Guided bone regeneration (GBR). Membrane
With this article we start a series of articles about the procedure of directed bone regeneration and the materials that are used for it. We will discuss both the materials that were used in the past and how they have changed now. This is an important issue, because quite a few patients have a bone deficit that makes placing an implant impossible.
In the past, the solution was to use a removable prosthesis that was fixed to the gingiva, but today the necessary amount of bone tissue can be augmented.
In this part we will look in detail at the different types of membranes that are used to build up bone volume. Let’s understand how directional bone regeneration started.
Directional bone regeneration at the right point came about thanks to periodontists. In particular, the scientist and periodontist Dr. Nyman conducted research on bone healing in parodontal recess.
And he came up with the idea that we need to somehow protect the bone tissue cavities from the ingrowth of soft tissue (epithelium). After all, the growth of bone tissue is incommensurably slower compared to soft tissue. Therefore, healing follows the simplest scenario: soft tissue covers the bone tissue and the bone tissue does not regenerate.
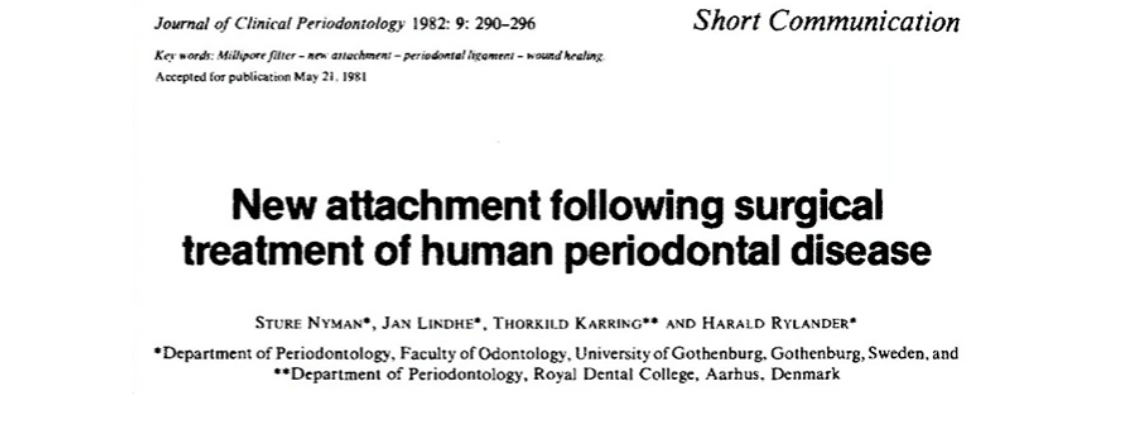
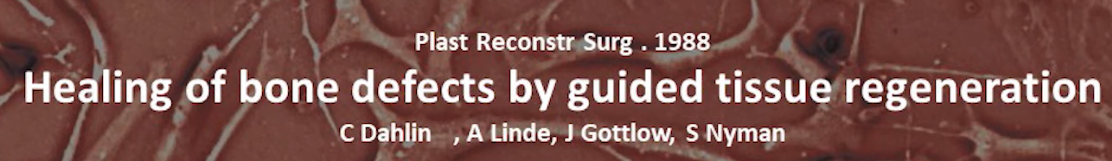
Dr. Nyman’s idea was that if you physically block the contact between the soft tissue and the bone, the cavity that is formed will be filled with bone tissue. Below you see a clinical picture of one of Dr. Nyman’s patients. Although the pictures are old, you can clearly see the incisors of the lower jaw with the defect, namely a periodontal canal 9 mm deep. And in the clinical photo you can see that in addition to the generalized bone loss, there is also a bone pocket between the 32nd and 33rd tooth.
Of course you can take the flap off and do a scaling (alignment) of the root surface. Polish everything, remove any deposits, then put the flap back in and suture. As a result, we get a new periodontal attachment. But the bone defect between the teeth will not go anywhere and soft tissue ingrowth will occur again and the bone defect will remain.
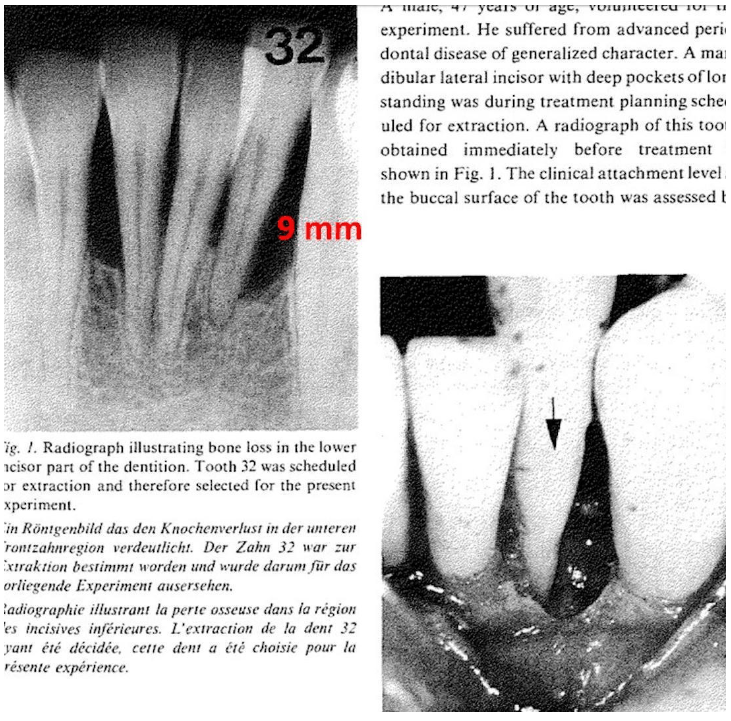
And then, and it was the 1980s of the 20th century, Dr. Nyman decided to use as a barrier a simple chemical filter from Millipore brand, which are still used in chemical and biological laboratories.
This is a cellulose filter that allows liquids containing proteins, enzymes, etc. to pass through, but with pores small enough to keep epithelial cells from sprouting.
In the illustration below, you can see a schematic of the surgery where Dr. Nyman got a brilliant result.
He experimentally proved that defects are covered by a barrier, which does not allow soft tissues to attach to the bone, the body successfully eliminated. The defect heals – bone tissue builds up in the cavity that the barrier forms.
In this experiment, he obtained almost 5 mm of bone growth. Dr. Nyman’s results have been the beginning of many scientists around the world. Here is one of the most iconic.
And just 6-7 years later, the first specialized Teflon (polytetrafluoroethylene foam) membranes appeared on the market, see the illustration below.
One of the most interesting properties of PTFE from the medical point of view is its complete biological and chemical inertness. It is not soluble in alkalis or acids, in this respect it surpasses even the noble metals. In addition, it has very poor adhesion (nothing sticks to it), and very high hydrophobicity and oleophobicity. That is, neither liquids, nor oils and fats stay on its surface, much less can soak it.
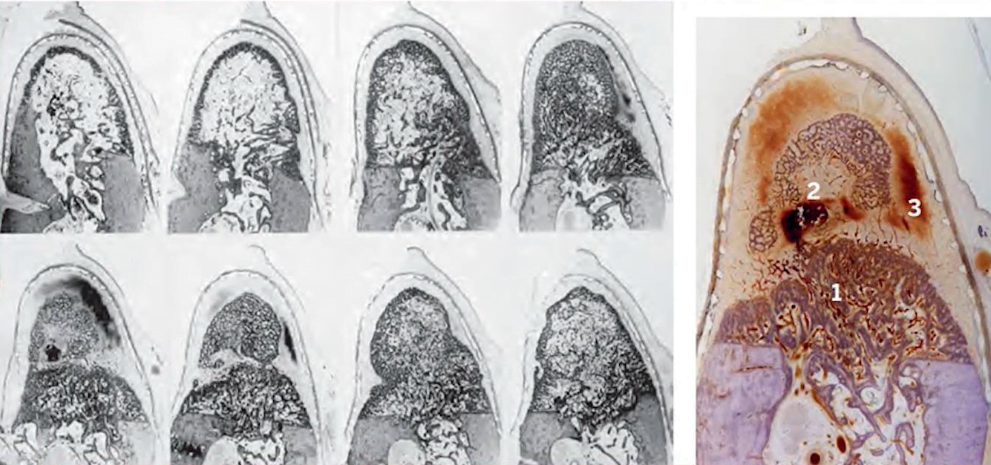
Some time later, Dr. Dahlin and colleagues conducted a series of extended experiments on primates.
