Treat or remove a tooth. Part 1 (a guide for Doctors)

This article will focus on the preservation and treatment of teeth diagnosed with periodontitis and will be of primary interest to surgeons and endodontists. It will also benefit orthopedic dentists. The material in this article will be useful not only for young specialists but also for their more experienced colleagues. In this article, we will discuss how to diagnose a tooth for fissures without resorting to complicated equipment and how to treat extensive periodontitis. The material is interesting but lengthy, so it is divided into two parts.
How to determine if there is a crack in the tooth – a basic set of tools
Dentists often have to make a prognosis for the preservation of a tooth during the first examination. If there is not enough experience in treatment and prosthetics, premature conclusions can be drawn and teeth that can be treated and restored may be extracted. As you know, a living tooth is always better than even the best placed implant.
Many people think that in addition to experience it is necessary to use high-precision and expensive equipment like cone beam tomograph. This is only partially true. It is good to be able to use sophisticated equipment, but we will now look at how you can get by with X-rays plus the simplest tools that are available in any dental office.
The restorative prognosis of a tooth is easier to determine than it may seem at first glance, and to do this you will need:
- Gutta-percha pins – they are available in any dental clinic and are very cheap. At the same time they are extremely effective and informative in the examination of root canals.
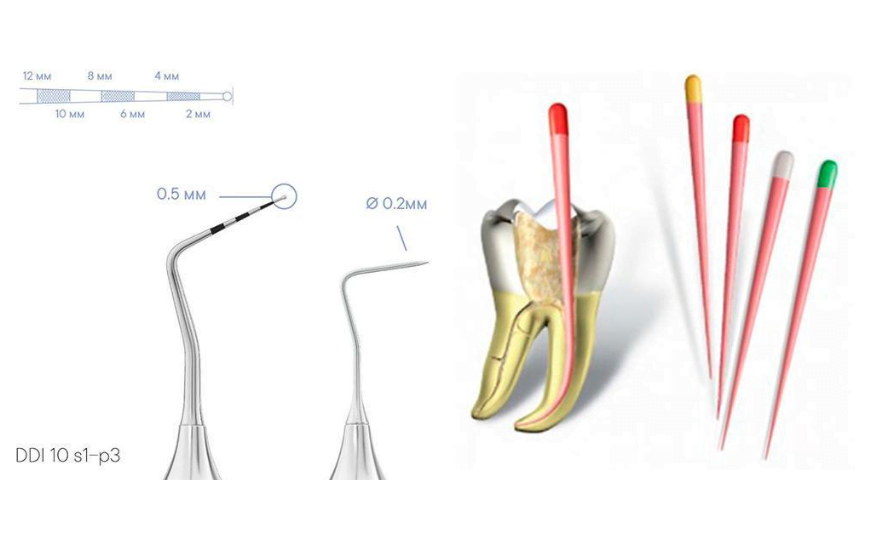
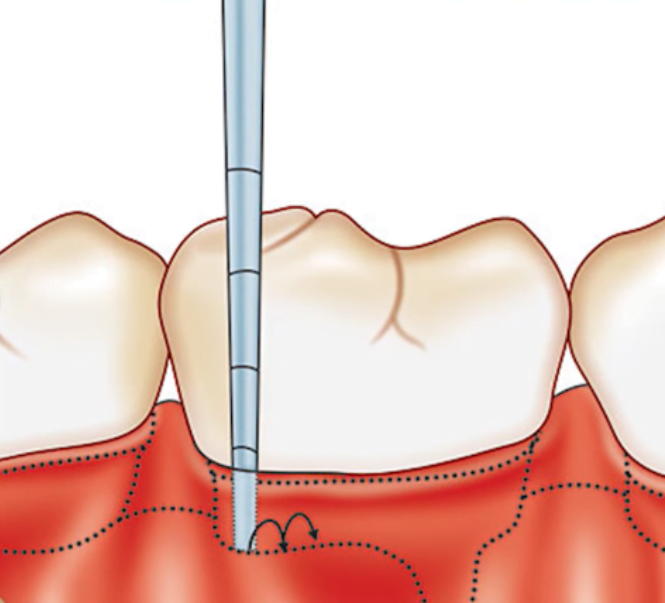
- Periodontal probe. Also the simplest, but very useful tool that allows you to determine if there are any localized periodontal defects, narrow slit-shaped.
