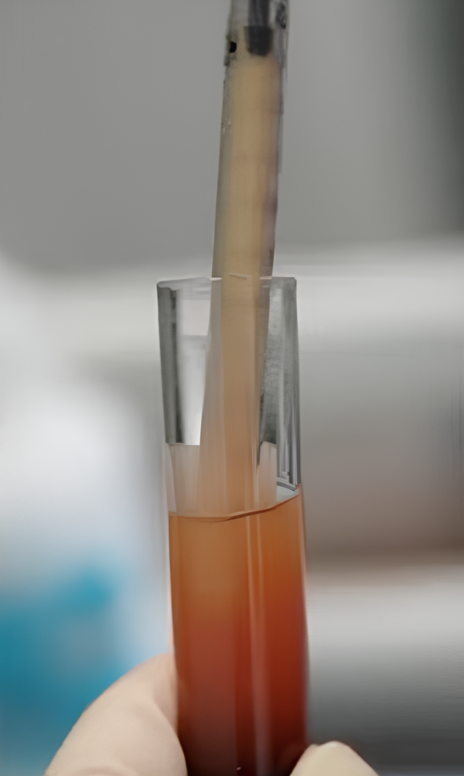
The patient’s blood is divided into fractions, from which the middle part is used for plasma therapy – a fibrin clot enriched with platelets and leukocytes YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Initially, preparations were based on plasma enriched with platelets and a small amount of fibrin – PRP (Platelet-Rich Plasma). Subsequently, PRF (Platelet-Rich Fibrin) technology emerged, which, in addition to platelets and leukocytes, contains an extremely high concentration of the fibrous protein fibrin. Anticoagulants were added to the initial plasma therapy preparations; specifically, they were pre-added to the collection tubes during manufacturing, providing doctors with sterile, individually packaged tubes containing an anticoagulant. This was done to prevent platelets from coagulating too quickly and inhibiting growth factor release.
Actively enriched plasma, combined with an anticoagulant, began to be used in 1998.
Then, a modification called PRGF (Plasma Rich in Growth Factors) appeared. This involved altering the centrifugation protocol to further increase platelet concentration. This method also requires the addition of an anticoagulant and is most often used in cosmetology (plasma lift).
Finally, since 2001, PRF technology has been used. The clot is obtained through a single centrifugation process without the addition of anticoagulants. The tubes for obtaining all PRF variants are empty (i.e., without anticoagulants), sterile, and individually packaged. It is crucial that PRF preparation eliminates the need for anticoagulants and subsequent activators. Platelets are immediately in the active phase and begin to function immediately after applying the preparation. While PRF should be used immediately after preparation, this is not a significant limitation in dentistry and maxillofacial surgery, as operations rarely exceed 40 minutes, ensuring complete preservation of cell activity during this period.
The PRF technique yields two products: a liquid, injectable version and a jelly-like clot.
The jelly-like PRF clot is most often used in dental operations. Once living cells enter the affected area, they release growth factors that the body naturally produces during healing. By introducing enriched plasma into the site of injury, a high concentration of platelets is created, far exceeding the body’s natural production capacity.
In addition, the fibrin-rich PRF clot has a jelly-like consistency. When excess liquid is removed and the clot compacted, it can serve as a physical barrier, protecting the wound site from infections and foreign substances. A membrane or plug can be formed from the PRF clot after squeezing out excess liquid; this will be described in more detail below.
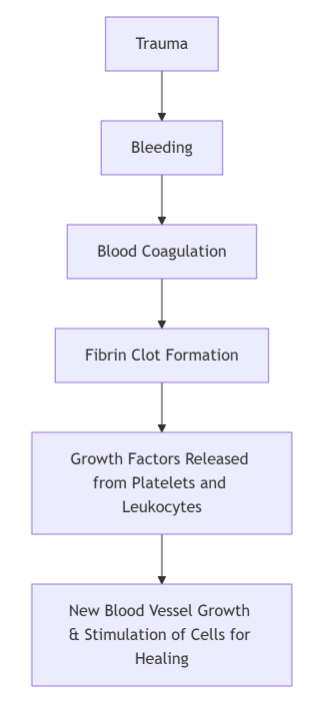
Let us remind you how the wound healing process occurs, see the diagram below.
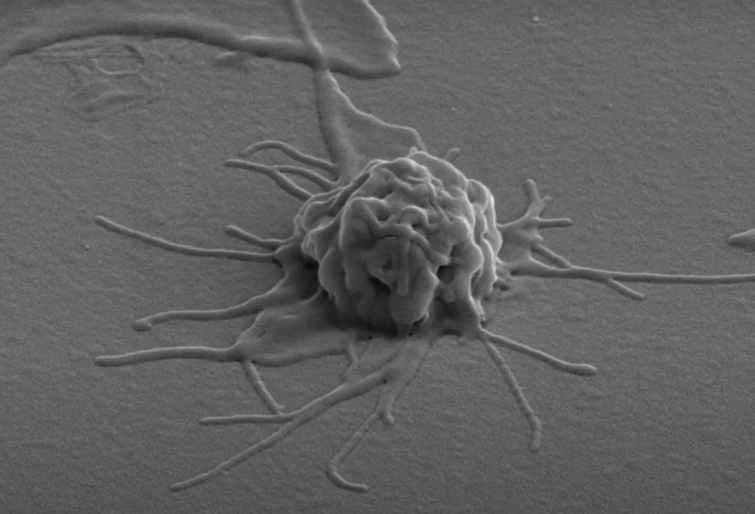
It is important to understand that platelets are constantly present in the bloodstream, but in an inactive phase. In this state, they appear as aggregates or balls of coarse threads. However, when bleeding begins, platelets enter the active phase at the site of blood vessel damage. They extend processes (pseudopodia), see illustration below, which they use to adhere to each other and to the walls of blood vessels at the injury site. The process of forming a clot from platelets (thrombus) is called coagulation. It is only in the active phase that platelets release the growth factors listed below.