During the experiments, they created artificial defects and compared the healing results with the use of membranes with the control group where the defects healed naturally.
After healing, histology was performed, which revealed that the defects closed by the membrane healed almost completely. And in this study the cavities closed with membranes were not filled with anything. They were filled with a biological clot, which naturally formed new bone tissue.
And already in 1994 the program study of the Bern group under the direction of Dr. Schenk was published, which was later used as a reference point by many specialists.
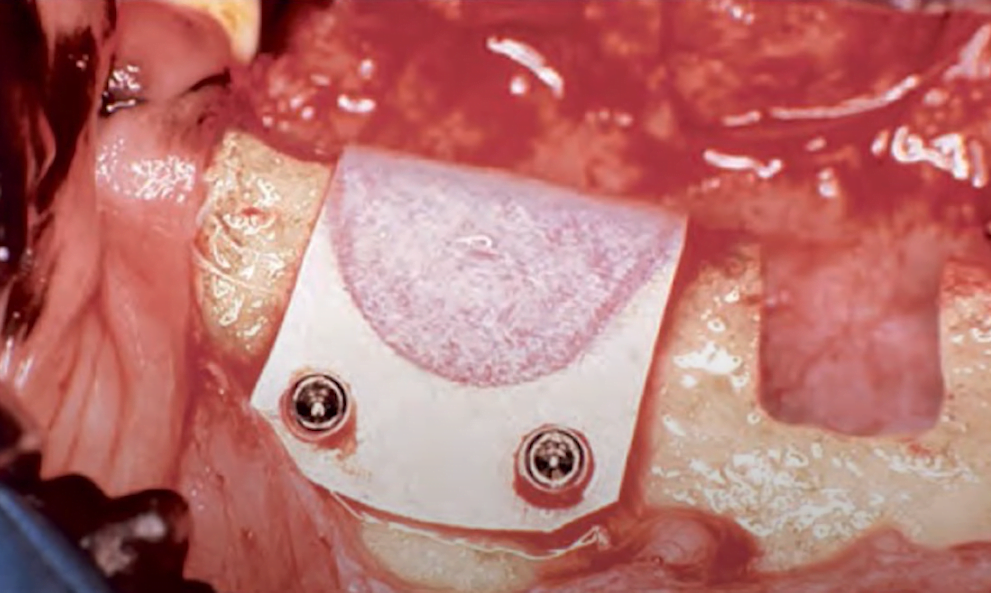
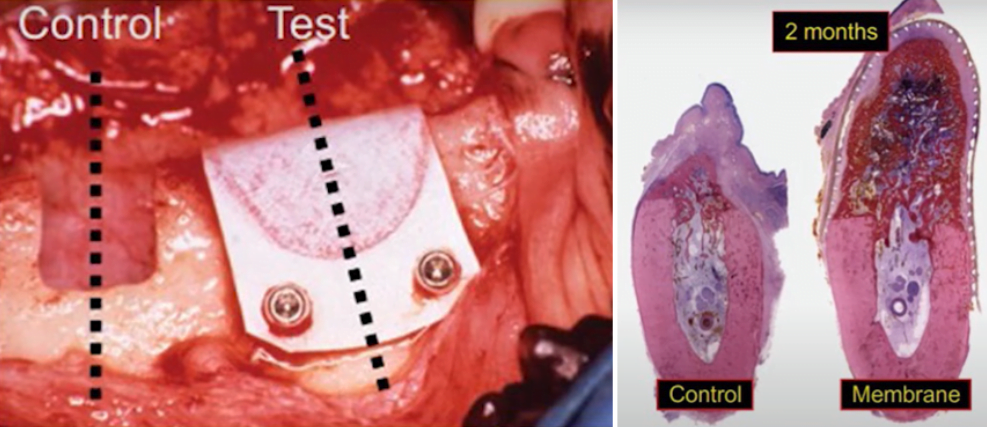
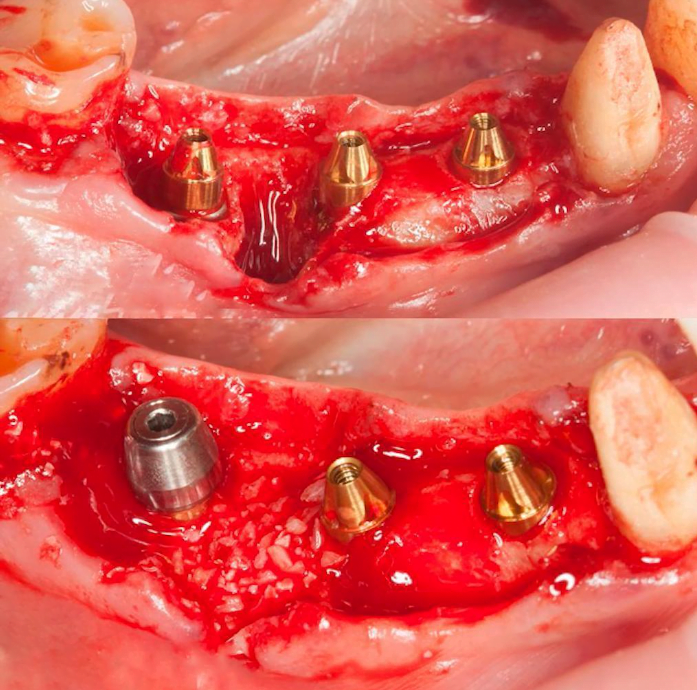
The study was performed on dogs using Teflon foam membranes. The artificial saddle-shaped defects in the alveolar ridge can be seen in the photo. The test control technique was used here as well. In the control group, the defects were not covered with anything.
In this study, membrane-covered defects were also not filled with anything, and bone tissue was formed from a clot saturated with proteins and enzymes, which is formed naturally.
The results were impressive such huge defects healed almost completely. And this study broadened the understanding of bone growth and regeneration.
Professor Schenck, being a morphologist and histologist, made a huge number of histological preparations. The main thing the researchers found out was that the key factor in bone healing is the barrier between the bone and the soft tissue, which very quickly grows into the defect.
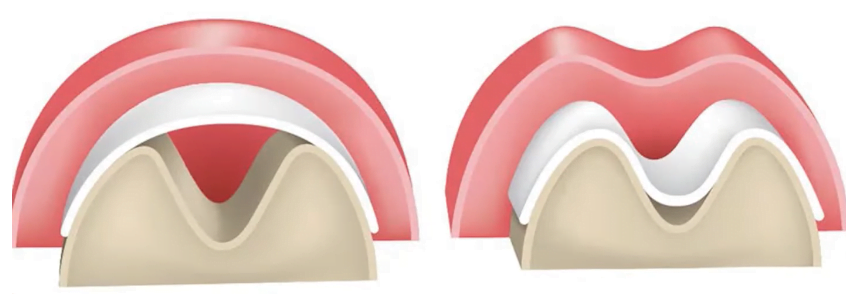
Note the following illustration, which shows that in the control case, there was no restoration of bone ridge height. The entire volume was filled with soft tissue, there was recession and reduction of the ridge in the area of the defect. And in the place where the membrane was, there was complete healing with complete restoration of the alveolar ridge height.
The time when these studies were conducted coincided with the active development of dental implantology. By the 1990s, Branemark-type root canal implants had become the standard and dentists were increasingly faced with a lack of bone for implants.
And there was a need for technology that would help restore bone volume in both the width and height of the alveolar ridge. The research and practical application of barrier membranes continued and by the beginning of the XXI century the procedures for targeted bone regeneration became common and even routine.
In 2009 an article was published in which the NCD technique was named as one of the most reliable with predictable results along with sinus elevator.

Modernity of the results and achievements of the GBR
Already in the twenties of the XXI century Dr. Boozer’s book – 30 Years of Directed Bone Regeneration – was published. In the book Professor Boozer as a direct participant of all stages of formation of the technology described all the way from the beginning to the present day.