- A spray bottle for a cold test to enable you to determine if the pulp is alive.

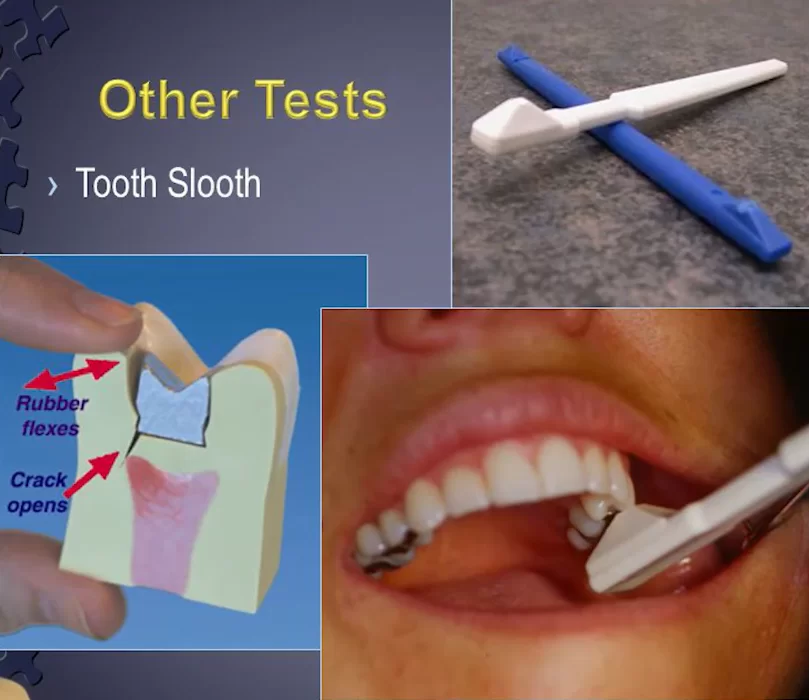
- A “Tooth Slooth” is a special plastic stick with a pyramid on top. Its shape is designed so that if you put the tip of the pyramid in the cusp of the tooth and ask the patient to bite the stick, it creates a lateral force as if to tear the tooth. If there is a crack, you can determine the cracked tooth syndrome quite accurately by the patient’s reaction.
Is it possible to save a tooth with significant bone damage in the apical region?
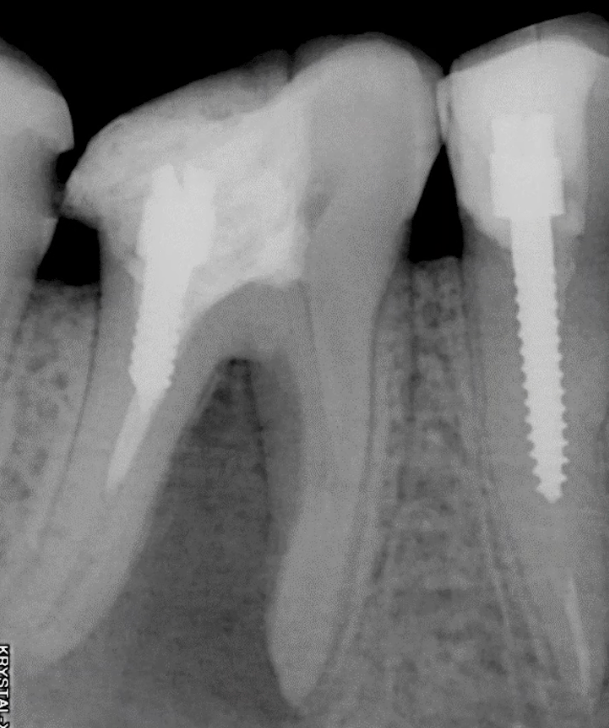
Very often a tooth extraction is indicated if there are extensive areas of bone thinning in the apical region, see example in the picture below. In fact, the size of the lesion is not decisive in the case of apical periodontitis.