Plasma therapy increases the concentration of active platelets and leukocytes at the injury site, accelerating the healing process from the coagulation stage to complete healing.
Key Benefits of Plasma Therapy
- It is impossible to create the same effect using medications because growth factors are present in living cells in specific proportions that are difficult to replicate when creating drugs from individual components.
- The risk of immunological incompatibility is eliminated since the preparations are derived from the patient’s own blood.
- There is no risk of infection transmission, as the basis is the patient’s own biological material, and all manipulations are performed with sterile, disposable instruments.
Growth Factors Important in Healing
(The concentration of which is increased by plasma therapy at the site of application)
There are many growth factors (more than 150) that function in the human body. Here are some of the most well-known:
- IGF (Insulin-like Growth Factor): Stimulates stem cell differentiation, enhances bone metabolism, and collagen synthesis.
- PDGF (Platelet-Derived Growth Factor): Contains signal peptides, produced by platelets and macrophages. Transforms cells that have appropriate receptors. Activates the proliferation and migration of mesenchymal (osteogenic) cells. Stimulates angiogenesis.
- EGF (Epidermal Growth Factor): Stimulates fibroblast proliferation and fibronectin synthesis.
- FGF (Fibroblast Growth Factor): Produced by endothelial cells, macrophages, osteoblasts, and platelets. Causes expression in bone tissue, angiogenesis, and ossification.
- TGF-β (Transforming Growth Factor Beta): Induces differentiation of mesenchymal cells, causes a variety of cellular and intercellular responses, including the production of other growth factors.
- PDEGF (Platelet-Derived Endothelial Cell Growth Factor): An enzyme that maintains blood vessel integrity.
- VEGF (Vascular Endothelial Growth Factor): Participates in angiogenesis, induces proliferation of vascular endothelial cells. It is a heparin-binding protein.
During the recovery period after dental surgery, the first three growth factors from this list are most important. The others also contribute, but without the first three, their effect would be less noticeable.
Why are Live Platelets the Basis of Plasma Therapy?
Because almost all of the listed growth factors are secreted by platelets, and only in the active phase. Therefore, it is extremely important to keep the platelets alive and active at the time of introducing platelet-rich plasma into the wound. Common functions of platelets:
- Platelets participate in multi-stage blood coagulation processes: thrombus formation and blood clot retraction, performing a hemostatic function.
- The reparative function in wound healing is one of the most important.
- Antibacterial activity, in particular, platelets can resist Staphylococcus aureus.
Therefore, manufacturers of tubes and other equipment compete with each other, claiming that only their devices can obtain and maintain the maximum concentration of living, active platelets.
But along with platelets, plasma also contains leukocytes. These are immune system cells that release cytokines and chemokines, which in turn control the intensity of the inflammatory response, preventing excessive inflammation that can slow healing. In open wounds, leukocytes perform another important function: recognizing “self.” Leukocytes not only identify pathogens as foreign and requiring removal, but without their marking as “friend,” the body’s own platelets introduced from outside would be rejected.
In What Other Cases, Besides the Healing of Surgical Wounds, is Plasma Therapy Effective?
- Acute inflammation of traumatic and other origins: Any surgical intervention leads to a phase of acute inflammation. A special case of acute inflammation that responds well to plasma therapy is alveolitis.
- Chronic inflammation: Increasing the concentration of platelets in this area allows you to break the vicious circle of improvements and exacerbations by artificially stimulating tissues for chemotaxis, proliferation, and differentiation of cells. In dentistry, this includes the treatment of periodontitis. Platelet-rich plasma stimulates the growth of new blood vessels, and pale, weak gums become pink and healthier again.
- Plasma therapy can improve the condition of healthy tissues without inflammation: This is an example of anti-aging therapy. Platelet epidermal growth factor suppresses the gene responsible for aging, stimulating the activity and growth of skin cells.
Classification of Preparations for Plasma Therapy
At the time of writing, the following classification was proposed. As agreed upon by experts from Switzerland, the USA, Italy, Poland, Sweden, Holland, and South Korea, all PRP preparations are divided into 4 categories depending on the content of leukocytes and fibrin in them:
- Pure Platelet-Rich Plasma (P-PRP): Obtained using a blood separator (PRP separator) using Vivostat PRF Anitua`s PRGF methods
- Leukocyte- and Platelet-Rich Plasma (L-PRP): Preparation methods – Curacen, Regen, Plateltex, SmartPReP, PCCS, Magellan GPS PRP. A temporary anticoagulant is used in the preparation. The centrifugation tube already comes with an anticoagulant (citrate phosphate glucose). This is the most modern option.
