Wisdom extraction healing process

Contents
The operation for wisdom tooth extraction has a poor reputation and, unfortunately, some dentists try to avoid dealing with such patients. We aim to debunk some of the myths associated with the complexity of the procedure and the issues during the healing process after the extraction of wisdom teeth. Please don’t be surprised if you come across descriptions and definitions well-known to any dental school student in the article. It is known that revisiting the basics is beneficial even for practicing dentists. Additionally, we have strived to make the article understandable for specialists in related fields and for patients. There is valuable information here, especially in the section titled “What to Inform the Patient About“.
Classification of Wisdom Teeth by Extraction Difficulty
Let’s clarify from the start that there isn’t always an indication for removal. If the eighth teeth (according to ISO classification) have erupted correctly and have a normal bite, there is no recommendation for their removal. They should be monitored, and if there are no issues like cavities, there’s no need to touch them.
However, this is not always the case. Wisdom teeth typically start to erupt quite late, usually between the ages of 17 to 25. At this age, the jaw is already nearly fully developed, and often there is not enough space for the wisdom teeth to emerge properly.
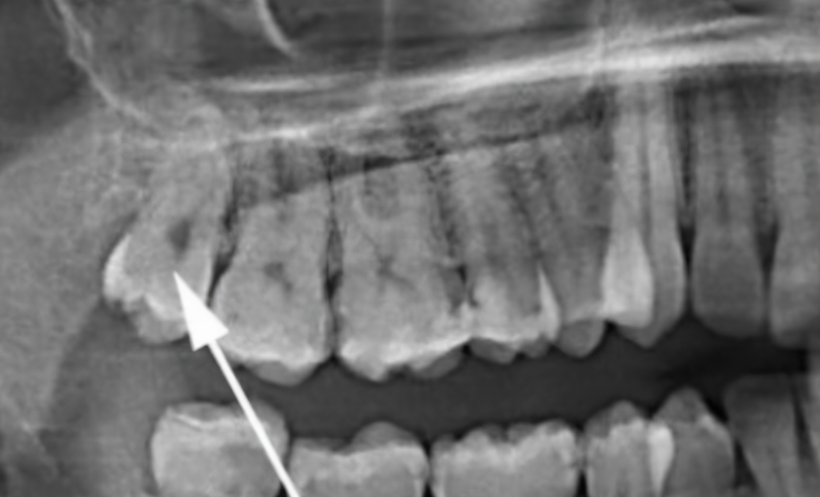
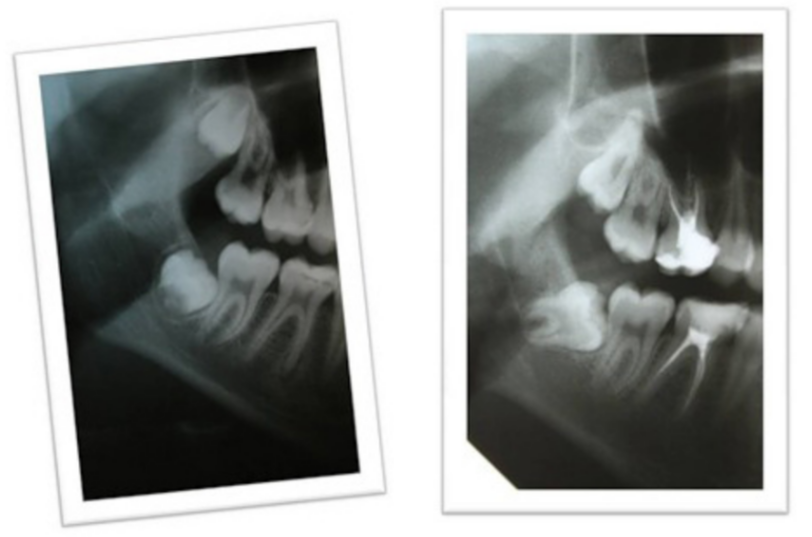
In some cases, the third molars (wisdom teeth) do not erupt (retention) because they are obstructed by the already grown and functional second molars (sevens). More often than not, retention is accompanied by dystopia (anomalous positioning), as shown in the image below.
Even if wisdom teeth do erupt, they often have an anomalous position (dystopia), as shown in the image below.
