Guided Bone Regeneration. Autologous bone grafts. Part 2

Autologous bone grafts
In the first part of this article series we analyzed different types of barrier membranes for directed bone regeneration from Teflon to collagen membranes. Let us briefly recap the conclusions we came to.
| Membrane type | Recommended application area | Remarks |
| Non-resorbable dPTFE Teflon membranes (reinforced with titanium) | For vertical bone augmentation (increasing the height of the alveolar ridge) | Requires repeated surgery to remove the membrane; also, due to low wettability and adhesion, complications in the form of exposed membranes are common |
| Titanium rigid frames | For the healing of large bone defects, individual titanium skeletons are especially effective | It requires a second surgery to remove the skeleton. It is also not uncommon for complications associated with exposing the titanium from under the soft tissue |
| Non cross-linked collagen membranes | The gold standard for most cases where minor or moderate bone augmentation is required | Completely resorbed by the body. Virtually no complications, no need for repeated surgery |
| Cross-linked collagen membranes | For cases where increased mechanical strength is required. For example, a large volume of bone grafts must be retained and the pins must be anchored to the bone. | Resorb much longer compared to unstitched, which is important if the volume of the defect is large, and the healing will be slow |
This part of the article will focus on bone fillers for GBRs, methods of taking bone material and factors influencing the effectiveness of bone augmentation surgery.
Why you need to fill bone defects for GBR
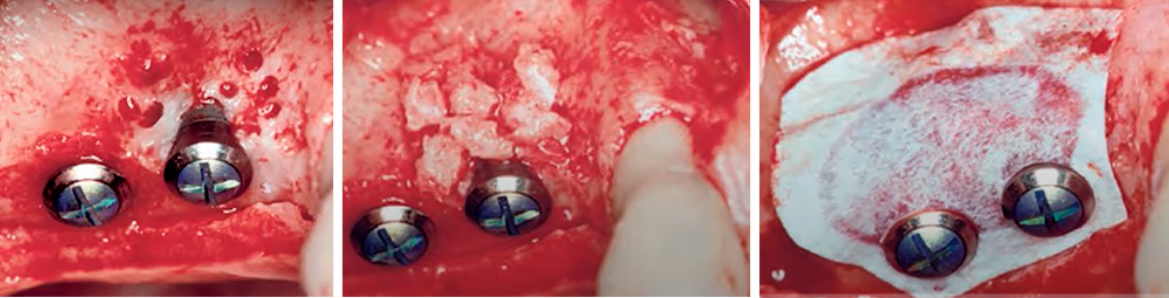
The idea that something should be placed between the membrane and the bone area appeared almost immediately as soon as the method of bone augmentation with barrier membranes appeared, which can be seen in the picture below where you can see the first generations of Teflon membrane.
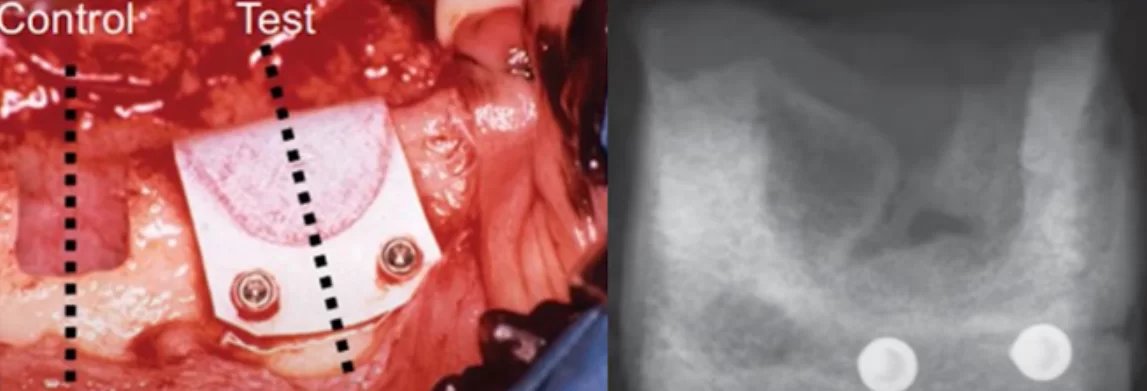
It is quite logical, because the processes of bone tissue healing are well studied. We turn again to Dr. Buser’s experiment that was discussed in detail in the last article. There, experiments were performed on dogs. Saddle notches were made in the bone, one part of which was closed with a Teflon membrane, and the part of the notches not closed with anything and was a control.
