How to Sell Treatment Using Implants Effectively
Contents
The commercial aspect of dental practice aligns with the concept of sales in other businesses. Let’s recap the core principles:
- Client (Patient) Awareness of the Problem: Without this, further progress is impossible. If a patient doesn’t experience pain or significant discomfort, they may not perceive a problem at all. For instance, the absence of a single premolar might not severely impact daily life; a person can adapt and live with it for years. However, various triggers can initiate awareness. A negative experience, such as bad breath or yellow teeth affecting a date. Or, during a routine examination, a dentist identifies unusual wear, wedge-shaped defects, and asks probing questions. The patient may then realize they grind their teeth at night, or clench and grind when stressed. Jaw pain or headaches after eating might also be triggers. Before this moment, the patient might not have recognized these as problems with potentially serious consequences.
- Finding a Solution and Analyzing Options: The patient visits various clinics and private practices, receiving consultations and treatment plans with associated prices for each option. They may be presented with various solutions: temporary or permanent, affordable or expensive. This stage is crucial for us as specialists. We need the patient to schedule an appointment. To achieve this, the patient must first learn of your clinic or practice. Importantly, even before the initial meeting, you must inspire trust and a sense of rapport. It is important to solidify your position at this stage by presenting several treatment alternatives. Your proposal should be clear and easily understood. If the patient consults other providers, they will already be equipped with critical thinking, noticing omissions and shortcomings in other plans. This significantly increases the likelihood of them returning to you.
- Choosing a Solution: Eventually, the patient selects a clinic or a specific dentist and agrees to treatment. This represents a victory, indicating that you and your team have done everything correctly.
- Closing the Deal and Receiving the Service: In our context, this means the restoration of one, several, or even a full arch of teeth supported by implants. It encompasses all stages, from surgery and implant placement to the fitting of a permanent prosthesis.
- Using the Solution to Resolve the Problem: In this case, it’s a prosthesis supported by implants. It’s vital to monitor and support the patient long-term.
Now, let’s examine in detail how to approach the first three points.
Always Have a Comprehensive Treatment Plan
Think proactively, focusing on the patient’s benefit. Even if a patient arrives with a single complaint, the examination will likely uncover additional, unperceived issues. This isn’t about pushing unnecessary procedures. It is about informing the patient of actual issues they are unaware of, so they understand the full picture. For example, a patient may seek a filling, but an X-ray reveals a cystic granuloma, which is asymptomatic. Or, an impacted eighth molar (wisdom tooth) may be pressing on the adjacent seventh molar, causing hidden caries.
Regarding implants, we should immediately develop a treatment plan that accounts for all existing problems and future restorations the patient might require one or two years after addressing the immediate issue.
A strong example was discussed in a previous article: “Planning Implant-Supported Restorations: From Single Tooth to Full-Arch.” The patient initially presented with mobility and pain in the upper front teeth, while the bridges in the posterior regions did not bother them.
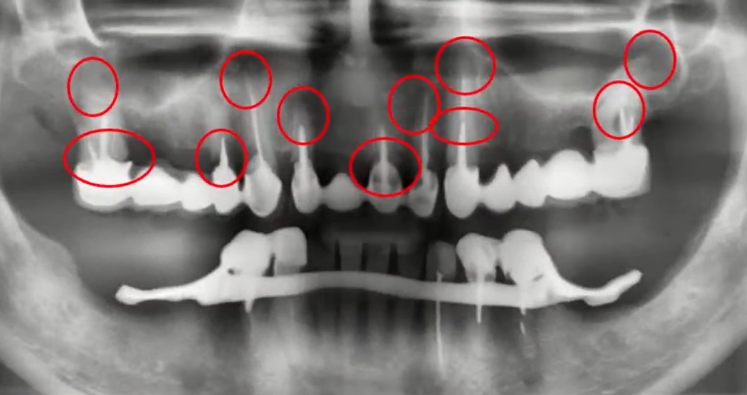
The patient’s complaints are regarding the four mobile and painful front teeth of the upper jaw. Problem areas are marked in red, including those not yet causing symptoms YouTube / Dr. Kamil Khabiev / Dental Guru Academy
The patient’s primary complaint was focused on the front teeth, but the image clearly indicated that the posterior bridges were failing. The dentist discussed all the problems and presented a comprehensive treatment plan. Initially, the patient agreed only to the first stage – removing the front teeth and restoring them with three implants. Some months later, one of the bridges fractured, and the patient returned to the clinic. They were then shown the previously prepared comprehensive plan. Ultimately, within a few months, the patient not only completed a full restoration of the upper arch, but also replaced a clasp denture on the lower arch with fixed implant-supported bridges. This was initially not part of their plan.
If the patient had not been presented with the comprehensive plan initially, this successful outcome might not have happened. The surgeon and prosthodontist collaborated from the outset, planning implant placement with the entire restoration in mind.