- Pure Platelet-Rich Fibrin (P-PRF): Preparation method – fibrinet
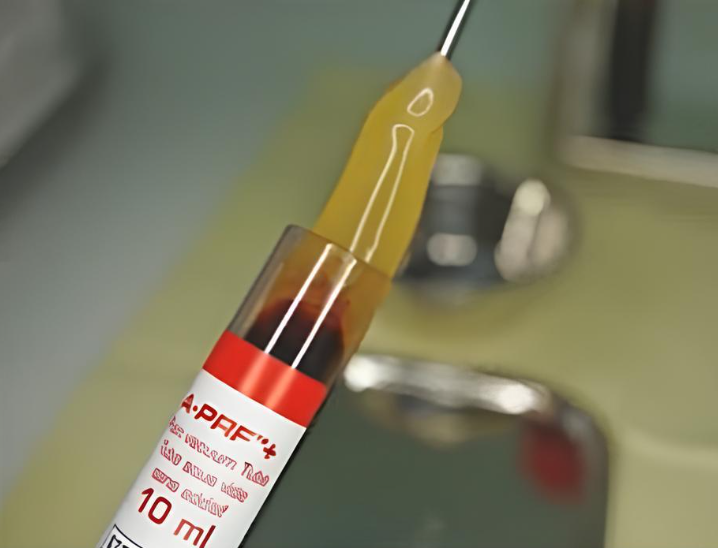
- Leukocyte- and Platelet-Rich Fibrin (L-PRF): Choukroun’s PRF: A-PRF, I-PRF. This is the newest variety with new methods of obtaining the preparation. In dentistry, these variants of preparations for plasma therapy are most often used. Anticoagulants are not used for this technology, so the “lifetime” of the preparation is short, it is advisable to use it in the first 15-20 minutes, maximum within an hour. Since dental operations last on average 40 minutes, the activity of the PRF clot is sufficient. Tubes for the PRF technique are sterile and do not contain any foreign substances.
Why PRF is the “Favorite” Technique of Surgeons and Dentists
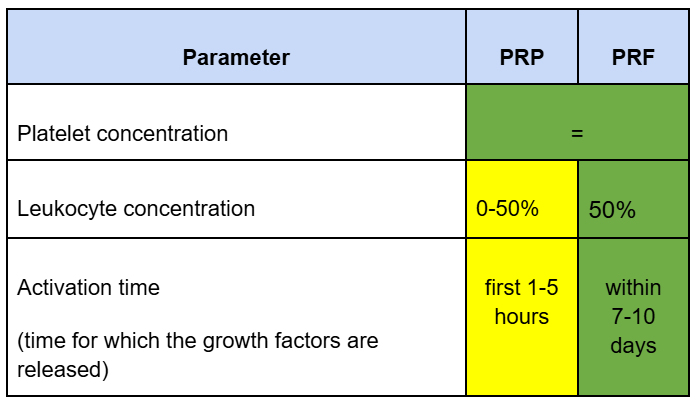
It is enough to compare the composition and concentration of individual components. If, subject to blood processing technology, the concentration of platelets in the PRP PRF clot is the same, then the concentration of leukocytes and the duration of the release of growth factors differ significantly in favor of the PRF technology.
It is enough to compare the composition and concentration of individual components. If, subject to blood processing technology, the concentration of platelets in the PRP PRF clot is the same, then the concentration of leukocytes and the duration of the release of growth factors differ significantly in favor of the PRF technology.
This is easy enough to explain. When receiving PRP, the centrifuge speed is much higher, and a significant portion of the leukocytes settle along with the red blood cells. Therefore, there are significantly more leukocytes in PRF.
As for the time of activation and release of growth factors, PRP is always a liquid suitable for injection, and the duration of action after administration is short, from 30 minutes to several hours. In PRF, a fibrin clot serves as a physiological matrix (framework) in which platelets and leukocytes live and gradually release growth factors for quite a long time. And 7-10 days is just the period of complete healing of a small wound.
How to Prepare Liquid and Jelly Form of PRF
From the patient’s blood, two products with a high fibrin content enriched with platelets and leukocytes can be obtained.
- Clot PRF or Clotted PRF, also known as A-PRF (Advanced Platelet-Rich Fibrin): A jelly-like form that is used either unchanged or in the form of a pressed membrane or crushed mass. For example, a membrane made from a PRF clot is used to cover surgical wounds, including the separation of bone graft and mucosa. And the crushed PRF clot is added to the mixture of bone chips of autogenous and xenogeneic origin. If you add enough crushed Clot PRF to the bone crumbs, you can get a plastic mass with a consistency reminiscent of plasticine. This is important for cases when it is necessary to form a new bone contour.

Extraction of Clot PRF from a tube after centrifugation YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- Liquid PRF is a liquid form for injection, which is also labeled as I-PRF (Injectable Platelet-Rich Fibrin): In dentistry, the injectable form is used, for example, to treat periodontitis. Liquid PRF is a relatively new product. But it is worth remembering that plasma therapy is not the only and sufficient method of treatment. This is a safe and effective, but still auxiliary technique.