As a result, we see that bone tissue is perfectly formed under the blood clot membrane. Blood vessels of the primary bone callus and tissue calcification are formed. At first glance it is not necessary to fill the bone defect.
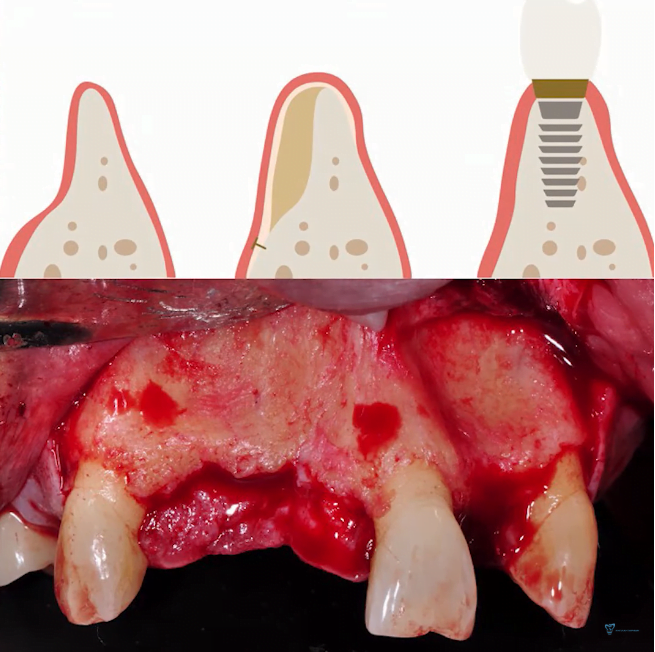
There is a nuance here. The experiment was conducted under “ideal” conditions. Real patients do not have bone defects of such a clear shape. In practice, we most often encounter bone deficiency on the vestibular side (lateral bone defects).
It is common for there to be a slight loss of alveolar ridge height and significant bone loss on the vestibular side a few months after tooth loss. Therefore, restoring bone loss on the vestibular side is of the greatest interest to practicing dentists.
In this position, no matter how hard we try and no matter what membranes we use, there is an almost 100% probability of blood clot shrinkage and the bone tissue will not recover to its proper extent. Therefore, the cavities between the membrane and the existing bone tissue need to be filled with bone material.
Let’s take a closer look at how bones heal and what role blood vessels and granulation tissue play in it. We discussed in detail how bone tissue heals in an article about the processes that occur after a tooth extraction. The healing process is well understood and consists of clearly defined stages: fibrin plaque, granulation formation, primary callus formation and finally bone mineralization.
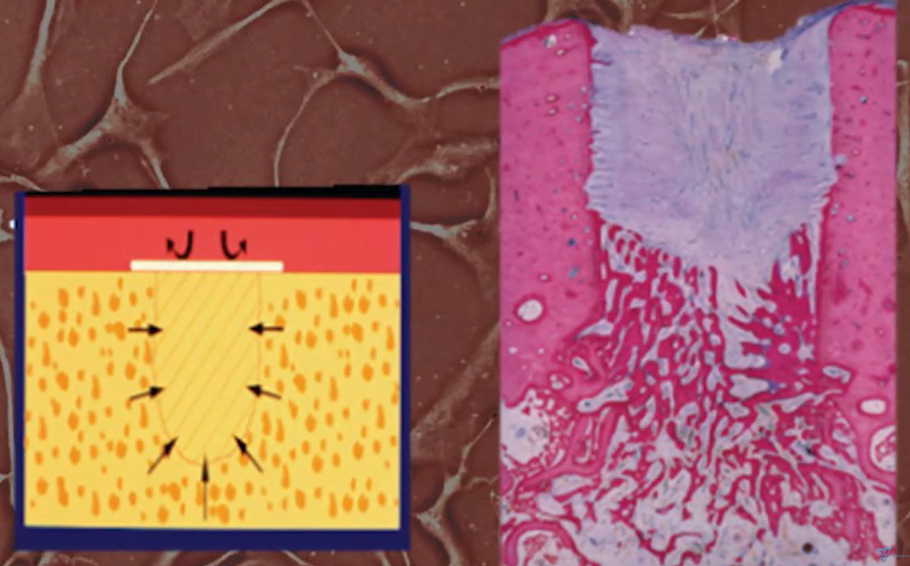
Let us recall the key function of the granulation stage. Bone tissue regeneration requires a formed capillary meshwork. It is the vascular network that provides delivery of growth factors and mesenchymal stem cells (preosteoblasts) to the injury site, where the healing processes take place. For the process of vascularization the granulation tissue is simply necessary – it provides physical support for the growth of blood vessels.