If there is good access to the root canals, after instrumental (cleaning) and medication (disinfection) treatment, the bone tissue will fully recover and inflammation will go away. Of course, after treatment the root canals must be sealed and the tooth must be restored with a crown that covers the entire tooth.
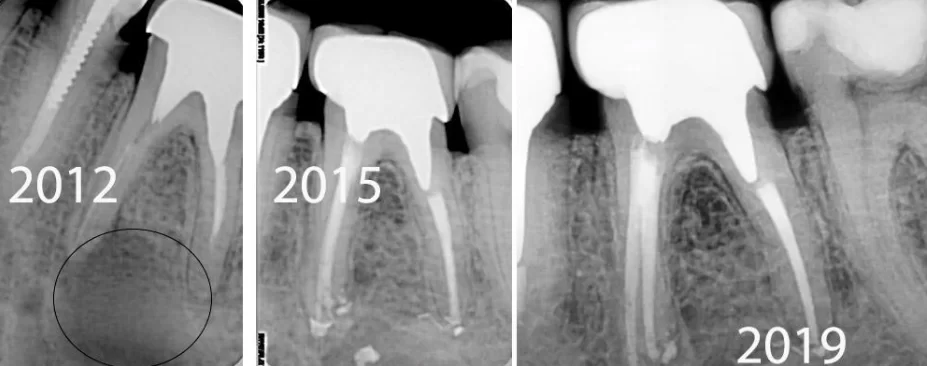
Let us look at a specific example from practice. The patient came in July 2010 with a significant intercorneal periodontitis lesion, and his image was used for the example above. This is a complicated case of symptomatic periodontitis, the patient complained of discomfort and painfulness when biting. Usually an intercorneal inflammation focus is a poor prognosis for a successful tooth restoration.
At one clinic, the patient was advised to have the tooth extracted, wait for the bone to recover, and have the implant placed. At another clinic, more experienced specialists decided to find out if the tooth could be saved. They started with diagnostics for the presence of fissures. This procedure should also be used when there are extensive unsuccessful restorations, or if there are large carious cavities.
You can find out if there are cracks without removing the restoration in the form of an express test. To do this, you will need the “Tooth Slooth” tool that we have already mentioned. It’s very easy to get it, you can buy it, or you can find an STL file on the Internet and print it on a 3D printer in any quantity.
The “Tooth Slooth” tool has two kinds of tips; one is a pointed pyramid, the other as a pyramid with a small depression on top.
The pointed version is placed in the fissure of the tooth with the apex if it is preserved (a depression on the occlusal surface of the tooth). Then we ask the patient to bite the “Tooth Slooth” stick. If it is painful, it means there is a crack.
However, much more common is the “Tooth Slooth” with a recess at the top of the pyramid. The recess is placed on the tops of the cusps of the tooth after which the patient bites down on the stick. Even if the patient did not feel any symptoms before visiting the dentist, but there was a crack, the patient will feel soreness with this placement and loading whereas a completely healthy tooth will not give any reaction.
Of course, the most reliable way to detect a crack is to expand the restoration, or remove the decayed tissue and physically see the crack. However, the second most accurate method is diagnostics with “Tooth Slooth” in spite of the simplicity and even primitiveness of the tool.
From practical experience, it is known that cracks are most often found on the lower teeth, usually lingual-medial cusps, but often distal cusps are also painful when tested.
The diagnosis was performed, but no cracks were found. This is very good; it means that the probability of successful treatment increases dramatically.
The next step in the diagnosis is to test with a periodontal probe. This is a very simple procedure that does not require anesthesia. It can be used to check for narrow slit-like periodontal defects. The probe technique is well known in all periodontal books and is taught in all educational institutions.