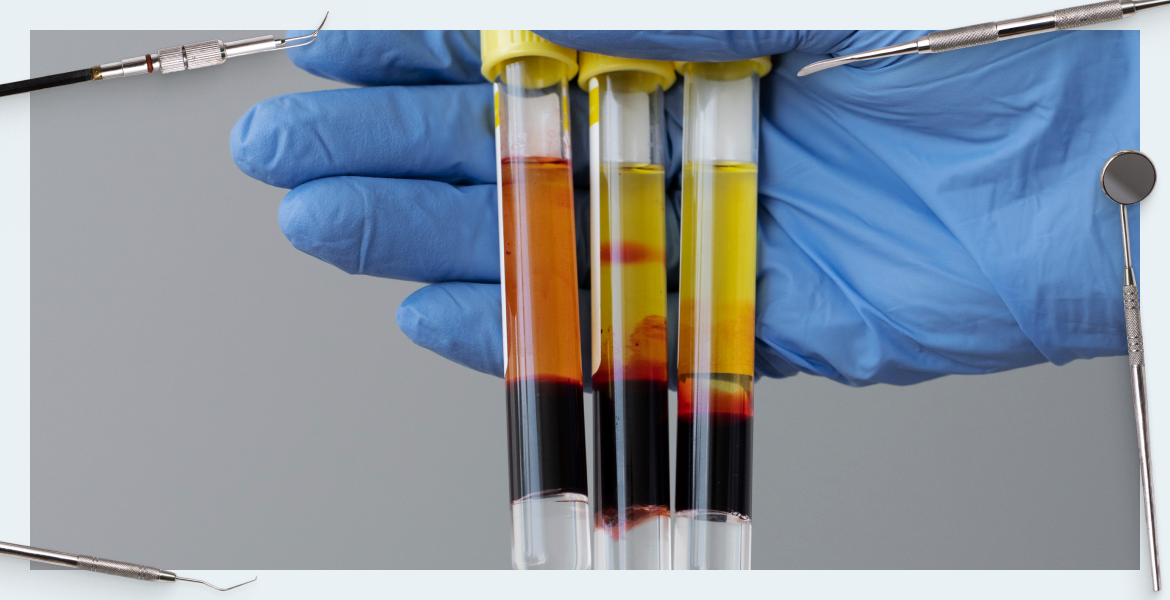
Both types of PRF are obtained from the same blood, using the same centrifuge to obtain PRF drugs. The only difference is the speed of rotation and the time of exposure to the blood. Also, different tubes are used for each type of PRF. Let’s look at this in more detail.
1. Clot PRF: Special red glass tubes are used for obtaining. It is difficult to confuse them; they are marked Clot PRF or A-PRF. The red tubes are rough inside, this promotes the formation of a jelly-like clot of fibrin fibers, which contains platelets and leukocytes.
So, we take blood from the patient’s vein with a peripheral venous catheter with a diameter of at least 19 G (the diameter is important to keep the blood cells intact and alive). We place the test tubes in a special centrifuge, where we process them at a speed of 1300 rpm for 8 minutes. This time and speed were determined experimentally; at these values, the maximum number of living cells is preserved and a clot of acceptable size and density is formed. If you change the time and/or number of revolutions, then either the clot will be thinner or there will be fewer growth factors. Then with the PRF clot you can do everything we mentioned above:
- apply unchanged to close wounds
- squeeze with a sterile cloth or use a special box and get a fibrin membrane 1.5-2 mm thick (not to be confused with collagen), also in a special box you can form a plug from the clot, which is very convenient for closing holes after tooth extraction
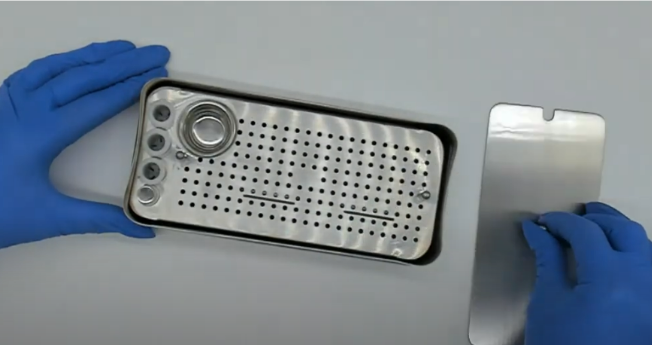
Box for manipulating PRF clots – you can get a membrane, a plug, or mix PRF with osteoplastic material YouTube / Dr. Kamil Khabiev / Dental Guru Academy
- grind and add to the composition of the osteoplastic material.
2. Liquid PRF: Orange plastic tubes are used. The inside is perfectly smooth, which is why the fibrin fibers do not have time to form a clot. Because of this, the usable enriched part of the plasma remains suitable for injection for at least 15-20 minutes. But here a lot depends on the centrifuge; with strong vibrations and unstable temperatures, the “lifetime” of the preparation can be greatly reduced. To obtain injectable PRF, the procedure with blood sampling is the same, but the centrifuge operating time and number of revolutions are much less: 700 rpm for 3 minutes. The amount of usable material is very small; it is a cloudy liquid concentrated in the upper part of the test tube. It is suitable for injection.

Preparation process of Liquid PRF YouTube / Dr. Kamil Khabiev / Dental Guru Academy
On average, men get exactly the same amount of enriched plasma as in the picture above. Due to the menstrual cycle, women obtain slightly more usable plasma.
IMPORTANT! The color of the plasma layer may change a couple of minutes after removing the tube from the centrifuge. It immediately has a reddish tint, and then becomes lighter and yellower. This is normal; during this time, the remaining red blood cells are deposited.
Rules for Working with Liquid Plasma (Liquid PRF)
- Do not open all the tubes at once. After removing them from the centrifuge, place them in a stand and use one at a time as needed. Otherwise, upon contact with oxygen, the plasma will begin to thicken (the coagulation process will begin).