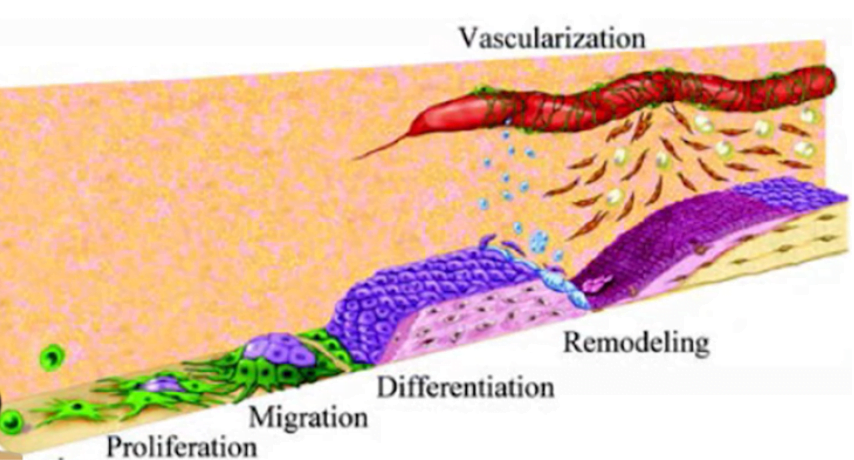
Formation of a blood vessel and its delivery of growth factors and cells that are involved in the healing process
Another scenario of bone healing is possible without the granulation stage. Numerous observations by histologists confirm that intraosseous defects as small as 1 mm heal without granulation formation. This effect was first discovered in animals, and then it was confirmed in humans. It was noted that the healing occurs very quickly, due to the fact that the cell matrix is formed at once, bypassing several stages of the classical healing scheme.
At the time of writing this article, there is no complete understanding of why this happens, but there is a very interesting hunch, which is described by the term – osteogenic jump distance ± 1 mm.
As we mentioned before, a blood vessel cannot grow indefinitely without the support of other tissue types. Apparently the osteogenic jump distance of 1mm is the maximum length that a vascular outgrowth can grow and bone tissue can form without granulation.
Yes, this is still a guess, but so far it is supported by observations.
Now we’re getting closer to understanding why we need bone-plastic materials under the membrane. They are needed to:
- Provide the necessary volume for bone formation, because without a filler, the clot under the membrane tends to decrease in volume and it will not be possible to build up the desired bone thickness;
- To support the growth of blood vessels and accelerate the healing process, because the space between the fragments of bone grafts rarely exceeds 1 mm, so you can start the regeneration process almost without the granulation stage.
What should be the ideal bone filler for GBR?
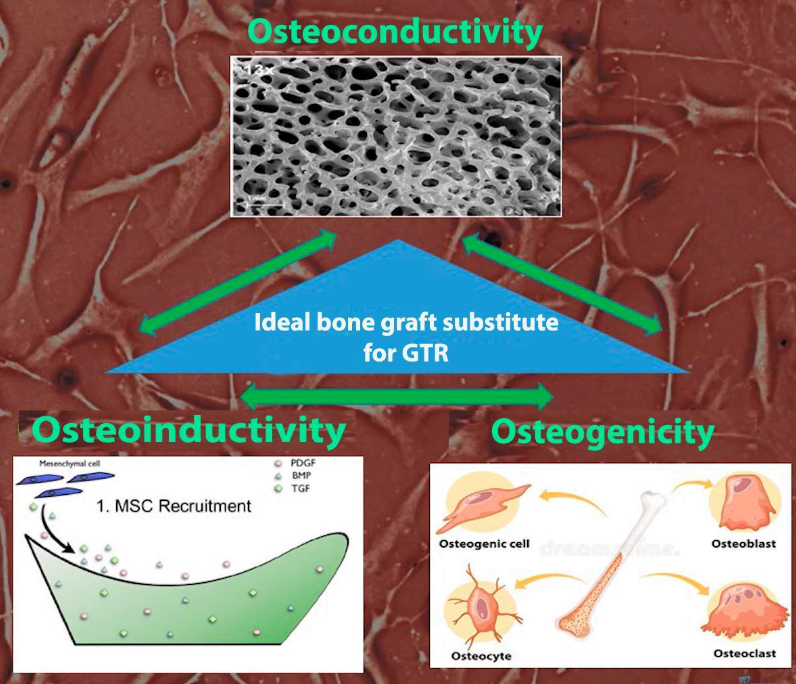
We will first discuss such an important property as osteoconduction. Osteoconductive properties are one of the main requirements to materials for guided bone regeneration. All types of bone grafts have this property regardless of their origin. However, the best material for bone regeneration must meet three criteria that were first described in the book 20 Years of Guided Bone Regeneration in Implant Dentistry (Second Edition):
- Osteoconductive materials are a matrix that serves as a framework (solid base) for the subsequent formation and growth of new bone.