What if the patient only had the presenting problem addressed, then the bridge fractured, and they sought care elsewhere, receiving another two or three implants. A year later, the second bridge would likely fail. The result would be chaos: implants in suboptimal positions and restorations altered by different clinicians. This leads to numerous problems and potential complications. It all stems from the first specialist not offering a complete course of treatment and not explaining the potential problems that might arise. When the forecast began to become reality, the patient’s trust in the first doctor would grow significantly. This patient would be unlikely to be swayed by the argument that the same treatment could be done at a lower cost.
A comprehensive plan may seem obvious, but few dental professionals routinely develop them and explain all the nuances to the patient in detail. The patient must understand not only the benefits but also the consequences of inaction. For instance, bone loss and decreased bone density are irreversible processes.
Other consequences of inadequate planning include haphazard implant placement, often developing over time. A patient presents with a problem with a single tooth, which is removed, and a single implant with a crown is placed. Subsequently, a nearby tooth or others are lost, leading to additional single-tooth restorations. Sometimes, teeth “fall out” faster than the implants integrate. This creates a cycle without consideration for neighboring teeth or the possibility of using those implants for a complete restoration. Considerations such as::
- Can these implants be used for a full-arch restoration? What type of interface do they have (planar or conical)? Will the abutment withstand increased lateral loads?
- Is there enough space between implants for adequate bone nutrition?
As a result, patients can end up in situations where some implants must be removed, and new ones are installed in areas where gaps of three or more teeth exist. All this stems from inadequate initial planning.
What Should Be Included in a Comprehensive Treatment Plan?
After (and only after) the patient recognizes the problem, a comprehensive treatment plan should be presented. A good plan includes:
- At least three treatment options with different budgets:
- Minimal: Depending on the situation, this might involve an all-on-4 system with a polymer prosthesis or even a removable denture. This option, even if temporary or incomplete, should provide a functional solution the patient can utilize.
- Maximum (Ideal): This uses the best possible materials, possibly individual abutments in all areas of the jaw, and implants from well-known brands.
- Optimal: This is the plan the patient is most likely to choose. It logically aligns with the maximum plan, employing the same implant arrangement for ideal load distribution. However, it may use implants from a mid-price range or use 8 implants instead of 10. Successful restoration is generally achievable with any FDA-approved implants, as demonstrated by successful cases with Uniqa Dental implants. The price difference will be significant. The optimal plan might use individual abutments only in the aesthetic zone and standard titanium abutments in the lateral areas. It’s crucial that the patient understands this option is not significantly inferior to the maximum one in terms of functionality and durability.
A secret: patients often choose the optimal plan and later expand it to the maximum during the treatment process. Do not tell your patients this.
The laws of psychology apply here; if you name a person one price, let it be the price of a balanced and optimal treatment plan, for example, $22,000, then they won’t understand whether the price is high or low, they have nothing to compare it with. And most likely, they will go looking for something cheaper. But if you give three options: $7,000, $22,000, and $48,000, and explain that the $7,000 option is a temporary prosthesis that will most likely be disappointing, they are much more likely to choose between the $22,000 and the $48,000 options. $22,000 then feels like an acceptable amount to resolve dental issues for the next 20 years. - Clearly Defined Stages of Treatment: This includes the duration of each stage, including healing and rehabilitation. This is critical, because the patient may not have funds for the entire treatment initially. You might start with four implants in the anterior area, placed in a way that allows additional implants in the posterior for a symmetrical and balanced restoration in the future.Details can also address potential patient complaints. For instance, the patient should be informed that swelling and discomfort are expected in the first week post-surgery and what medication will help alleviate those symptoms. If a temporary prosthesis is fitted, the patient should be aware of its limitations and expected lifespan. Unfortunately, some patients disappear for years after a temporary prosthesis is placed, never returning.
How to Answer the Question – Which Implants are Better?
The recommended answer is that there isn’t a single ideal implant, but rather an ideal implant for specific clinical cases.
The dentist always chooses implants based on specific indications, such as:
- Implant shape
- Thread profile
- Diameter, etc.
This is not brand-dependent. The dentist selects the required configuration and orders from a manufacturer that offers those shapes. The illustration below shows a schematic of different implants for different clinical scenarios.