The probe is dipped into the sulcus without excessive pressure and examined first from the distal to the medial edge on both sides of the tooth. If narrow periodontal defects are not detected, the chances of preservation and successful treatment of the tooth are further increased.
Back to our patient, the following procedures were performed on the first visit:
- The old restoration was removed;
- A cariesectomy was performed; and
- The root canals were washed and cleaned.
The canals were temporarily filled with calcium-containing paste.
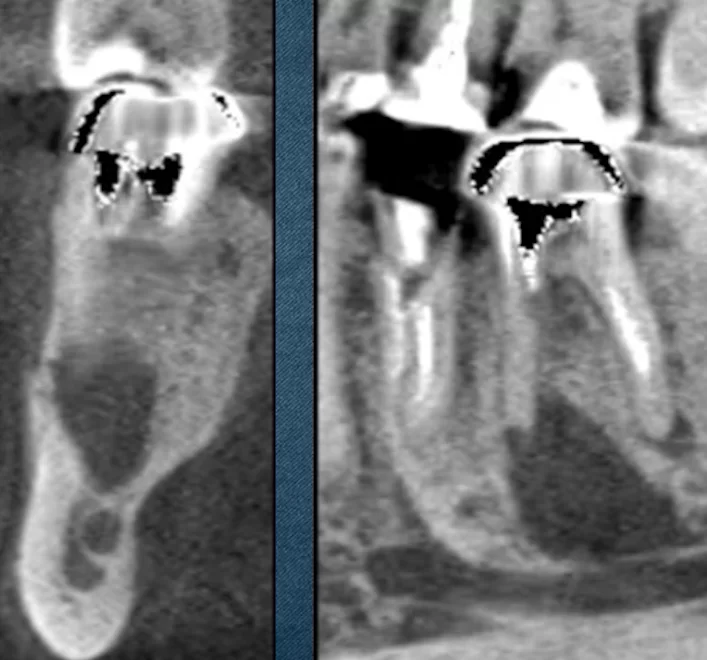
The following picture was obtained as a result of filling the canals with calcium-containing paste. The radiograph shows that the root of the tooth has a root canal with an exit to the intercorneal space.
The presence of such a canal explains how the infection could enter the intercorneal space and develop such an extensive lesion area.
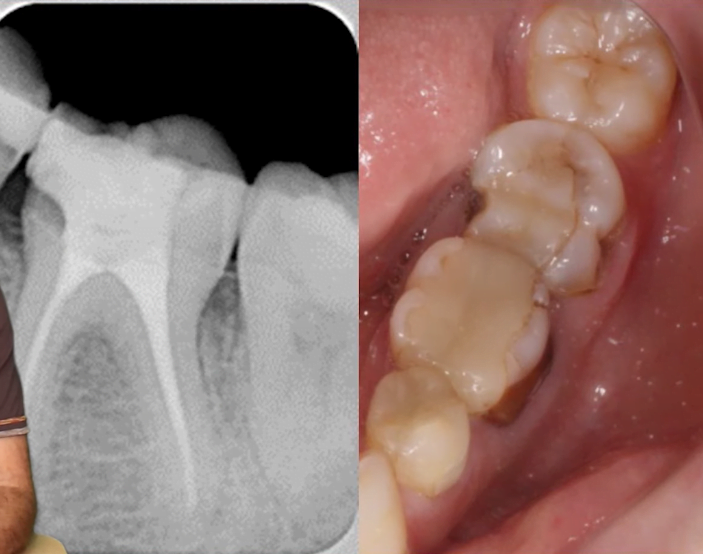
In August 2010, the root canals were filled with permanent filler; the tooth was restored with amalgam and prepared for a full crown. In September 2010 a temporary crown was placed, see left image.
The patient came back five years later. The tooth is restored, there is no discomfort. Since everything is fine, so why go to the dentist? This often happens.