- Osteoinductive materials contain proteins that stimulate and support the proliferation and differentiation of progenitor cells into osteoblasts.
- Osteogenic materials contain cells (osteoblasts or osteoblast precursors) that can form new bone if placed in the proper conditions.
We have now logically come to an understanding of what factors promote healing and growth of new bone tissue, but to fully understand the picture we need to know what prevents healing.
What helps and hinders bone healing?
Let’s start with the factors that impede bone healing.
- Lack of blood supply. If there are no blood vessels, there is no nutrition and no bone growth.
- Mechanical instability. Bones grow slowly, which means that stability in the defect area must be ensured for at least 4 weeks. This is the task of the barrier membrane. For this, they are often reinforced with titanium and pinned to the bone.
- Oversized defects. Without support, blood vessels will not sprout into defects that are too large, which means no new bone will be formed.
- Competing tissues with high proliferative activity are primarily soft tissues, which grow very rapidly and begin to fill the defect in the first hours after traumatic intervention. Barrier membranes just do not let the epithelial cells get to the place where the new bone should grow.
Now let’s look at what contributes to bone growth.
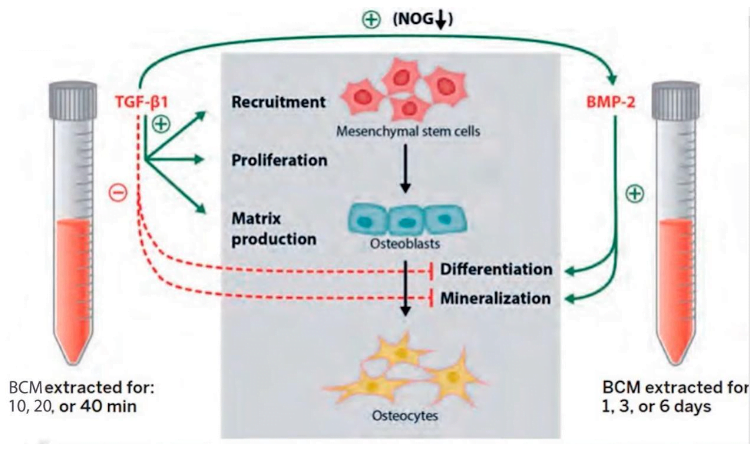
- Osteoinduction by growth factors. These are materials capable of secreting bone-morphogenic proteins (BMP2 transforming growth factor and others), as well as enzymes that stimulate growth and attract MSCs.
- Osteoconduction with autologous bone or a substitute. These are the fillers that are the topic of today’s article.
- The transfer of stem cells that differentiate into osteoblasts. This process occurs without stimulation, but it is also possible to isolate the stem cells separately, place them in the wound and the healing process is accelerated.
- Distraction osteogenesis.
- GBR with the use of barrier membranes.
What bone grafts can be
Here is a short list of materials that are used as fillers in GBRs.
- Autografts are the patient’s own tissues, which we will focus on in this article.
- Allografts are tissues of another person, usually of cadaveric origin.
- Xenografts – tissue from another species (bovine or pig bone, sometimes horse bone).
- Alloplastic materials – synthesized artificially.