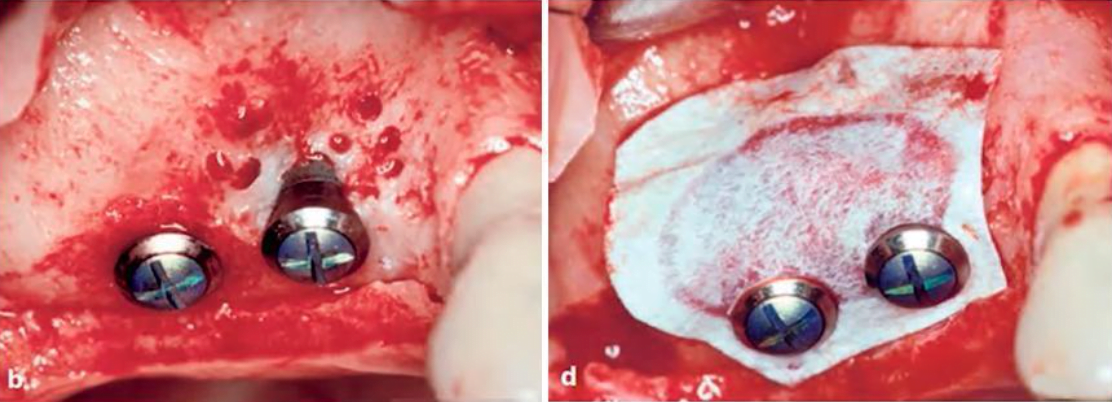
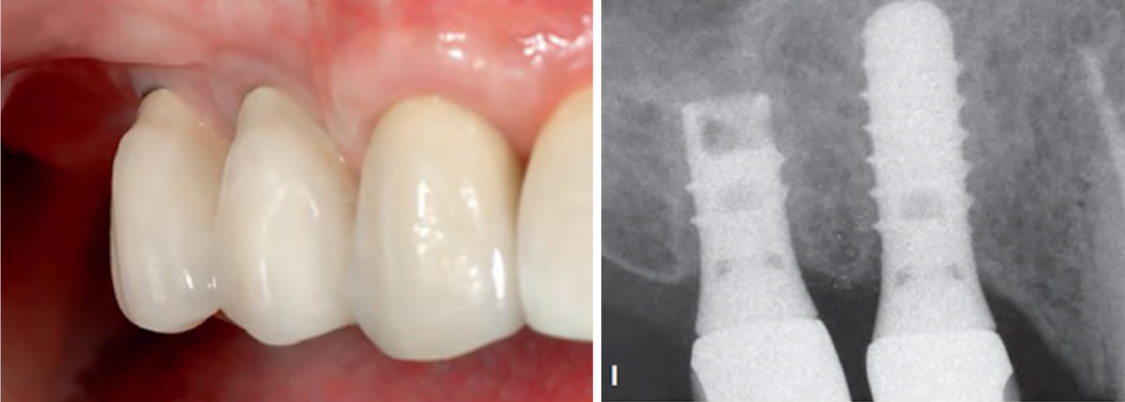
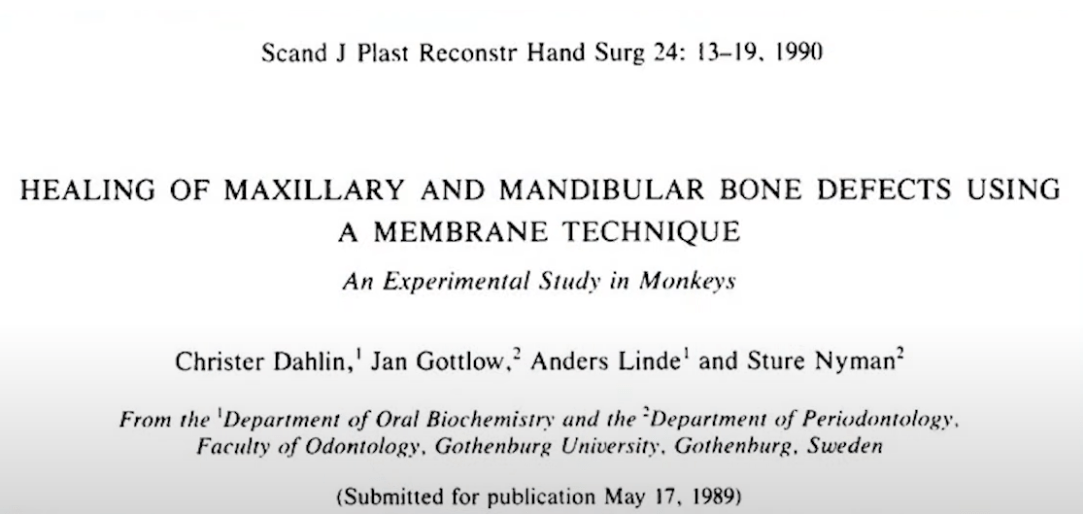
In the book, Professor Boozer describes, among other things, his own clinical cases. Here is a photo of one of them.
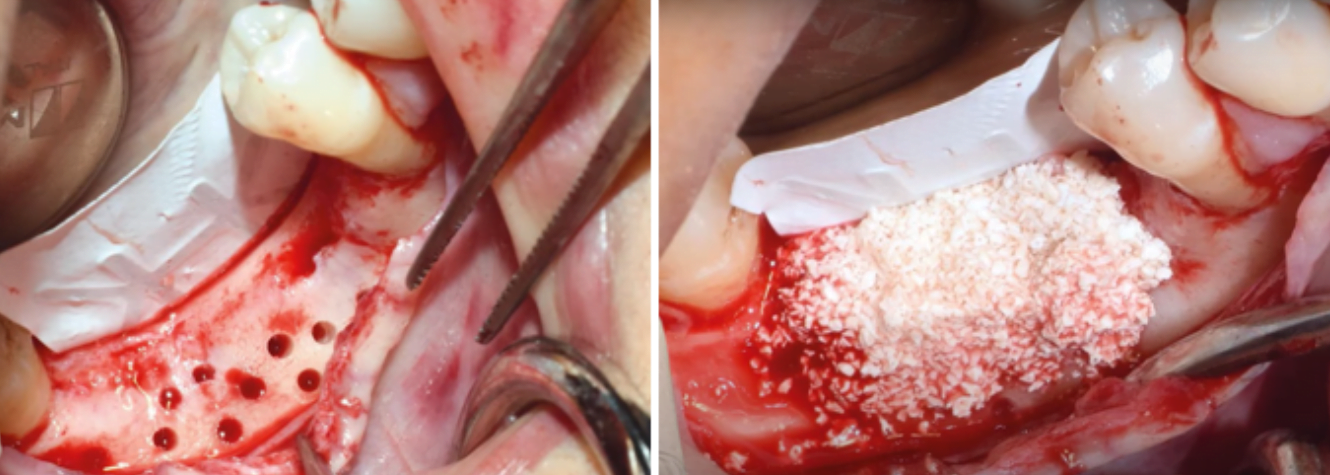
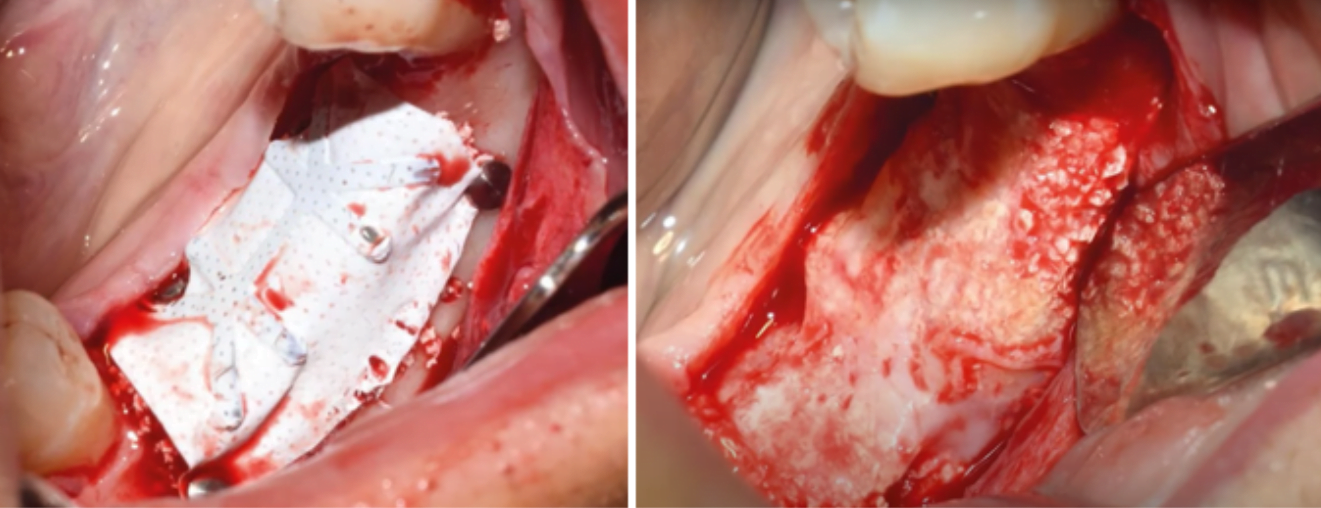
Photo of implants and pronounced bone deficit on the vestibular side (left) and bone chip covered with GoreTex membrane (right)
The patient had a frequently encountered bone defect on the vestibular side, which was repaired with a GoreTex Teflon membrane. Bone chips were used as a filler and the flap was sutured. After the healing process was completed and the membrane was removed, significant bone growth was clearly visible in the following images.