- Draw enriched plasma into the syringe, avoiding the dark layer, and inject it at the place of application. We will discuss the recommended method of administration a little further in this article. Insulin syringes are used to collect plasma, and 27-30G needles are recommended for injection.
Novice specialists may wonder why they need to buy special tubes if they are empty without anticoagulants, etc. After all, you can use ordinary laboratory test tubes with the same volume of 10 ml. We do not recommend this because laboratory tubes are only sterile from the inside, but the special red and orange PRF tubes are completely sterile and are sold individually.
There is also a question about the number of PRF tubes. On average, before surgery, it is recommended to make a stock of 10-12 tubes. For one hole after the removal of the 6th or 7th tooth, 4 test tubes with PRF, or rather plugs made from it, are used. But it all depends on the complexity of the operation. Removing 1-2 teeth is one thing, but the scope of surgical intervention with an open sinus lift is a completely different matter.
IMPORTANT! Learn the “lifetime” of different PRF options:
- Plugs and membranes from pressed PRF: several hours (no more than 2).
- Untreated Clot PRF: it is recommended to use within 15 minutes after opening the tube. For example, to make a membrane or stopper, it is recommended to store the material in the test tube for no more than an hour.
- Injectable Liquid PRF: it is recommended to use immediately; it can remain in a closed tube for about 20 minutes.
Recommendations for Working with a Centrifuge
In addition to the fact that for obtaining PRF preparations there are specialized centrifuges, which differ from laboratory ones in lower speed and temperature conditions, the balance of the centrifuge load is extremely important. The tubes should be distributed evenly, for example, as in the picture below – six tubes are evenly spaced along the mounting holes. The minimum recommended number of tubes is 3; they should be installed as the vertices of an equilateral triangle. But there are tasks when you need to process 2 or even 1 test tube. This can be done, but the two test tubes must be located strictly opposite each other. And in the case of one test tube, a counterweight is required. That is, you definitely need to load another test tube with ballast. Moreover, simply filling a second test tube with saline solution is not the best solution, since the density of blood and saline solution is different and it will be difficult to avoid vibration and beating during operation of the centrifuge. But this also depends on the centrifuge itself; some models cope normally if there are one or several test tubes with water, and some make noticeable noise and vibrate.

Centrifuge for obtaining PRF with test tubes and ready Clot PRF in test tubes YouTube/Dr. Kamil Khabiev / Dental Guru Academy
Rules for Using Liquid and Jelly PRF
Clot PRF
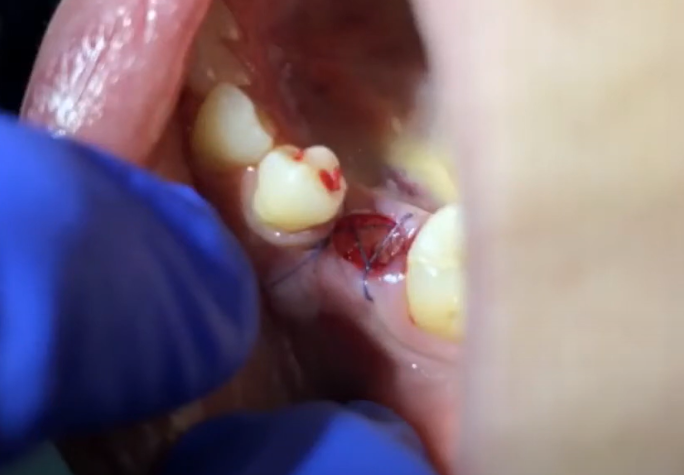
1. Plugs from Clot PRF: The photo below shows one of the most common ways to use Clot PRF clots. First, plugs were formed from the jelly-like clot. A hole like the one in the photo requires several plugs, usually 3-4 pieces. You need to fill the hole quite tightly and at the end you need to press the last PRF plug with a sterile napkin. At the end, we put a simple suture over the hole; it is needed not to tighten the edges of the wound, but to keep the PRF clots inside.
PRF clots may well come into contact with the external environment.
IMPORTANT! Unsqueezed PRF clots have a fairly low density, and if you fill an open well with only them, after a couple of days the well may turn out to be empty. They are either washed out or dissolved. Therefore, at least at the border of the wound there should be either plugs or a membrane of compacted (squeezed out excess liquid) PRF clots.
The same principle applies to single-stage implant installation. If the hole with the implant is closed with PRF plugs, the healing process will occur much faster, and the risk of inflammation is reduced to zero. The picture below shows the option of installing an implant instead of a multi-rooted tooth. Clot PRF in this case solved the problem of wound isolation; there was no need to install a gum former and suture the gum around it.