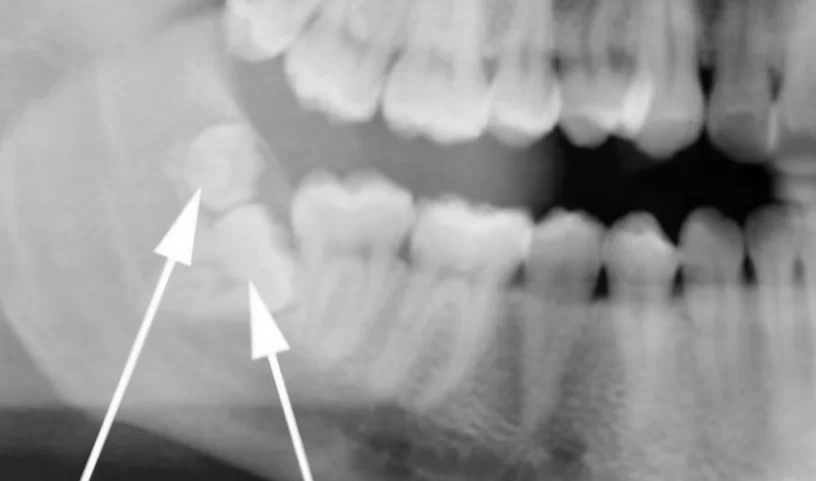
That is not all. Extremely rarely, there are cases of polydontia in individuals, where not one but two or even three wisdom teeth are present in one location, as shown in the image below. These are the most challenging cases to treat.
Let’s delve into this in more detail:
- Retention. Let’s discuss with a specific example. In the illustration below, there are images of the same patient taken with a three-year interval. Due to lack of space, the wisdom tooth got caught on the second molar and began to rotate into a horizontal position. This is a typical situation where removal is recommended.
Indications for removal – a retained wisdom tooth that has begun to rotate into a horizontal position.
It is often recommended that retained teeth are not disturbed if they are not causing any issues. However, leaving a wisdom tooth in such a position is not advisable. Let’s now understand why.
- Deformation of the dental arch. Despite the tooth not erupting and not being susceptible to issues like cavities, it still negatively impacts the entire dental arch, as shown in the illustration below. Under pressure, teeth can shift and deviate from their normal bite. Moreover, this can occur not only in the immediate vicinity of the retained tooth but also in the anterior section.
- Inflammation due to the accumulation of food residues and plaque between the seventh and eighth teeth. There is no bony partition between the sockets of the seventh and eighth teeth, forming a sufficiently deep pocket where food residues and plaque can accumulate. Microorganisms will actively multiply in this environment leading to inflammation that is practically inevitable.
- Inflammation during the eruption of retained teeth can be quite severe, especially after the age of 20. Pericoronitis is treated, and it is worth dedicating a separate article to it, but it is better to remove problematic teeth before serious inflammation develops, as shown in the photo below.
- A cyst in the jawbone tissue caused by the follicle of a retained wisdom tooth is a very serious issue. During normal eruption, the tooth follicle disappears, but in the case of a retained tooth it can lead to tumors and cysts. In the image below, there is an extensive cyst, and the patient did not feel any discomfort.
- Displaced wisdom teeth unquestionably hinder oral cavity hygiene. Moreover, they can cause other serious problems:
- Caries development and the spread of cavities to adjacent teeth. Often, cavities appear on the furthest and less visible surface of the tooth, and the patient may not notice it until the tooth deteriorates to the point of causing pain.
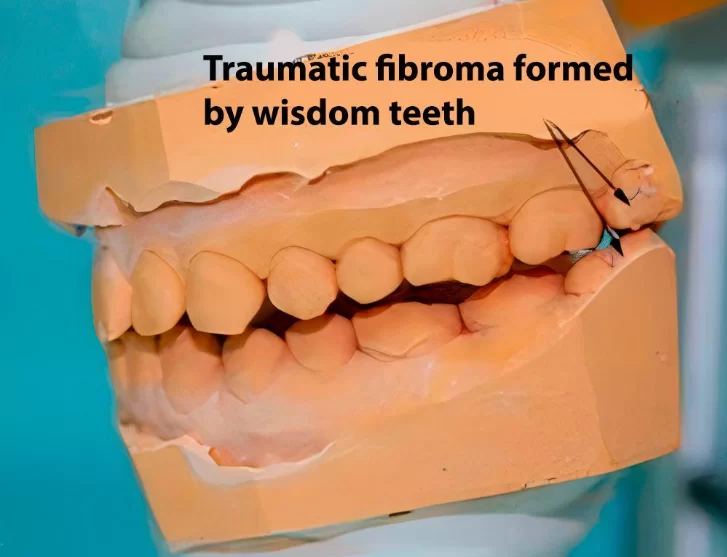
- Formation of traumatic nodes due to incorrect tooth alignment. They disrupt normal reflex connections, leading to issues with the musculoskeletal chewing apparatus. Subsequently, this worsens bite pathology, strains the chewing muscles and causes grinding in the temporomandibular joints. In other words, signs of musculoskeletal dysfunction appear. These problems can only be addressed after the removal of wisdom teeth that create traumatic nodes.