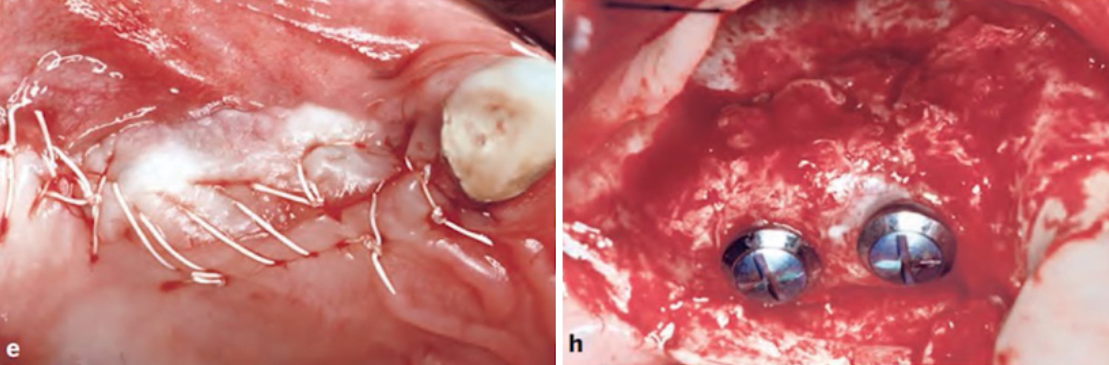
Pictures at different stages on the left sutured flap immediately after placing the membrane, on the right the opened flap where you can see a significant increase in bone tissue.
But the most interesting thing is the pictures of the same patient 25 years after the placement of implants. Nowadays it is already possible to do a CT scan and all the pictures show the excellent condition of both the bone tissue and the prosthesis.
The key principle – directed bone regeneration
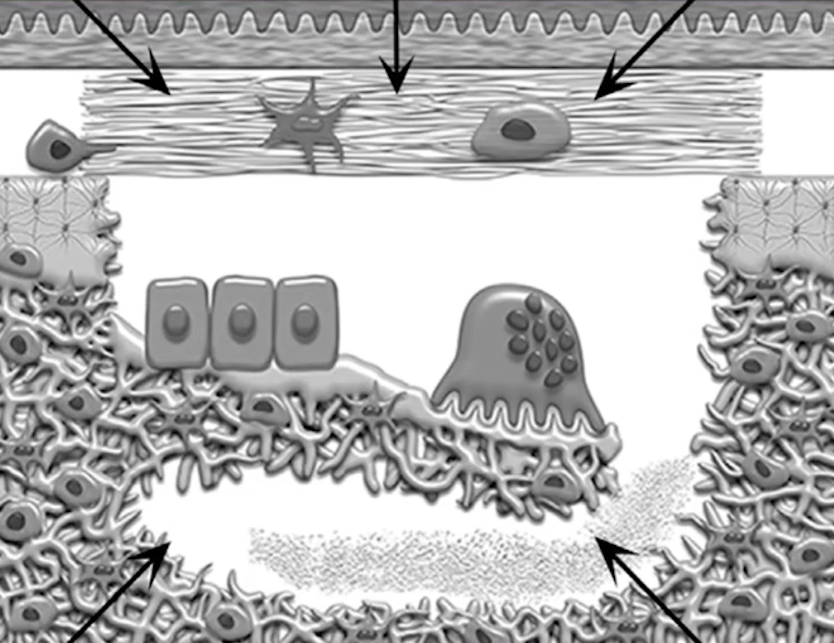
Actually, it’s very simple – the main condition for healing a bone defect or increasing bone volume is to block the contact between the epithelial cells and other neosteogenic cells and bone tissue in the site of the defect.
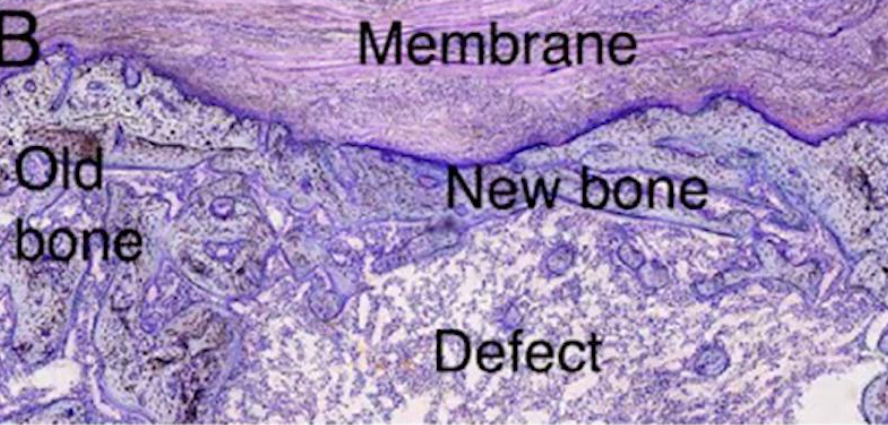
In the illustration below, you see a test where you can see on the top slide that new bone tissue has formed between the old bone and the membrane. And the same defect not closed by the membrane is simply overgrown with soft tissue and has not recovered at the level of bone tissue in any way.

Histological section where you can see that in the case of the barrier membrane, the bone regenerated, and in the control case the bone defect remained
The soft tissues of the oral cavity have an enormous regenerative potential, and in case of any injuries the body tries to close the wound as quickly as possible. And when the doctor closes a bone defect with a flap, it starts to grow into the bone tissue in the first hours.
First they are fibroblasts and then epithelial cells. Whereas bone tissue grows quite slowly. In such a situation, rapid growth and healing of soft tissue blocks the growth and restoration of bone tissue. In the case of installation of the barrier membrane, soft tissues fuse on the surface of the membrane, and the conditions for new bone tissue formation are created between the membrane and the bone base.
In this way, defects (cavities and depressions) that occurred between the teeth can be healed or the height and thickness of the alveolar ridge can be increased.
What requirements modern GBR membranes must meet
Around the same time that Dr. Boozer’s patient received treatment, namely in 1994, a consensus conference was held in Arizona. Below you see the famous photo of key experts in the field of guided bone regeneration, who were the initiators of this conference.
The specialists discussed the current state of this field and the future prospects for its application. And it was unequivocally accepted that guided bone regeneration is definitely a promising direction. It was confirmed that the bone tissue grows perfectly well if a barrier of a membrane is created. But the disadvantages of the ePTFE membrane technique were also noted:
- A significant number of complications in the form of exposed membranes. Especially in the early stages, leading to loss of the graft and having to start all over again.
- Difficulties in manipulating the membranes due to their hydrophobicity, hardness and the need to fix the edges of the membranes with screws to the bone. This is an intractable problem due to the physical properties of Teflon.
- The need for repeated surgery to remove the membranes.
The key conclusion is that the technology is promising and we need to look for ways to avoid the disadvantages that doctors and scientists had encountered by that point.
And just in the mid-90s the first collagen membranes appeared, which did not need to be removed and which were completely resorbed by the body. They were used in the same way as the previous generation. Namely, they created a barrier impermeable to epithelial cells and allowed the formation of bone tissue in a certain place.
The joint use of collagen and Teflon membranes made it possible to develop requirements for modern barrier membranes, which are still relevant today:
- Biocompatibility. There should be no complications due to the contact of living tissues with the membrane material.
- Cellular Occlusion. Impermeability to epithelial cells.
- Ability to hold volume for bone growth. Especially relevant when alveolar ridge height needs to be increased. The barrier membrane must be rigid enough to hold the bone graft in a certain shape.
- Integration with surrounding tissues.