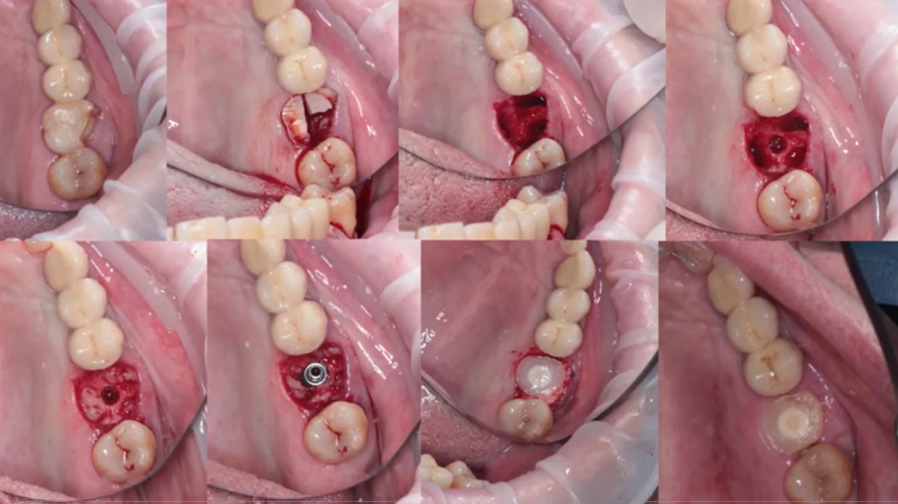
Use of PRF for socket closure after implant placement YouTube / Dr. Kamil Khabiev / Dental Guru Academy
And most importantly, we managed to do without introducing external bone material, which is never completely processed by the body. Having your own native bone around the implant is always the best solution, and Clot PRF will speed up its formation.
And here is how the healing process occurs after using Clot PRF. The picture below shows the situation 2 weeks after tooth extraction. The wells were filled with Clot PRF plugs.

Healing situation 2 weeks after tooth extraction, the sockets were filled and closed with Clot PRF YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Even if the patient does not maintain proper hygiene and skips rinsing, or, on the contrary, rinses the mouth too intensely (which can lead to the washing out of a blood clot), no complications will arise, neither infections nor alveolitis.
Another option for using Clot PRF for simultaneous implantation is shown in the picture below. The thickness of the vestibular wall in this case is sufficient (more than 2 mm), which means the addition of bone material is not necessary. Therefore, the empty space between the implants, bone and soft tissue is simply filled with PRF clots. This helps preserve the entire bone volume that was present during implantation.
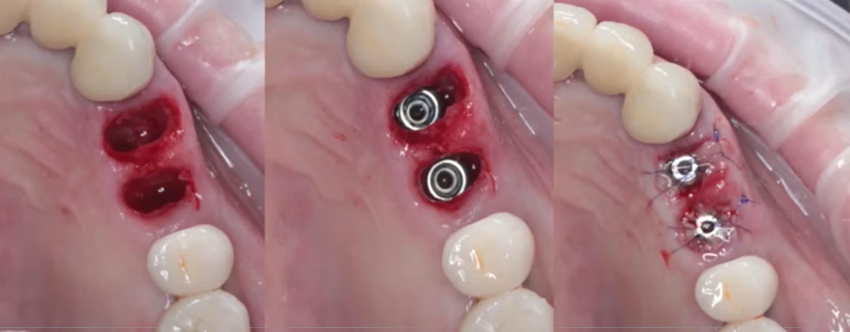
Application of Clot PRF for closing defects during simultaneous implantation YouTube / Dr. Kamil Khabiev / Dental Guru Academy
And if the implants were placed in the front part of the jaw, where the thickness of the vestibular wall is 1-1.5 mm, then a bone graft would be added. But even in this case, Clot PRF is used only in the form of a membrane to separate the osteoplastic material from the mucosa.
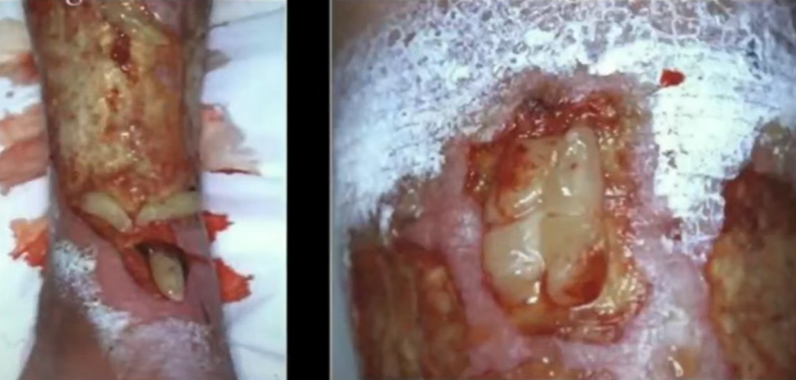
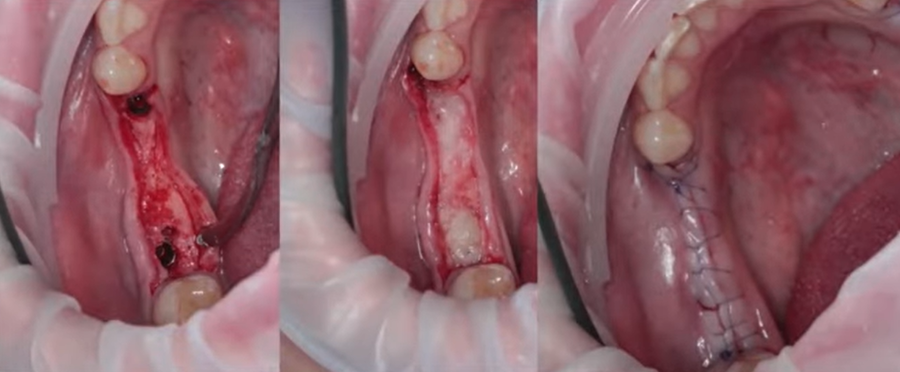
2. PRF clot membrane: Used for larger surgical interventions. An example in a series of pictures below. During sinus lift, the lateral window is filled with osteoplastic material. Then, after the implants are installed, the bone cavity is filled with a bone graft. A PRF membrane is placed as a barrier between the mucosal flap and the bone.