- If wisdom teeth block and prevent adjacent second molars from erupting normally, this is also an indication for removal. Take a look at the images below. The difference in time between the upper and lower images is only 21 days. After the removal of the wisdom teeth, the second molars were unblocked and almost assumed their correct position.
Let’s summarize. The only scenario where there is no indication for the removal of wisdom teeth is when they are in a normal position and actively involved in the chewing process. Removal is recommended in all other cases even if the patient is not experiencing any discomfort and there are no obvious signs of inflammation. Not only diseases and complications, but also the likelihood of future problems, serve as a reason for extraction. Conflicting opinions among dentists about when to remove wisdom teeth and when not to are related to their individual experience in performing such operations. If the surgery is challenging, time-consuming and causes significant pain and discomfort to the patient, then the specialist will often be against removal unless there are clear problems. Conversely, if the removal of even poorly positioned wisdom teeth does not pose challenges for the doctor, they will advocate for the preventive removal of wisdom teeth.
The latest removal techniques that expedite the healing process of wisdom teeth extractions
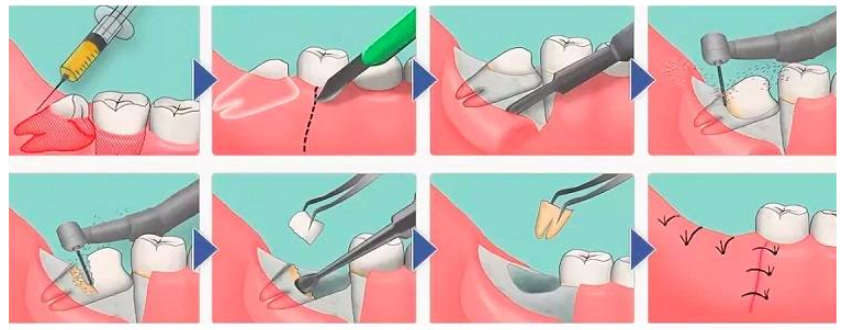
To begin with, let’s understand the standard procedure because all innovations complement and facilitate the process of wisdom tooth removal, but the general sequence of the operation is almost the same.
The wisdom tooth removal procedure consists of the following stages:
- Anesthesia is a common stage for all types of wisdom teeth removal procedures. The operation can be performed under local anesthesia or general anesthesia, and this procedure is conducted by an anesthesiologist. Let’s focus on the specifics of local anesthesia.
To minimize the patient’s discomfort, it is recommended to apply an anesthetic gel to the injection site (topical anesthesia).
For the removal of upper jaw wisdom teeth, a simple infiltration of the anesthetic in the operation area is usually sufficient.
The situation is more complicated with the lower jaw. Here, the anesthetic is directed to the nerve bundle responsible for the specific area. This procedure “turns off” the sensitivity of the lips, chin, and part of the tongue. This type of anesthesia is called regional.
Inform the patient that the anesthetic drugs may cause increased heart rate, limb twitching, and a sense of unexplained anxiety. These symptoms will subside in 10-15 minutes without consequences. Dental surgery is already a significant stress for the patient, and we don’t want them to panic about the side effects of anesthesia.
It’s also important to ensure the successful administration of anesthesia. To do this, apply a series of pressure with a special instrument in the operation area. There should be no pain, but the patient should feel the pressure. With the right anesthesia, tactile sensations are preserved. The further course of the operation depends on the type of wisdom tooth we are dealing with.