- Biodegradability – complete recycling by the body without the need for repeated surgery to remove the barrier membrane.
- Susceptibility (resistance) to complications.
Varieties of membranes that are used for targeted bone regeneration operations
Let’s start the review with those variants of barrier membranes that appeared earlier.
- Polytetrafluoroethylene. Let us remind you of the advantages of this material:
- Bioinertness – it also does not dissolve in alkalis or acids;
- Almost nothing sticks to it, which is important at the stage of removal of the barrier membrane;
- High strength and stability.
The series of illustrations below show the sequence in which the diaphragm for bone augmentation is installed. The pictures clearly show both the preparatory phase with bone graft placement and the fixation phase of the membrane. And the last photo shows the result after the removal of the membrane.
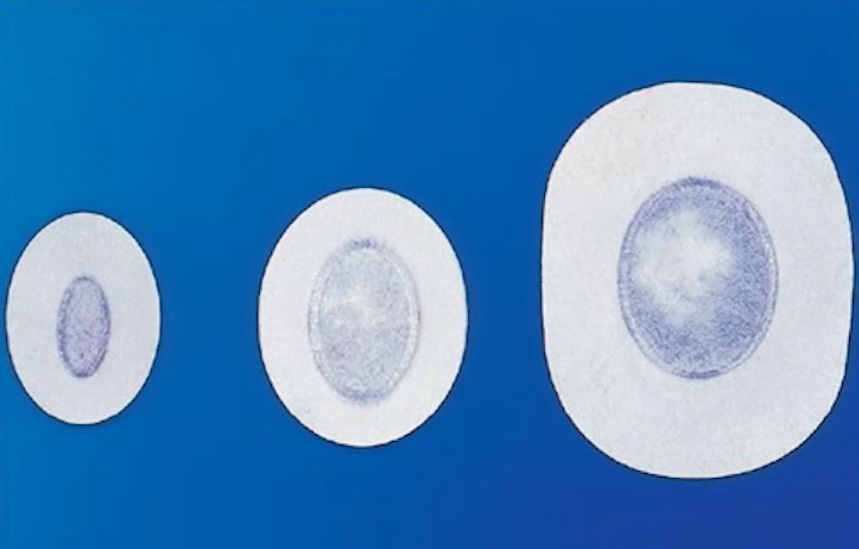
Let’s understand how polytetrafluoroethylene membranes changed. The configuration of the first membranes from GoreTex was rather complicated, see the illustration below. They were made in such a way that in the center the density of the material was smaller and the pore size was correspondingly larger.
And at the edges the membrane is denser, which gives more strength. After all, these are the areas that were used to mechanically anchor the membrane to the bone.
It was the central part that covered the bone defect and here you need a large permeability for fluids with proteins enzymes and other substances that should penetrate into the area of new bone formation.
For a long time this approach was the gold standard. But by today, the production of Teflon foam ePTFE membranes has been discontinued.
In modern medicine, membranes made of denser dPTFE are used. The difference is in the structure and pore size. The old samples had a pore size of 20-25 microns in the central part and about 8 microns in the densest part. The modern samples have a pore size of only 0.2 microns, which is much smaller.
The rejection of polytetrafluoroethylene foam was due to a frequent problem in which the soft tissues that covered it were not strong enough and often exposed the membrane. In fact, the soft tissues could not adhere to the Teflon. This happened both in the early and late stages of healing, see image below.
And when the membrane was exposed, where the pore size was 20-25 microns, it became permeable to bacteria that were smaller, and they penetrated into the area of bone formation. That caused an inflammation and the whole procedure had to be restarted. And sometimes with an even bigger bone defect, because the doctor had to remove the suppuration.
Therefore, modern PTFE membranes are impermeable not only to the epithelium’s own cells, but also to most pathogenic microorganisms. At the same time, proteins and enzymes dissolved in the intercellular space can still penetrate through the pores.
Thanks to the new membranes, the effects of exposure have been reduced. But exposure is still an extremely negative complication. And that was another reason to look for an alternative to PTFE membranes.
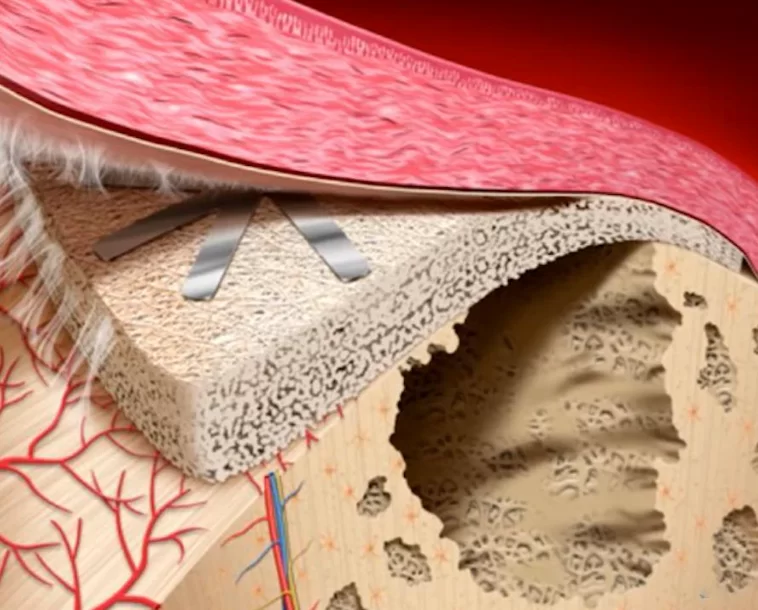
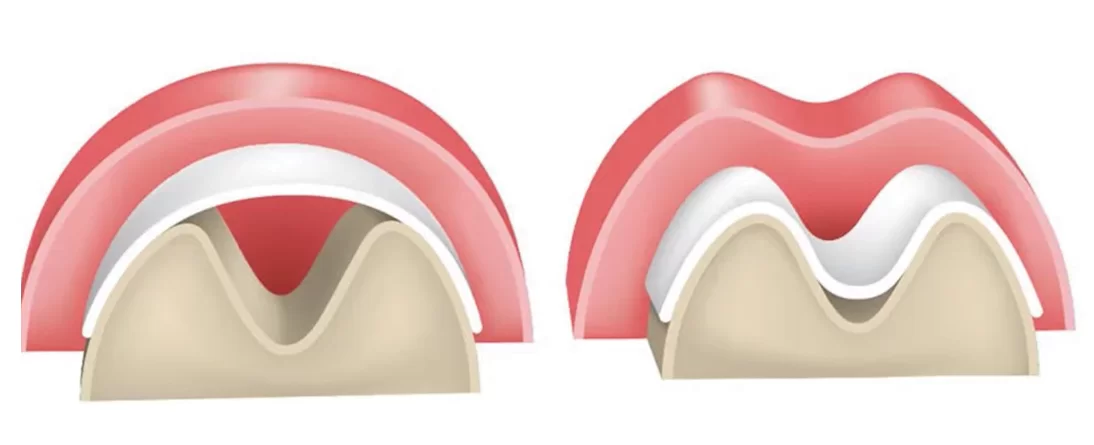
Another nuance is that, for all its strength, PTFE remains flexible, and it is difficult to form a direction for vertical bone growth with it. The membrane will simply be distorted by the movements of the food lump and the alveolar ridge will not be formed to the desired height and shape, see the illustration below.
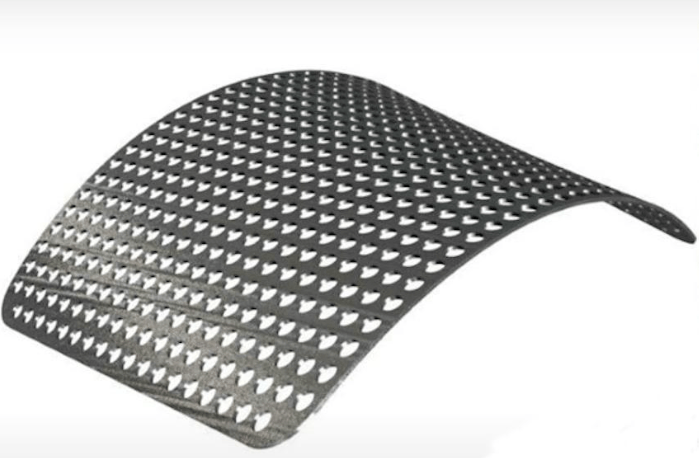
Immobility is important for proper bone growth. That is why barrier membrane versions reinforced with metal inserts began to be produced. Most often, titanium is used as reinforcing inserts. Such variants do allow the formation of a rigid framework over the regeneration site, see illustration below.