Application of PRF membrane to cover the site of bone grafting surgery (sinus lift) YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The PRF membrane also works great in case of accidental perforation of the Schneiderian membrane. This is not to say that the perforation area can be sealed with tape, but it is very close to that. But this only helps if the membrane is healthy and in good condition and the perforation occurred due to the careless actions of the surgeon. If the membrane is inflamed and covered in adhesions, it makes no sense to use a PRF membrane to eliminate defects. In such difficult cases, it is necessary to interrupt the sinus lift operation and transfer the patient to a specialized specialist to bring the maxillary sinus in order.
With a closed sinus lift, if the thickness of the native bone is more than 5 mm, it is enough to insert a PRF clot into the cavity between the bone and the Schneiderian membrane and everything will heal perfectly and the required volume of additional bone will be formed without the need to introduce osteoplastic material.
But for small defects the PRF membrane is also used. The picture below is an example of simultaneous implantation with immediate loading. To increase the volume of the gum, a PRF membrane was inserted and fixed under it. A bone graft was not used in this case, since the thickness of the external bone wall was more than 2 mm.
Here is another example of the use of a PRF membrane in large-scale surgical interventions that are accompanied by bone grafting. In this case, the PRF membrane is used in the same way as a collagen membrane and covers the defect. It serves as a barrier to prevent epithelial cells from entering the area of bone grafting. Otherwise, instead of bone, the volume of the defect will be filled by soft tissue.
Application of PRF membrane during bone grafting surgery YouTube / Dr. Kamil Khabiev / Dental Guru Academy
It is important to recall once again that a PRF membrane can replace a collagen membrane only in the area of small defects, and where it does not bear a mechanical load, but simply serves as a barrier and a source of growth factors.
The PRF membrane is excellent at promoting healing during soft tissue graft harvesting. Here it is important to fix the membrane, otherwise it will simply fall out of the wound and there will be no effect.

Closure of the defect with a PRF membrane after soft tissue harvesting YouTube / Dr. Kamil Khabiev / Dental Guru Academy
3. To add to the osteoplastic mixture either a crushed PRF clot is used, or an intermediate version is prepared. For this, red Clot PRF tubes are used, the centrifuge operates at 1300 rpm, but the time is not 8, but 3-4 minutes. During this time, the red blood cells have already precipitated, but a jelly-like clot has not yet formed and the material turns out to be quite liquid. This intermediate option is perfect for mixing with bone chips, resulting in a “sticky bone”. This mixture is very easy to work with; it perfectly fills all cavities and holds its shape. Adhesive bone is used both for immediate implantation and for sinus lift and other maxillofacial surgeries.
4. Burn treatment: PRF clots are placed directly on the affected areas in the form of an application.
5. Poorly healing ulcers in diabetes can also be treated with plasma therapy. Clot PRF clots are placed directly into the wound cavity, and over time the ulcers heal, as can be seen in the pictures below.
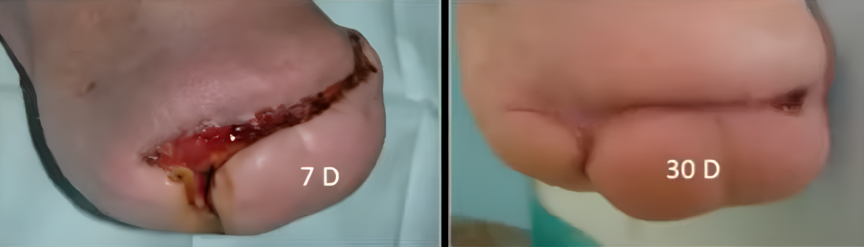
The healing process in case of diabetes using plasma therapy – 7 days after the start of treatment (left) and after 30 days YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Liquid PRF
1. Treatment of gingival recession: One week before surgery to treat gingival recession, single injections of Liquid PRF are given. The photo below shows the difference before and after. The volume of the mucous membrane increased, the color became more pink, which indicates the growth of the capillary network. The chances of successfully ending the recession are increasing.
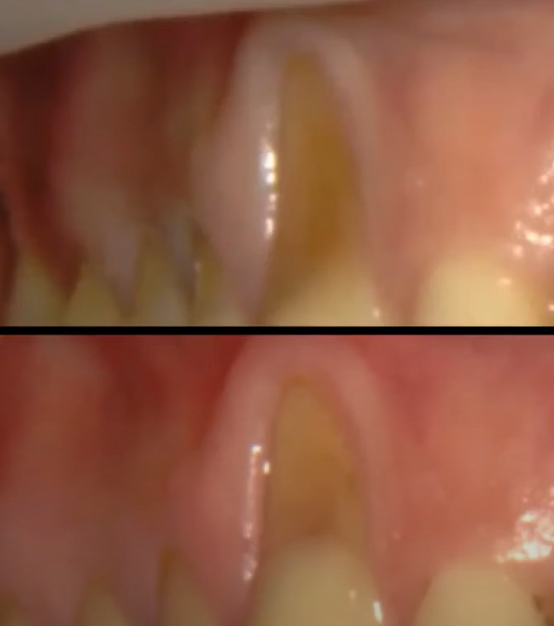
Preparing for surgery to treat gingival recession with Liquid PRF injections YouTube / Dr. Kamil Khabiev / Dental Guru Academy
This case is interesting because only a PRF membrane was used to treat the recession. The operation was carried out without a connective tissue graft and was quite successful. At the same time, there were no additional injuries that are inevitable when collecting a tissue fragment for transplantation.