- The protocol for the removal of a impacted wisdom tooth is more complex compared to their erupted counterparts. Here are its main stages:
- Incision of soft tissues to gain access to the tooth being removed. The classical approach involves a precise incision with a scalpel. However, there are new methods, for example, using a laser for incisions to reduce bleeding and speed up healing in the postoperative period. We discuss below these innovative methods and the instruments associated with them.
- Division of the wisdom tooth into parts. This is a necessary procedure because they usually have curved, hook-shaped roots. Moreover, the tooth is often in an incorrect position due to some obstruction. It might be pressing against the adjacent molar, covered by a bony protrusion or something else. Initially, it is necessary to free the tooth from the bony plate covering its head. Then, using a special bur, we divide the tooth into 2-3 parts. There can be no compromise in the choice of tools and operating modes. If we are talking about a bur, the rotational speed should not exceed 150,000 rpm to avoid burning the bone and surrounding tissues, and the flow of cooling air should not cause emphysema in the postoperative period
Additionally, a laser or ultrasonic instrument can be used for dividing the teeth into parts.
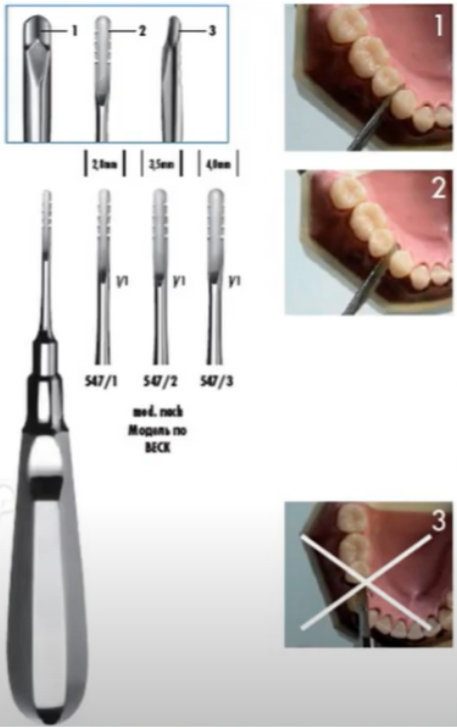
- Removal of tooth fragments and its roots. Elevators, forceps, and occasionally small pliers are used for this purpose. The specific type of elevator used is determined by the dentist’s skills and preferences, as well as the clinical situation.
After the removal of wisdom teeth, biomaterials like bone grafts are not usually used. On the contrary, the socket is thoroughly cleaned from tooth fragments using a curette. Healing occurs according to the classical scenario, where the socket is filled with a blood clot, and granulation tissue forms, and so on. The healing process after tooth extraction with bone grafting takes longer and is accompanied by a greater number of complications. However, there are specific cases where tooth extraction is associated with a significant loss of bone mass and, in such cases, a guided bone regeneration procedure is recommended. For more information on types of bone materials and barrier membranes used to restore bone volume, refer to our articles on guided bone regeneration.
- Suturing of soft tissue flaps to reduce bleeding and protect the socket from food particles. Tooth extraction healing process with stitches occurs faster because the wound volume is smaller and the chances of food residue getting into the socket are reduced. Resorbable suture material is used for suturing. Keep in mind that after the removal of a wisdom tooth the wound will still bleed, so the stitches should not be too tight and should not impede blood flow. Otherwise, the patient may experience significant swelling. The healing process after tooth extraction, how it looks with illustrations and descriptions of all stages from granulation tissue formation to the final mineralization of new bone, can be seen in the article “Tooth extraction, healing implantation.”
The protocol for extracting semi-retained teeth is virtually the same and is somewhat easier because the tooth is not as deep and access to it is better. Suturing is not always necessary in the case of extraction of semi-retained upper wisdom teeth.
- Protocol for the removal of a dystopian wisdom tooth. This operation could be called simple if the wisdom tooth has one straight root. Unfortunately this is rarely the case. In the picture below you can see a curved root that is not so easy to remove. There are usually two roots and it can be easily broken if not extracted carefully.
This type of root is also extracted using an elevator, but it is important to choose the correct shape and handle (straight or T-shaped). Otherwise, the protocol of the operation follows the same steps as the previous ones.
Now let’s take a closer look at innovative methods and tools for wisdom teeth extraction, which can speed up recovery after wisdom teeth extraction.
- Laser in wisdom teeth extraction reduces bleeding, because the laser beam “cauterizes” the capillaries in the soft tissues. Therefore, it belongs to minimally invasive surgeries compared to classical surgery with a scalpel.