But it is not possible to solve the problem with the exposure of the Teflon membrane surface. It’s all about the absolute “non-stickiness” of this material. And if the soft tissue layer is too thin, such unpleasant complications often occur. In addition, the quality of bone tissue regeneration under the old type of membranes with large pores is still better. This is due to the fact that small pores make it difficult for fluids rich in proteins and growth factors to penetrate to the site of new bone formation.
If we go back to the requirements for modern barrier membranes, we see that PTFE membranes of both old and new types do not meet several of them at once:
- Integration with surrounding tissues – epithelium does not adhere to the membrane surface, which often results in complications.
- Biodegradability – Teflon is not accepted by the body, and after healing it is necessary to reoperate and remove the barrier membrane.
- Resistance to complications – unfortunately, there are quite a few complications with PTFE membranes.
This gave an impetus to the search for new materials, which we will describe next.
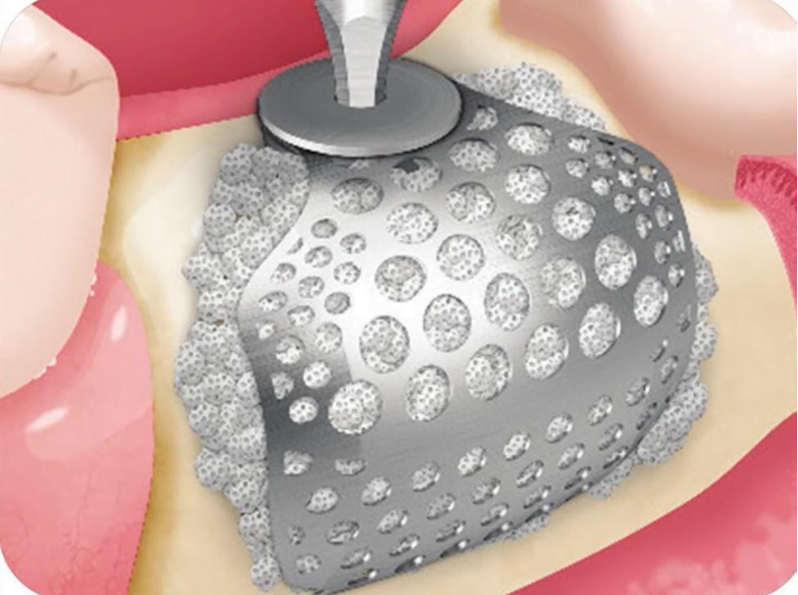
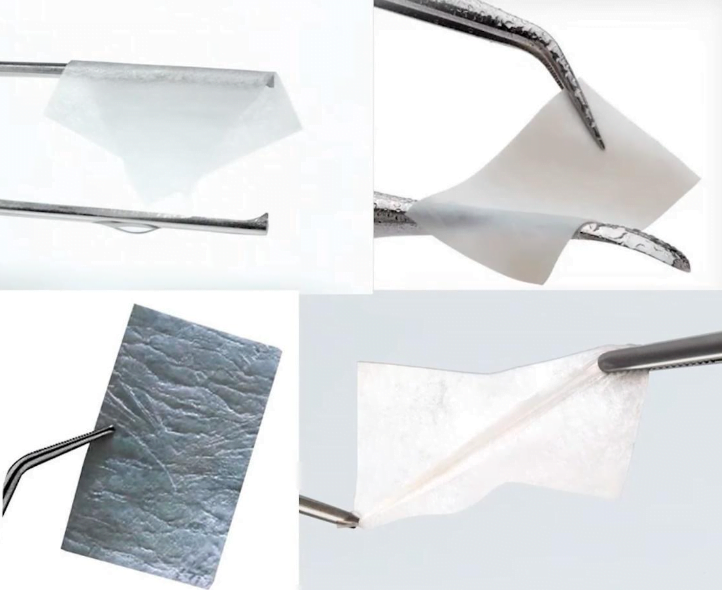
2. Titanium mesh membranes. The size of the holes here is quite large, about 1 mm, which is good for the free flow of fluids. But the question may arise whether the holes are too large to prevent sprouting of the epithelium. Nevertheless, in practice, good regeneration results are obtained. If the holes in the titanium are larger, additional collagen membranes with small pores are used together with them.
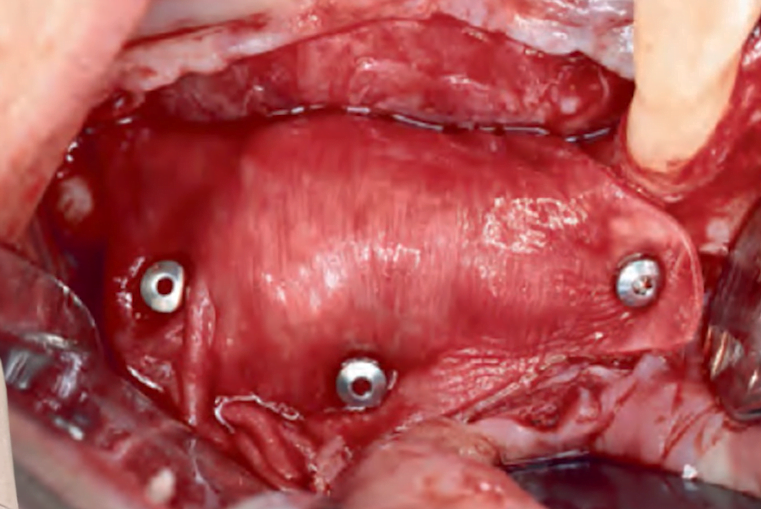
Based on titanium mesh membranes, special frameworks have emerged that immediately have the shape of the alveolar ridge to be augmented. And if a small section of bone tissue needs to be augmented, there are small bonebuilders that are fixed with a plug that is inserted into the implant.
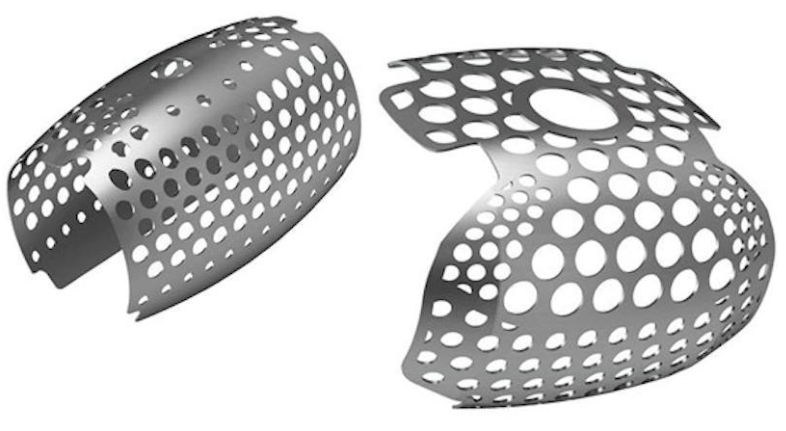
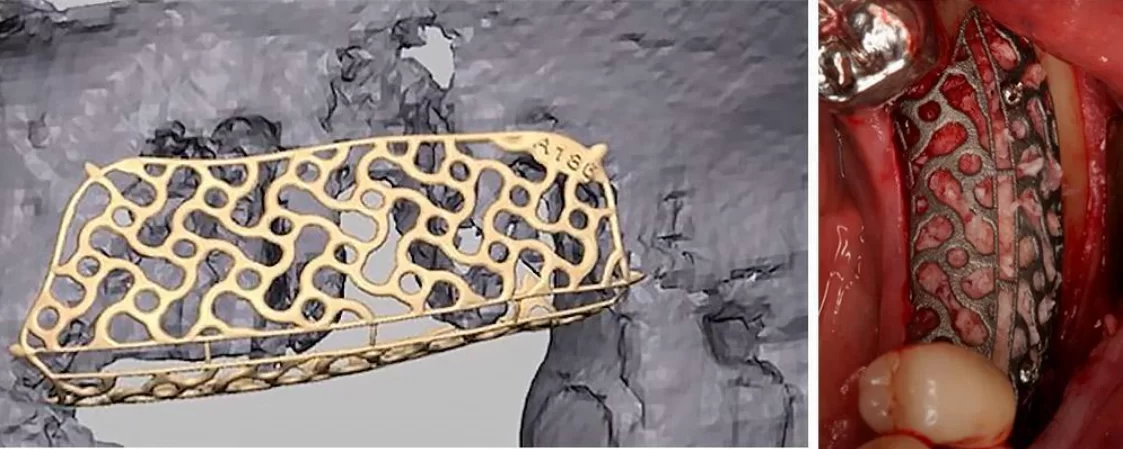
The pinnacle of the development of titanium structures for guided bone regeneration is the development of customized solutions, see illustrations below.