However, it gives you an opportunity to see the changes that occurred during that time. As you can see from the right picture, the bone tissue is completely restored, and there is no trace of the extensive inflammation. At the same time, the wear of the temporary crown was visible, which was the reason for the return.
In 2015, a permanent crown was fabricated, and as you can see from the control image from 2018, the restoration looks fine.
This means that such teeth can be restored regardless of the size of the apical periodontitis lesion. The most important thing is that there are no cracks in the tooth.
It is also important to use a full crown when treating this kind of tooth. The endo-restorative protocol, which has become dominant in the treatment of such cases, also speaks to this.
According to this protocol, the treatment was not completed until 2015. Yes, the root canals were cleaned and sealed, but that’s only the endodontic part and half of the successful treatment. Until the tooth is fully restored, the treatment cannot be considered successful. Only by performing a full crown restoration can long-lasting results be achieved. Here’s what our patient’s restoration looks like 10 years after the first treatment in 2010.
The importance of the quality of the restoration is confirmed by a 1991 study by Dr. Vire’s group.
The study found that the most common causes of tooth loss were:
- 59.7% – unsatisfactory quality of restorations;
- 32% – periodontal problems;
- 8.6% – failed endotreatment.
Almost 60% of losses are due to poor restorations, which negates even very successful endodontic treatment. Endodontic treatment should almost always end with a complete crown, albeit a temporary one made of plastic, but always completely covering the entire tooth.
A temporary crown is useful when there is not 100% certainty that the endodontic treatment will be successful. It is possible to place a temporary crown, monitor the patient for 6-8 months and if all is well, make the restoration with a permanent crown.
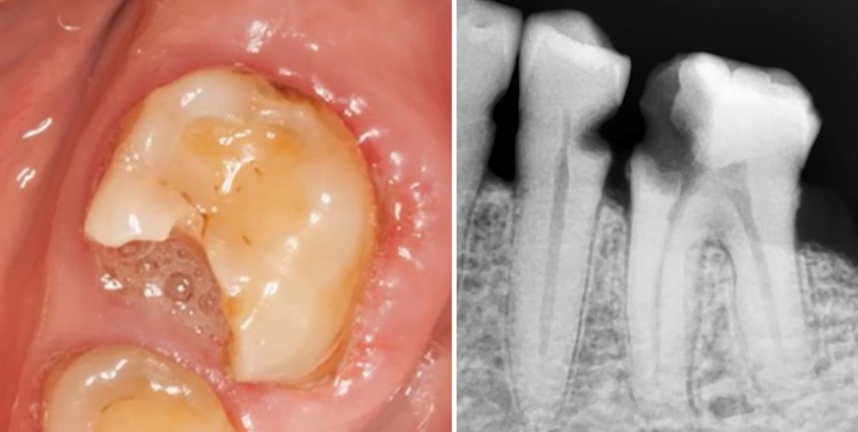
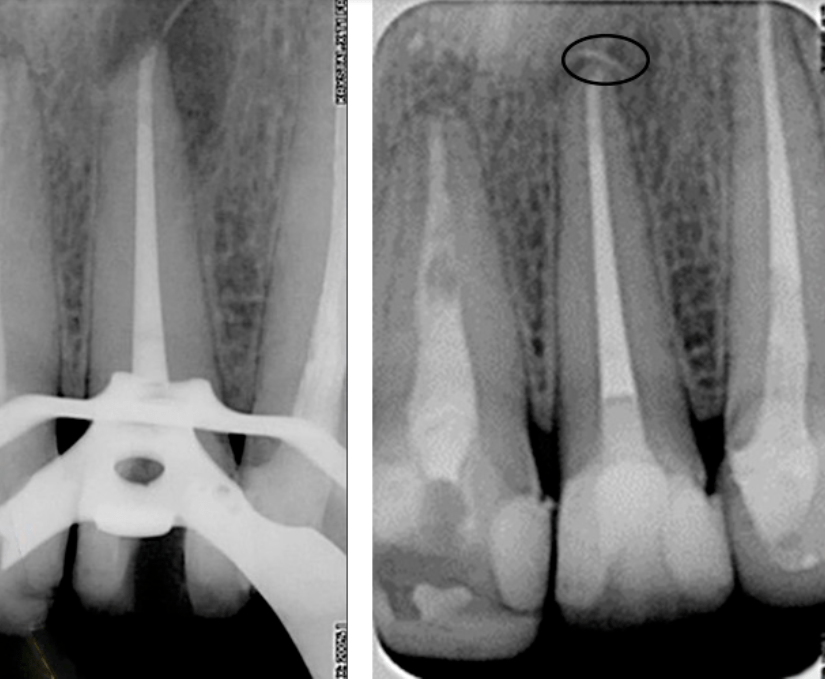
What can be considered an unsatisfactory restoration? One example is in the picture below. You can see a giant patch on two teeth at once with rough seams and gaps.