Why autogenous bone is the “gold standard” for GBR
The answer is very simple and obvious – it is an ideal bone filler that has all three criteria for the best material, which we described above:
- Osteoconductivity – structural support for new tissue.
- Osteoinductivity – the material contains and releases growth enhancers.
- Osteogenicity – the material contains viable cells that can grow and divide.
Where to get autogenous bone for transplantation
Most often the source of bone material is the patient’s own jaw or skull. For the extraction of a large volume of bone, the branch of the mandible is most often used. This is the area where a sufficiently large volume of bone mass can be safely extracted, including the cortical and cancellous parts.
Also the chin area where, with the right skills, the right amount of bone material can be taken quickly enough.
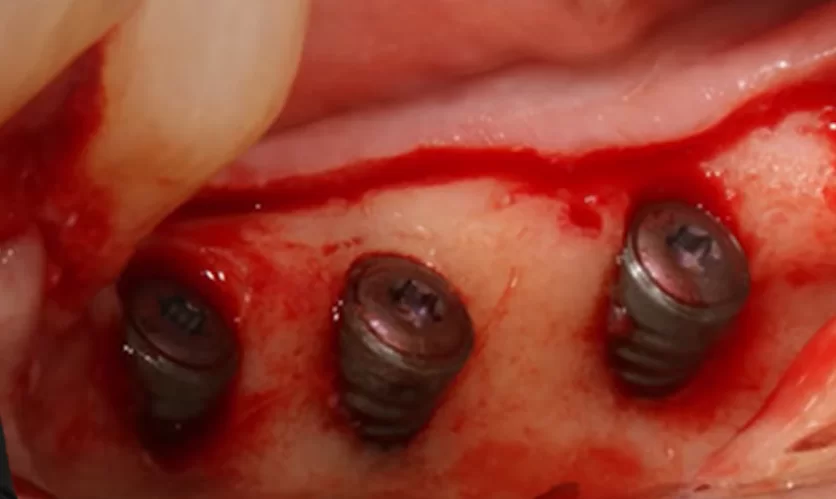
If we are talking about small defects, it is almost always possible to take bone material in the immediate vicinity of the defect. To do this, it is enough to go over with a scraper. If implants were placed at the same time as bone grafting, you can use the bone material that was left during drilling.
There are less commonly used sites for bone harvesting that are used to repair very large bone defects. Unfortunately, the amount of bone in the oral cavity area that can be taken is not that significant. If you have a severely atrophied alveolar ridge, you need to use bone material from other sources as well:
- The iliac crest. You can take a large volume without harming the body. However, because of the predominance of cancellous bone, such a graft is quite strongly resorbed by the body in the new place.
- Ribs are a good enough source of bone tissue.
- Dark bone (very high quality bone material comes out of the skull bones, not worse than from the jaws and chin).
What are the most common bone defects?
More often than not, dentists have to deal with lateral bone defects. That is when there is a bone deficit on the vestibular side of the alveolar ridge. You can see an example of such a clinical case in the picture below.
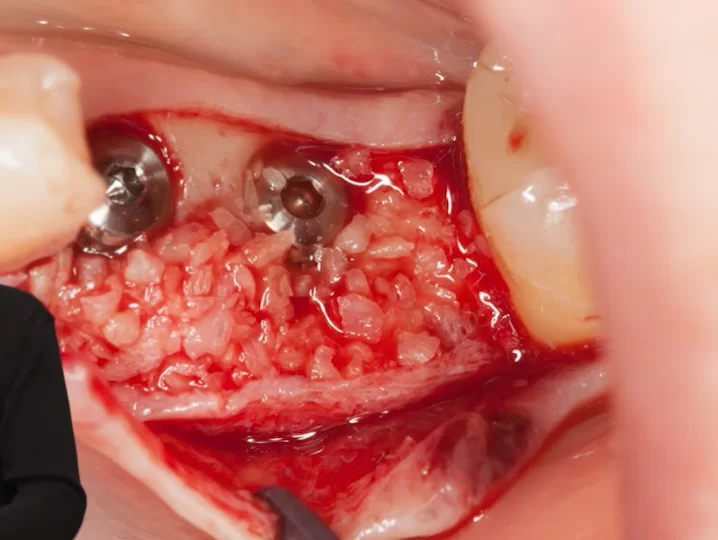
To repair such defects you need a prepared bone material. To do this, a fragment of bone must be extracted in one place, then crushed and placed under the barrier membrane. The photo below shows a prepared bone graft.