To work, you need to produce a certain amount of PRF membrane. It is better, of course, to squeeze the PRF clot through a special box press. Please note that several layers of such a membrane will need to be placed under the flap. Flap release and membrane placement and suturing follow a standard protocol for surgical treatment of gingival recession.
Treating gingival recession: before (top) and after (bottom) pictures using PRF membrane only YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Another advantage of the PRF membrane is that it does not have to be completely covered with a flap. If a fragment of the membrane comes into contact with the environment, this will not affect healing in any way.
But it is worth remembering that the use of a PRF membrane instead of a connective tissue graft is limited and there are relatively few such operations. The patient must have a thick gum biotype and several other conditions must meet for such an operation to be successful. But in any case, PRF, both in the form of injections and in the form of a membrane, is successfully used as an auxiliary material.
As for the administration of injectable PRF, it can be administered either with or without infiltration anesthesia. It all depends on the sensitivity of the patient. When administering the preparation slowly, anesthesia is usually not required.
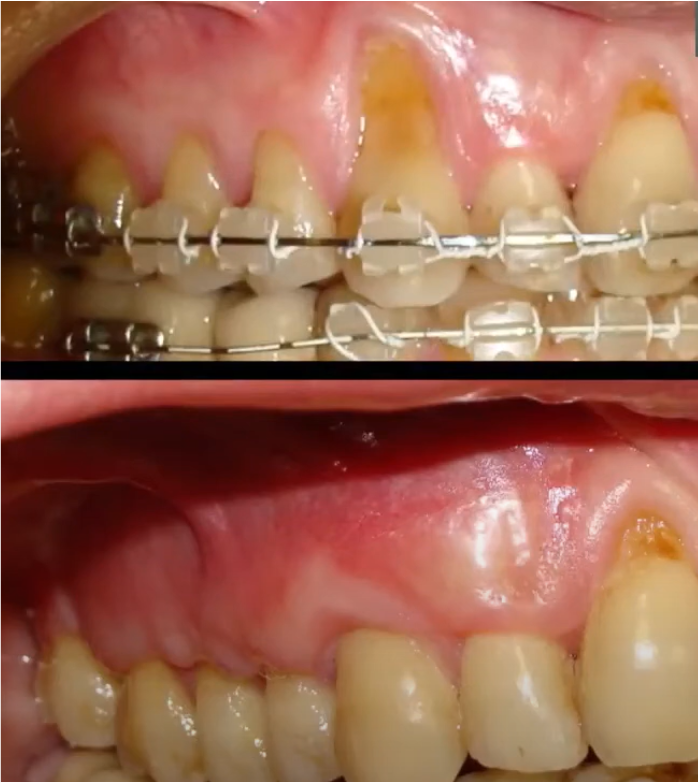
The preparation is injected into the transitional fold and can be an effective addition to the periodontitis treatment protocol.

Injection of Liquid PRF into the transitional fold is used in the treatment of periodontitis, gingival recession and some other diseases YouTube / Dr. Kamil Khabiev / Dental Guru Academy
2. Maintenance injections during open curettage surgery: One series of injections a week before surgery along the transitional fold of the mucosa, and for another 2-3 weeks after the open curettage operation. The volume of injections is 2 ml per jaw. There is no need to stab directly into the problem area – this will cause additional injuries. Let us remember that this surgical procedure is used for deep cleaning of periodontal canals, for example, in severe forms of periodontitis. In such diseases, the mucosa is weak with impaired blood supply (ischemic). Liquid PRF injections help restore blood supply and help increase gum volume.
3. Injections directly into periodontal pockets for severe forms of periodontitis: Before the injection, sanitation is performed to completely remove the biofilm at the injection site.
4. Also, plasma therapy with the injectable form of PRF is successfully used in trichology, but it is also not the only form of treatment.
Dosages of PRF Clots
The required amount is determined by the volume of the bone defect or surgical field. For example, after the removal of molars 7, 8 teeth, an average of 6 plugs from Clot PRF are needed to fill the holes; in the area of 5 teeth, 4 plugs will be enough. And the defects need to be filled tightly until, even with pressure, the new plug sinks into the hole.
Contraindications to Plasma Therapy
First of all, these are oncology and systemic blood diseases, but there are other conditions and even medications that cannot be used with plasma therapy:
- Thrombocytopenia
- Platelet dysfunction syndrome
- Septicemia (extensive sepsis)
- Hypofibrinogenemia
- Anemia
- Oncological diseases are treated with drugs that block growth factors. This is not an absolute contraindication, but all procedures must be agreed with the oncologist.
- Use of corticosteroids (within 2 weeks before procedure)
- Use of NSAIDs and antibiotics (within 48 hours before the procedure). If the operation is extensive, then similar drugs are often used. To get out of this situation, blood is taken before administering sedatives, antibiotics and NSAIDs.
- Active and recent infections
- Acute infectious diseases
- Taking anticoagulants/antiplatelet agents, before the procedure the patient is sent for a coagulogram, and if everything is normal there, blood can be taken for plasma therapy
- Decompensated form of diabetes mellitus
- Systemic connective tissue diseases
- Autoimmune diseases that are treated with immunosuppressants (organ-specific/organ-nonspecific) are also not an absolute contraindication. The decision is made based on analysis