It is also a bad option to put a post in the root of the tooth and put a giant filling on it. Just such a restoration was removed from a patient whose case we reviewed.
Poor restorations distribute the load unevenly and could provoke cracking, and consequently tooth loss, despite the best efforts.
Here are the findings of another study from 2002 comparing the survival rates of endodontically treated teeth with full crown restorations and other techniques.
Endodontically treated teeth without crowns were removed six times more often than teeth with crowns. This is confirmed by actual clinical practice. This does not mean that crowns are indicated in every case. However, in the case of extensive carious processes, both primary and arisen under restorations, we have to deal with extensive cavities. Which only get bigger after a necroectomy. If the tooth is not covered with a crown, the likelihood of fractures increases.
Therefore, when making a treatment plan it is important to understand that if the tooth has been severely affected, it is imperative to complete the restoration with a crown after endodontic treatment.
Let us add another clinical case of asymptomatic periodontitis. The patient had no complaints, but the examination revealed a significant lesion area in 2012.
Since the tooth was already crowned, it was not possible to perform selective load testing. It remained to check the tooth with a periodontal probe for cracks. The result was negative and no defects were found.
The further treatment plan was simple:
- Removal of the crown;
- Cleaning and treatment of the root canals;
- Filling the root canals; and
- Placement of a temporary crown and observation, followed by a permanent crown.
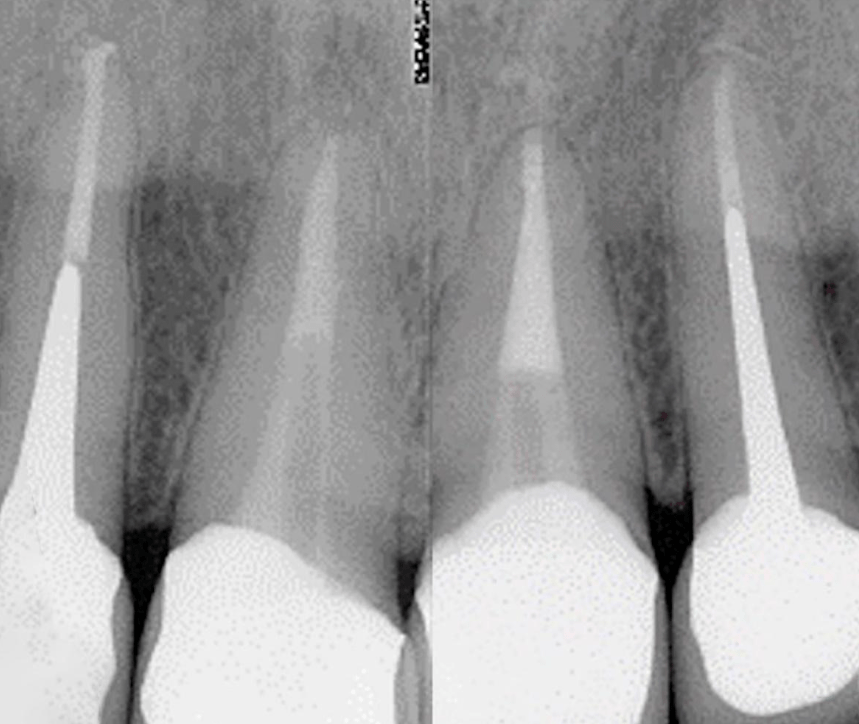
You can see the results in the pictures below. Immediately after the treatment in 2012, there is a significant area of bone damage (highlighted in the image). Three years later in 2015, we see complete healing of the bone tissue.