What are the most effective methods of taking and preparing bone material?
In this article, we will not discuss in detail the technique of bone grafting with large bone blocks, but it is worth mentioning that such a technique exists and is quite successfully used. Fresh bone flanks have one common problem – vascularization. Spongy part is well vascularized in its new location, and after two to three weeks it is completely riddled with blood vessels, and after a year it is impossible to distinguish between the original bone and the augmented one. However, the cortical layer is vascularized worse because the dense bone plate initially had few blood vessels.
If the bone block is crushed, however, its osteoinductive properties increase by an order of magnitude. There is a powerful stimulation for the development of blood vessels and formation of solid bone tissue.
In addition, by grinding the bone we release osteocytes and other cells that are contained in the structure of the bone block. This allows them to get to work immediately and form new bone tissue.
It is because of these properties that most bone augmentation surgeries are performed using shredded bone material.
Let’s consider the most common methods of obtaining ground bone:
- Using a special mill. To do this, you first need to cut out a bone block and grind it with a hand mill, see the illustrations below.
Small bone fragments are placed in the working cavity of the mill and crushed in a circular motion until a homogeneous bone augmentate is obtained.
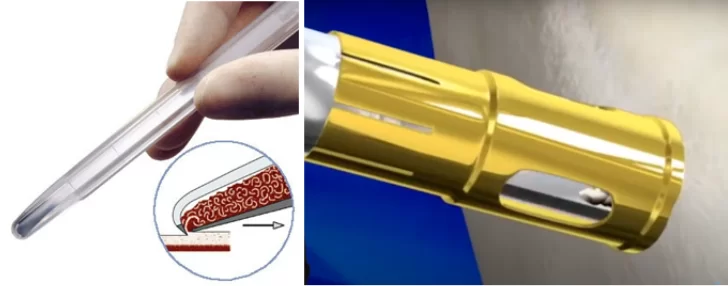
2. A special scraper for collecting bone mass in the immediate vicinity of the surgical site. For example, if we do surgery on the upper jaw, we do not need to do another surgery on the lower jaw to collect bone. The quality of the bone material is also high, but only a small amount of bone graft can be obtained this way.
3. There are also special cutters that allow you to cut out small bone blocks and grind them immediately. There are also cutters that allow you to cut out bone fragments in the form of small columns without shredding.
4. Vacuum bone catchers are similar to the previous option, but the collection goes over the surface of the bone. A special tip scrapes over the bone, and the crumbs are drawn into the cylinder due to the vacuum effect. This is a very convenient method, but the bone particles are very fine and a very fine bone suspension is drawn into the cylinder.
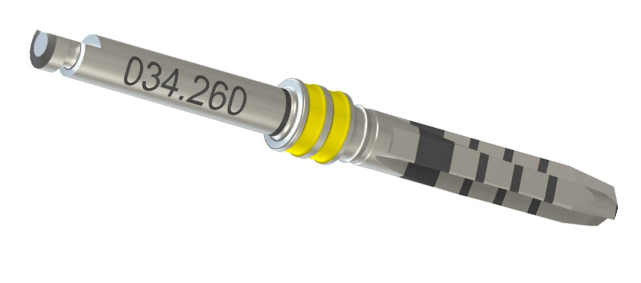
5. Collecting bone material from the drills during the implant surgery. This is the simplest method that does not require special devices, but not all cutters retain enough bone material on the blades. Straumann cutters for the BLT implant series are particularly good in this regard. They retain plenty of bone material in the sulcus even at high speeds and with irrigation.
It is possible to collect bone chips with any drill if you turn off irrigation and work at about 100 rpm. In this mode, the risk of bone overheating is practically zero.
6. Collecting bone material with a piezochirurgical handpiece. However, this is not easy because all piezochirurgical handpieces must be operated with cooling and the bone material is washed away by the flow of coolant.
Bone material obtained by different methods, however, is not of equal quality. There are numerous studies on this and here are the results of one of the highest quality, which has quality illustrations.