The laser, which is already set to a different mode, can help with the separation of the tooth into fragments. The extraction of tooth fragments is performed with the same instruments as described above.
We will not describe the principle of operation and the element base of gas, solid-state and LED lasers, but we will give brief statistics for 2019 that which describe the share of application of dental lasers of different brands in the United States.
| Trademark | The market share percentage in the USA % |
| Biolase | 32 % |
| Fotona | 18 % |
| Convergent Dental | 14 % |
| AMD Lasers | 11 % |
| Millennium Dental Technologies | 10 % |
In addition to surgery, lasers in dentistry are also used for stimulating soft tissues and teeth whitening.
- Ultrasonic treatment of wisdom teeth before extraction. Special surgical scalers, also known as ultrasonic scalers, are used for this purpose. High-frequency vibrations applied to the wisdom tooth disrupt the ligaments holding the roots. This facilitates extraction in particularly complex cases where the tooth root is highly curved and there is a high risk of breaking it if extracted with an elevator. Ultrasonic treatment facilitates extraction although dividing the tooth into parts remains a necessary procedure.
- Minimally invasive methods. These include operations to remove wisdom teeth using laser ultrasonic scalers, as well as the use of instruments with reduced cutting edges for minimal incision of soft tissues. The use of local anesthesia and absorbable stitches also helps reduce invasive intervention and ease the postoperative period.
As for the question of how long does wisdom teeth removal recovery take, if complete healing has not occurred within 2-3 weeks you are likely to have experienced a complication. Some complications with healing depend on the patient’s health condition, for example, healing is always slower against the background of diabetes mellitus. In some cases, the patient himself can delay healing by insufficient or too intensive hygiene, smoking, etc.
Specific complications after wisdom teeth extraction
Some complications may resolve on their own, but in some cases special treatment or even a repeat surgery may be needed. Here is a list of the most common complications:
- Bleeding from the wound – may occur in the context of taking pain relievers and other medications that affect blood clotting.
- Swelling and pain in the removal area – applying ice is recommended for prevention, but swelling can also be caused by improper suturing.
- Infection of the wound or surrounding tissues – prophylactic antibiotics are recommended to reduce the risk of infection, more details on this are given below.
- Damage to adjacent teeth or nerves – this is the most complex scenario, and even experienced specialists may make mistakes. Therefore, the correct selection of instruments and constant skill improvement is critically important for the doctor.
- Dry socket – inflammation of the bony socket where the tooth was usually occurs 2-7 days after extraction. This is a rather unpleasant complication that can be triggered by the patient themselves. Inflammation of the alveolar bone occurs if the blood clot does not form properly or if it is constantly disrupted, shifted, or rinsed. Normal healing after tooth extraction vs dry socket is characterized by increased pain, exposure of bone, and a bad mouth odor. Treatment requires cleaning the socket from dead tissues, treating the socket with antibacterial gels while taking antibiotics. It is also necessary to instruct the patient on oral hygiene, consumption of solid and hot foods, and strongly advise smoking patients to quit smoking at least during the healing period. If you ask if it is possible to get a dry socket after 8 days, in some cases, it happens but it is more often associated with retraumatization in the area of the removed tooth. The occurrence of a dry socket 2-3 weeks after extraction is very unlikely. However, if the healing process was difficult due to the patient’s health condition, and the surgical site was constantly traumatized, such a late onset of dry socket after wisdom teeth removal is possible.
How to reduce pain and speed up the healing process in the postoperative period
The principle of prescribing medication after wisdom teeth removal is similar to the case of dental implant placement. In both cases, anti-inflammatory and pain relieving drugs are used and, in certain cases, antibiotics may also be prescribed.
- Antibiotics. The operation to remove teeth belongs to the second class of cleanliness of surgical wounds. This is a combined class of clean-contaminated wounds (with a moderate likelihood of introducing foreign substances or pathogenic microorganisms into the wound). This is inevitable since it is impossible to completely disinfect the oral cavity, and surgical intervention will inevitably take place in the presence of microbiota.In the dental community, there are both opponents and proponents of prophylactic antibiotic use. We advocate the use of antibiotics and will substantiate our position based on facts and the results of other specialists’ work.To summarize the research results, the number of complications in the groups receiving antibiotics is slightly over 4%. In the groups where antibiotics were not prescribed before dental implantation, the frequency of complications is about 10%.