Titanium is biocompatible, neutral, and unlike Teflon is very strong, which allows to immobilize the bone graft completely. However, with titanium constructions the same complications can occur in the form of exposure of metal parts from under the soft tissues. There is also the problem of repeated surgery to remove the titanium framework.
3. Resorbable membranes. All of the previous options need to be removed, and they often cause complications. This means they fail on at least two key requirements for barrier membranes, viz:
- Biodegradability – Teflon and titanium membranes need to be removed.
- Resistant to complications – it is not uncommon for the membrane structure to be exposed from under soft tissue.
Biodegradable membranes can be divided into two large groups:
- Synthetic polymer-based.
- Based on collagen polymers derived from sources of biological origin: bovine tendons; bovine dermis; porcine dermis, human dermis.
To date, synthetic polymer membranes are not as good as we would like them to be, and the main advantage is the unlimited amount of raw materials for synthesis. But the search and development continues, perhaps soon barrier membranes based on synthetic polymers will surpass variants of biological origin. But unfortunately, now they have a serious disadvantage – inflammatory response from the body.
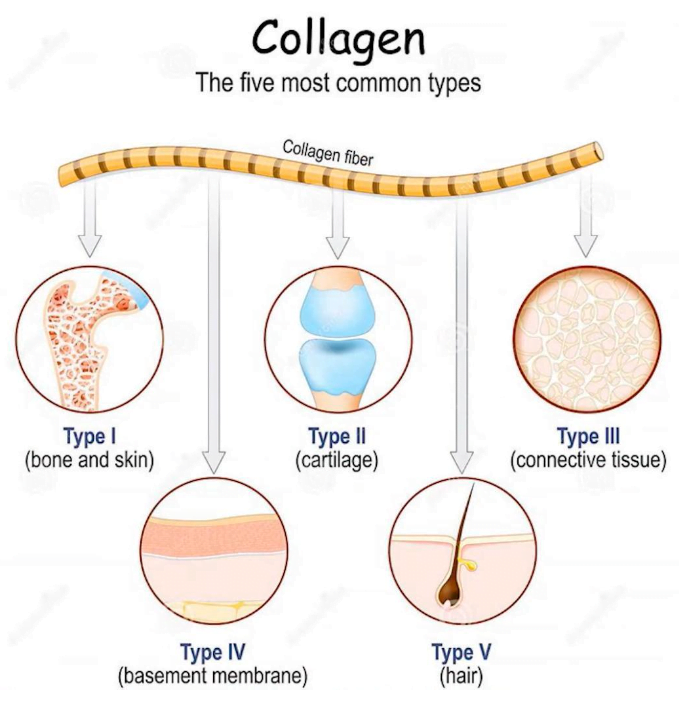
Collagen membranes derived from sources of biological origin do not cause such adverse reactions, so they are leading the way among resorbable barrier membranes. Collagen is the most abundant extracellular and matrix protein. It is involved in a multitude of processes. This includes epithelial attachment, healing processes, and cell differentiation, all of which involve collagen. It is present in almost all tissues, in some more in others less.
The source of collagen is not so important, because during the transformation process all foreign tissues are removed and the result is pure collagen fibers in a polarized form. The scheme of transformations is shown in the illustration below.
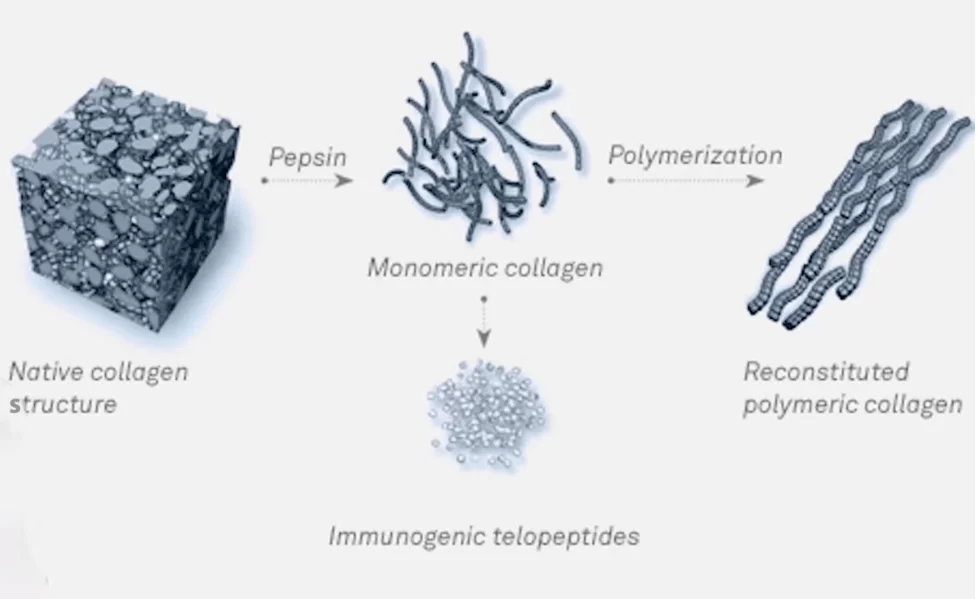
Barrier membranes with different properties can be created on the basis of collagens of biological origin. But what they all have in common is biodegradability. That is, they are completely recyclable and no extraction operations are needed.
Most collagen membranes decompose rather quickly, literally within 3-4 weeks. This is usually enough for reliable healing of the bone defect, because the primary bone callus is formed during the first four weeks. But the high rate of resorption can be a problem in some cases, which we will talk about next.
Also, most unstitched collagen membranes also have a common disadvantage with Teflon membranes. They are too soft and easily deformed, which leads to the same sagging problems if a large enough volume of bone needs to be augmented. It is especially difficult if the alveolar ridge height needs to be increased.