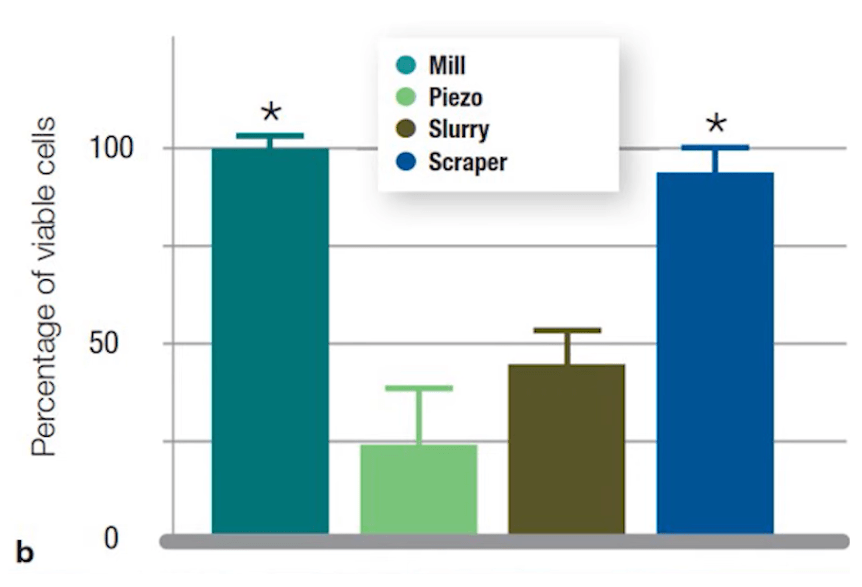
Research shows that some methods cause cell damage and, as a consequence, a sharp decrease in the osteogenicity of the bone material. The size of the particles also matters. If the bone material is crushed into dust, the osteoconductive properties of the filler deteriorate.
The highest live cell content and optimum granularity of the structure are found in bone material obtained by using mills.
Bone material collected by mechanical scrapers is not far behind the leader.
The worst case is the piezochirigic method, obviously a large number of cells are damaged during bone extraction, and irrigation washes out the osteoinductive factors. Nevertheless, it is still a usable bone material.
To summarize, recall that one of the goals of bone crushing is to increase the contact area of fragments with biological fluids and accelerate the formation of whole bone tissue. Here the balance between the number of living cells and the size of bone fragments is important.
Practical recommendations for the use of autologous bone grafts
Everything we describe here has a scientific basis and is supported by clinical evidence. Details can be found in Dr. Buser’s book, which we mentioned more than once in our last article, “30 Years of Directed Bone Regeneration”.
1. Bone-conditioned medium: During his surgeries, whether it was a sinus elevator or something else, Dr. Buser used a sterile syringe to collect some of the patient’s blood that somehow ended up in the surgical area. He would add that blood to the container that contained the bone-plastic material. At the same time he mixed the blood with a small amount of saline solution.
Now, this method is already an established concept and is recommended for wide application. The idea is that a mixture of bone augmentate, blood and saline within about 40 minutes acquires properties that multiply the quality of the augmentate and enhances reparative processes in the defect area.
As an experiment, observations were made on BCM, which was placed in a special installation where cell viability was maintained. As a result, a change in the properties at different time intervals was noted. At later stages the division and differentiation of stem cells and formation of osteoblasts and then osteocytes were observed. All this was outside the human body.
Therefore, we recommend making BCM bone material, especially since it is very simple and does not require any additional equipment. While the site will be prepared just the necessary 30-40 minutes will pass. It is also recommended to soak the membrane in this nutrient medium, if, of course, we are talking about collagen membrane.
2. At every implant surgery, collect some autogenous bone and keep it until the end of the surgery. It can come in handy in many cases. It is not uncommon for a CT scan not to show the whole picture and to reveal small bone defects. For example, the bases of the implants need to be covered, or the alveolar ridge is not thick enough, and you have the material on hand. Of course, we recommend adding some saline and the patient’s blood immediately to get a bone nutrient medium.
Summary
- Autogenous bone material is the gold standard because it best meets the three quality assessment criteria:
– osteoconductivity;
– osteoinductivity;
– osteogenicity. - Not only is the area for bone tissue extraction important, but also the way the bone material is prepared. The best quality is the bone material obtained with a mill or a hand scraper.
- Preparation of bone nutrient medium, when the patient’s blood and saline in equal proportions is added to the bone mass, allows to accelerate the process of bone tissue regeneration.
We hope this article was useful to you, see you in the next article of this series.