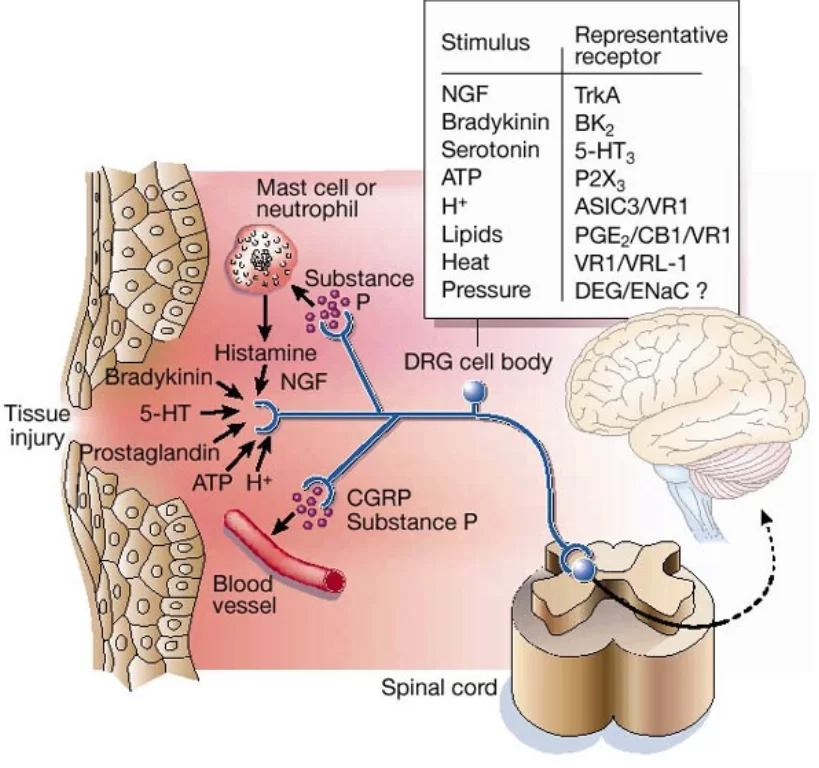
It is important for the antibiotic to be present in the patient’s blood at a sufficient concentration at the time of the operation. To achieve this, a prophylactic dose should be taken an hour or two before the operation. The action of the antibiotic during the operation is what minimizes the risk of infectious complications.However, for the sake of objectivity, we must acknowledge and explain the point of view of specialists who do not consider prophylactic antibiotic use necessary. Indeed, tooth extraction or single implantation is a relatively simple surgical procedure. The survival rate of implants, even without antibiotics, is significantly over 90%. However, wisdom teeth extraction is a more invasive operation compared to the removal of any other tooth, so prophylactic antibiotic use is still appropriate.It is extremely important to inform the patient about all risks. After all, the decision to take antibiotics should be made by the patient. If the patient has any chronic conditions that may be affected by antibiotic use, it is necessary to consult with their treating physician. Only then should the patient be provided with all available information about risks and consequences.For the prevention of infection during surgical procedures in the oral cavity, broad-spectrum antibiotics are needed. They should act on both aerobic and anaerobic bacteria, as well as on gram-negative and cocci (staphylococci, etc.) bacteria. In short, on all representatives of the oral cavity microbiota that can cause infectious contamination.Most often, antibiotics of the penicillin group are used for this purpose, for example, Amoxicillin with clavulanic acid. Clavulanic acid itself acts as an antibiotic and is effective against bacteria resistant to the penicillin group.This is not the only antibiotic with such action. The main thing at this stage is to know what action the drug should have. The specific drug will need to be selected based on the patient’s characteristics. After all, the situation where a patient is allergic to antibiotics of the penicillin group is not uncommon. The good news is that you can always find an equivalent drug with a similar effect that the patient is not allergic to or does not have other contraindications. - Pain relievers after wisdom teeth removal. After the anesthesia wears off, the patient often experiences significant pain during the first few days after the extraction. Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce the pain syndrome. These same drugs are used in the preparation stage for surgical procedures and to alleviate the condition of patients during the diagnostic stage. However, not all drugs are equally effective and safe, and they should be prescribed with great caution considering the high dosages. Moreover, it is important to understand the difference between selective and non-selective NSAIDs.The mechanism of pain transmission operates through a network of nociceptive receptors, which are present in almost all tissues of the body.