The control image from 2019 shows that there are still no problems. However, it is noticeable that the crown is not very close to the edge of the tooth, but nevertheless this case can be called a complete success.
Fistulas and periapical foci of inflammation are not necessarily indications for removal
In addition to extensive bone defects, there is another clinical symptom of an inflammatory process. Namely, the spread of inflammation to the soft tissues in the form of a fistula, which often misleads even experienced specialists into believing that the tooth must be extracted.
In fact, a fistula is not so scary, and such a symptom even provides some advantages.
First, it is diagnostic. You can always insert a gutta-percha pin into the fistula (it is almost painless) and trace the sinus tract. This way you can find out where the tract leads and where the infection comes from.
Secondly, a fistula is an excellent indicator of the success of treatment. If in the first visit the canals are cleaned and sealed, for example, with a calcium-containing product and a temporary filling is placed. If the fistula disappears after a few days, it means that the treatment was successful and the infection has been defeated.
In addition, if something went wrong in the endodontic treatment, there will be no complications in the endodontic treatment if there is a fistula.
To confirm this, let’s look at another clinical case where the only diagnostic tool was a gutta-percha post. It was placed in the sinus tract, and the X-ray showed that the source of infection was the apical delta.
The treatment was done. The root canals were filled and the problem tooth and the surrounding area were treated and restored. The next picture, namely the right side, shows almost complete healing of the bone tissue.
It is noteworthy that during the extraction of the pin, a small mishap occurred, namely, the tip of the pin broke off. It was pushed behind the apical space. The second image clearly shows that the bone dislodged and pressed this fragment to the apical space during the recovery process.
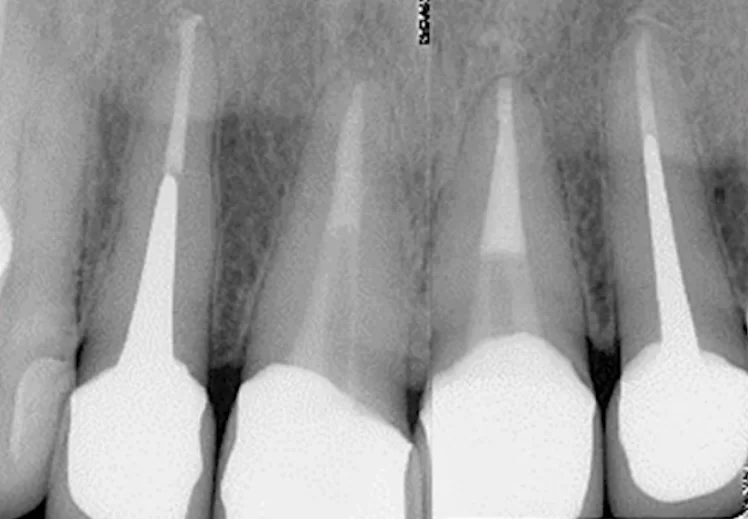
Nevertheless, you can clearly see that the healing was successful. The teeth were then restored, and at the control examination we see the following picture.
All of the inflammation has completely healed and the restoration looks great on x-rays and normal images.
The first part of our article is coming to an end, so let’s summarize the intermediate results:
- The presence of an inflammatory focus and even its extensive size cannot be a definite indication for extraction.
- It is not necessary to use expensive equipment to diagnose and determine the restorative potential of a tooth.
- The presence of a fistula is not necessarily an indication for extraction. On the contrary, in some cases it can even aid in diagnosis and serve as an indicator of successful treatment.
The second part of this article will focus on fissures, and the possibility of preserving a tooth despite the presence of a fissure.