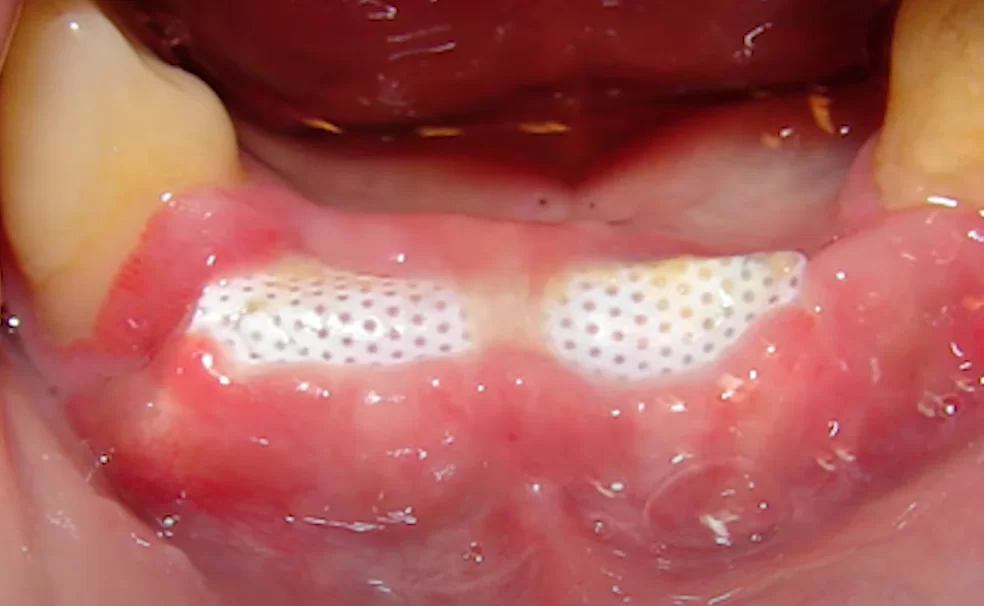
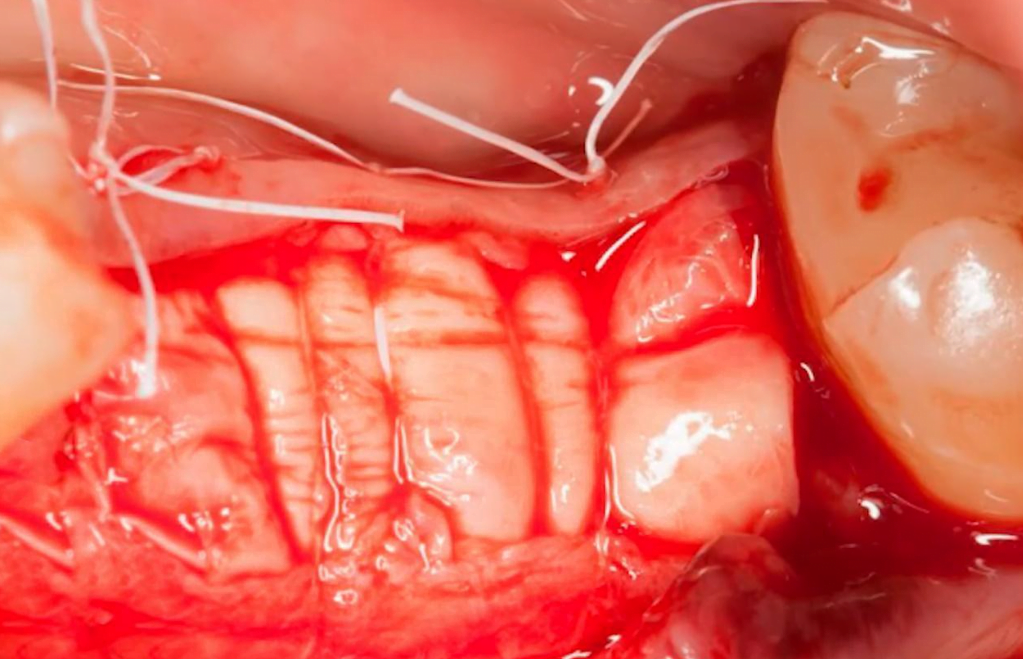
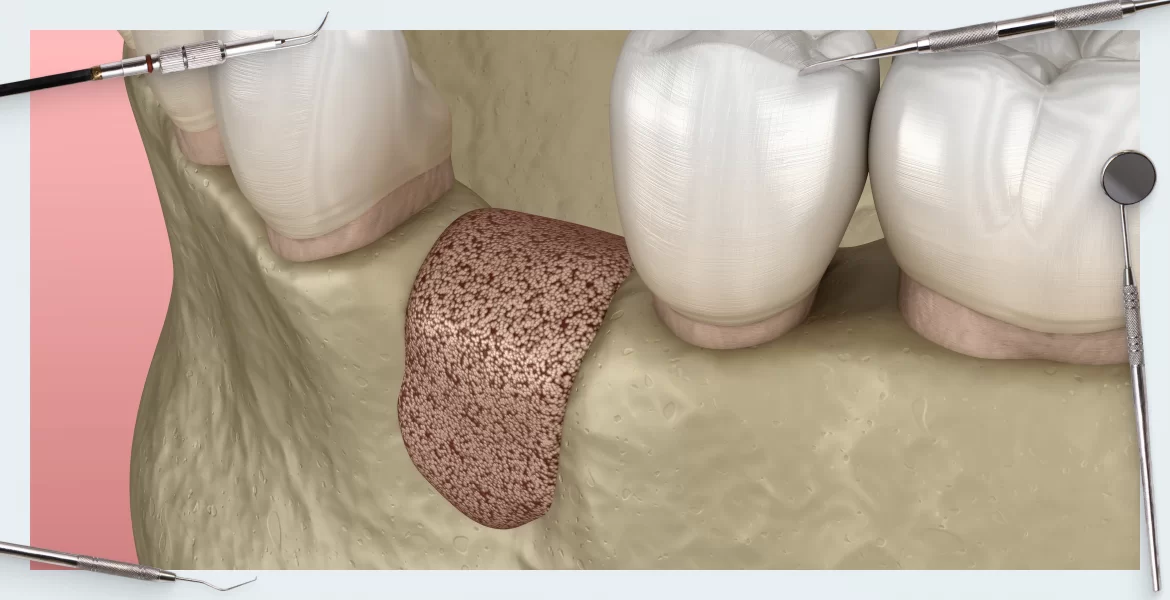
Now let’s talk about the varieties and properties of different types of membranes. As always, everything is determined by the area of application. For small defects, where you don’t even need to fix the membrane, as in the illustration below, the thinnest and most easily stretched membranes will do. In this case, it is not so important how quickly the barrier membrane dissolves.
The situation is quite different if a horizontal augmentation of a significant volume is to be performed. In such cases, the bone graft must be fixed very tightly and long enough for the primary bone callus to be fully formed by the time the membrane is resorbed. One of the options is shown in the photo below, where the membrane is stretched and pinned in place. And in this photo the surface of the stretched membrane looks something like a sausage, doctors sometimes call this method sausage.
Membranes that can cope with such challenges can be found under the brand Bio-Gide (double-layer uncrosslinked collagen membrane) or CreosTM. Not all membranes can withstand the necessary tension and can tear at the fixation sites.
Therefore, the appropriate type of membrane for each type of surgery must be chosen carefully. Most crosslinked collagen membranes can withstand a high mechanical load.
Let us understand the difference between crosslinked and non-crosslinked membranes. Non-crosslinked consists of chaotically interwoven collagen fibers and their structure resembles regular absorbent cotton. The structure of crosslinked barrier membranes looks more like tissue, as in the illustration below.

An ordered textile structure, which is similar to a cross-linked membrane structure, where collagen fibrils are interwoven in an orderly fashion and intertwined with each other
The price of cross-linked collagen membranes is much higher, but the strength is also several times higher. But be careful, cross-linked collagen membranes from different manufacturers have principally different properties. For example, the Mem-Lok membrane is very stiff and almost does not stretch or tear.
It needs to be cut to shape before being placed on the defect area, and it tolerates mechanical fixation well. Another example is the OSSIX PLUS membrane, also made of cross-linked collagen, but it is very soft and elastic and is only slightly stronger than the non-cross-linked collagen membrane. OcceoGuard membranes have intermediate properties, so a suitable solution can be found for each clinical case.
But the common feature of all crosslinked collagen barrier membranes is that they take a very long time to resorb. In practice, it has been repeatedly observed that the structure of the membrane was partially preserved even six months after installation. This is a huge advantage, because the bone tissue is formed much slower in older people, and they are more likely to become patients of dentists.
There are no perfect solutions – the choice depends not only on the individual case, but also on the methods and skills of each doctor. For example, some specialists prefer a technique with tension and fixation of the membrane to the bone tissue, as in the illustration above. For this purpose, a double-layered non-crosslinked collagen membrane such as Bio-Gide, Jason or CreosTM is well suited.
But there is another way to secure the membrane, which is suturing as shown in the picture below. A membrane like OSSIX is better suited for this. Yes, it takes a little longer to heal, but that’s not critical because it’s important to get a good end result. That is, a strong bone in sufficient volume to insert the implant with minimal re-surgery. And the second method gives the same result without the use of titanium screws.
The unexpected role of the barrier membrane in bone growth
It was long believed that the barrier membrane was only a barrier to keep epithelial cells out of the bone formation area. A relatively recent review article – Barrier membranes: More than the barrier effect?
In which a very different view of the role of barrier membranes, both collagen and Teflon membranes, is shown. The publication makes a strong case that the membrane itself is already an osteogenic factor.
This means that the presence of the membrane is already a stimulation of osteogenesis. Biodegradable collagen membranes work better in this respect. A significant amount of bone growth factors, vascular growth factors were found under them. And it did not depend on other factors such as the type of graft – it is a property of the membranes. And that needs to be very clearly understood.
To summarize, here are the key conclusions and practical recommendations that coincide with Dr. Boozer’s conclusions given in the book 30 Years of Guided Regeneration Third Edition.
Non-resorbable collagen membranes are now the choice for most GBR procedures.
Whereas, non-resorbable dPTFE membranes reinforced with titanium inserts may be recommended for selected vertical augmentation procedures where the stiffness of collagen membranes is insufficient.
In the second article of this series we will discuss the types of bone grafts that are used in the GBR procedures.