So, we need to intervene in their work and either completely disable the signal or weaken it. This can be done in two ways:
- Use local anesthesia – drugs from the articaine series completely block the conductivity of nerve endings in a specific area. Thus, any operation can be performed calmly, and the patient will not feel anything. However, the effect of local anesthesia wears off while the injury remains.
- Use pain relievers that reduce the level of sensitivity to pain. The signal is weakened or does not reach the brain, and the patient feels fine.
The vast majority of pain relievers also have another property – anti-inflammatory. This means they reduce the inflammatory reaction and, as a result, have fever-reducing properties. This helps to slightly shorten the healing period.
All these properties are characteristic of nonsteroidal anti-inflammatory drugs (NSAIDs), which are used not only in dentistry.
Drugs of this group inhibit the action of cyclooxygenase 1 and cyclooxygenase 2 enzymes. The difference is that non-selective NSAIDs block both types of enzymes, while selective ones only block cyclooxygenase 2 enzymes. The difference is easy to understand in the table below.
Selective drugs are more specific and do not harm the gastrointestinal tract. However, if the patient does not have gastrointestinal issues, they will easily tolerate the short-term use of non-selective NSAIDs even at high doses.
Let’s briefly remind ourselves of the side effects of non-selective NSAIDs. The thing is that cyclooxygenase-1 (COX-1) is an enzyme that constantly participates in physiological processes and performs essential functions. For example, in the gastrointestinal tract, COX-1 is involved in prostaglandin synthesis in the mucous membrane of the stomach and intestines. Here, it serves a protective function by preventing the erosion of the mucous membrane. For instance, in the stomach, our own hydrochloric acid is a fairly strong damaging agent. COX-1 helps preserve the mucous membrane. Nonsteroidal anti-inflammatory drugs disrupt the structure of cyclooxygenase-1.
Not only hydrochloric acid but also many components of bile and other enzymes have a negative effect on the mucous membranes of the intestines, kidneys, and vascular membranes of the liver. In all these cases, non-selective anti-inflammatory drugs inhibit COX-1, thereby reducing the protection of the mucous membrane. Consequently, against the background of taking nonsteroidal anti-inflammatory drugs at high doses, peptic ulcer disease may exacerbate, and internal bleeding caused by mucous membrane damage may occur. These are serious side effects that must be communicated to the patient.
In the family of nonsteroidal anti-inflammatory drugs, there are well-known names not only to specialists.
- First and foremost are analgesics (metamizole), including Analgin, Baralgin, Pentalgin, and others. All of these belong to non-selective drugs. The maximum single dose is 1000 mg, and the maximum daily dose is 3000 mg.
- Equally well-known is ibuprofen, sold under commercial names like Nurofen, Brufen, Solpadeine, etc. The maximum single dose is 200-600 mg, and the maximum daily dose is 2400 mg. When taken, it also inhibits both types of cyclooxygenase. Let’s delve into this one in more detail as this drug is considered strategically important and is labeled as the gold standard in many studies for treating acute or chronic pain.
- Ketorolac is also a non-selective anti-inflammatory and analgesic. It can be found under names like Ketorol, Ketanov, Dolak, and others. The maximum daily dose is 10-30 mg, and the maximum daily dose is 90 mg. This drug is considered quite potent and is well known to both dentists and patients. This reputation is well-deserved; in the mid-90s, when it was first introduced, ketorolac was highly anticipated since its effects in some cases were comparable to opioid analgesics.
Less well known among patients, but well familiar to doctors, are selective nonsteroidal anti-inflammatory drugs (NSAIDs):
- Celecoxib (Celebrex) – maximum single dose 200-400 mg, maximum daily dose 400 mg.
- Etoricoxib (Arcoxia) – maximum single dose 60-90 mg, maximum daily dose 120 mg
They selectively act on COX-2 and do not affect COX-1.
Another noteworthy drug and its derivatives is Nimesulide. It belongs to moderately selective drugs, with a maximum daily dose of 100-200 mg and a maximum daily dose of 400 mg. Even among pharmacologists there is no consensus on whether to classify it as a selective or non-selective drug.
Also, let’s remind ourselves that a positive effect occurs when taking high doses of NSAIDs (close to the maximum allowable). Therefore, it is important to protect the patient from side effects before they occur. Let’s delve into possible side effects in more detail:
- GI Tract – a decrease in the protective potential of the mucous membrane leads to its damage under the influence of external factors such as gastric hydrochloric acid, bile acids, enzymes, bacterial activity in the small and large intestines, and so on. The good news is that patients with erosion, ulcers of the stomach or duodenum, are aware of their problems. This means that measures can be taken immediately against potential complications.In addition to ibuprofen, an inhibitor of the proton pump should be taken, for example, the widely known Omeprazole.The second option to reduce the risk of complications is to prescribe the patient selective NSAIDs, for example, from the coxibs group (Celecoxib).
- Blood pressure often rises with the use of NSAIDs. Moreover, there is no special difference between selective and non-selective drugs in this regard. Rofecoxib and etoricoxib demonstrated the most significant negative impact on blood pressure. The good news is that wisdom teeth removal is typically performed on relatively young patients. However, if the patient already has problems with the cardiovascular system and hypertension, it is essential to consult with their attending physician.
- Impaired blood clotting is not a frequent side effect, but it should also be considered. In this case, there is a risk of bleeding and a delay in the healing process. Fortunately, there is data and authoritative research that indicate ibuprofen, in particular, is an effective analgesic and its use is not associated with an increased risk of bleeding.
- Allergy to NSAIDs most often occurs in patients who have:
- Hypersensitivity to aspirin. Typically, the patient is aware of this and can provide timely notification.
- Upper respiratory tract disease – nasal polyposis.
- Lower respiratory tract disease – asthma.
Such patients should only be prescribed NSAIDs with great caution and after consulting their attending physician or allergist.
Based on clinical trials, the following recommendations have been developed for the use of NSAIDs.
- The lowest risk of complications from all parts of the GI tract is observed with Celecoxib. It less frequently causes complications in patients at risk for GI tract compared to non-selective NSAIDs in combination with a proton pump inhibitor. Celecoxib has the lowest risk of developing GI bleeding, ulcers, dispersions and gastrointestinal disorders (GI disorders).
- Etoricoxib reduces the risk of dispersion and asymptomatic ulcers but does not reduce the risk of GI bleeding, including from the distal parts of the GI tract.
- Aceclofenac, meloxicam, and nimesulide less frequently cause dispersion and asymptomatic ulcers compared to other non-selective NSAIDs.
- Naproxen and celecoxib destabilize arterial hypertension to a lesser extent.
What to Warn the Patient About
We understand that most dentists are already familiar with what is written below, but let’s reiterate to refresh the memory.
- Do not rinse the operation site with anything other than clean water, and even then, moderately. Otherwise, you can wash away the blood clot and complicate the healing process.
- Never warm the area of the extracted tooth. On the contrary, it is recommended to apply ice to the cheek on the first day after tooth extraction. Keep the ice on for no more than 15 minutes to an hour. This will reduce the swelling, but do not keep the ice too long or you may overcool the throat and nearby lymph nodes.
- General overheating of the body should also be avoided. Saunas and hot baths should be avoided for several days. Overheating contributes to bleeding.
- Exclude significant physical exertion, at least for 3 days. Fitness and heavy physical work increase blood pressure and, during this period, the blood clot is not yet completely formed and the wound may bleed slowing down the healing process.
- Do not eat until the anesthesia wears off. Otherwise, there is a risk that the patient may bite their tongue, the inner surface of the cheek or lip and not notice it. Local anesthesia usually wears off after 2-3 hours.
- When eating, chew on the opposite side from where the wisdom tooth was removed. This will minimize the risk of food getting under the suture material or into the socket.
- Oral hygiene. It is essential to brush the teeth with the softest toothbrush the patient can find to avoid injuring the area where the tooth was removed. Most importantly, inform the patient not to remove the white coating that may appear on the gum in the area of the removed tooth. This is fibrin, and its presence indicates normal and sufficiently intense healing of the socket. The formation of white plaque during the healing process after tooth extraction is normal
In conclusion, it can be said that experienced specialists optimize the treatment protocol for a specific clinical case and may combine techniques, such as using a laser and ultrasonic tissue softening around the tooth root. If you are a novice specialist, arrange for more experienced colleagues to assist you in tooth extraction surgeries. This experience will accelerate the acquisition of the necessary skills.