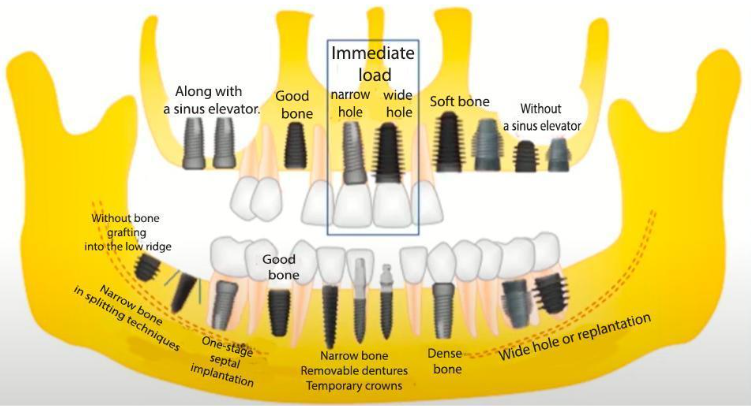
Approximate schematic of how implants of different shapes might be used in various clinical situations YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Choosing implants according to indications also helps avoid sinus lifts or combine implantation with ridge splitting, reducing the need for complex bone grafting. While common, these procedures have fairly high complication rates. Implantation patients, especially those needing total restorations, are often elderly and have underlying health conditions. Therefore, complex grafting should be avoided whenever possible.
The concept of selecting different implant types can be part of an optimal treatment plan. Explaining the risks avoided and your rationale for a specific set of implants can further increase trust. Again, the patient has a choice, this time between a good and an excellent option. Once the patient understands all the available options, associated costs, and time commitment, they will unlikely seek other opinions. Even if they do, your approach will appear more complete and thoughtful, increasing the likelihood of them returning to your practice.
.
How to Discuss the Price of Treatment
Avoid using words like “cheap” or “economy class” when presenting a treatment plan. These terms are subconsciously associated with low quality or limited capability. When presenting the three treatment options, use terms like:
- Basic or standard
- Optimal
- Premium
The difference between these options should primarily reflect the complexity of treatment, and to a much lesser degree, the implant brand. The patient should be assured you use high-quality implants and superstructures in all cases. What they are paying for is the complexity of the work and the expertise of the dentist ensuring even complex procedures are completed without complications.
For instance, placing one or two implants into a well-healed bone is a straightforward procedure, taking only 15-20 minutes. Tooth extraction with simultaneous implantation is more complex and demands a higher skill level from the surgeon. Implantation combined with alveolar ridge splitting adds further complexity.
As previously stated, bulk bone grafting should be avoided when possible. Yet, the cost of treatment with and without bone grafting can be similar. The second option reduces the risk of complications, but simultaneously, the complexity of the procedure increases and a highly skilled surgeon is needed. The scope and complexity of the work largely determine the final treatment cost.
Implant treatment is expensive, and patients often ask for discounts. Some dentists, fearing the loss of a patient, readily agree to a discount. However, we recommend the following options:
- Staged Payments, No Discount:. Total restorations often require six months or more. Offering staged payments, perhaps for each phase of treatment, allows the patient to spread the cost over six to nine months.
- Full Upfront Payment with a Discount: This is another acceptable option. The patient pays the full amount immediately, but at a slight reduction compared to the total cost stated in the treatment plan. This is psychologically more appealing; the patient feels they benefit.
If the patient starts negotiating, it’s a positive sign indicating their interest. At the start of the communication, patients are often unsure of the value you provide and are testing the waters. The ultimate goal is to convince the patient that the result they will receive is worth much more than the cost of the procedure.
Offer More Value Than Competitors for the Same Price
One of the best options is to offer soft tissue plastic surgery as a bonus. For instance, an apically displaced flap procedure is relatively simple and does not involve significant additional costs.
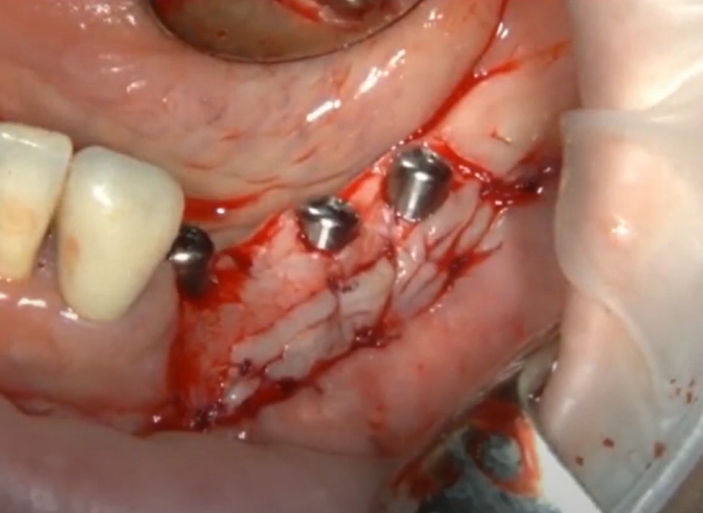
Soft tissue work being performed after the installation of three implants and three healing caps YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Some specialists might perform such procedures in multiple stages and charge separately for each. However, the doctor shown in the example performs it during the implant placement and the patient is only charged for the implants and healing caps. Therefore, the patient receives a more highly skilled surgeon but pays less than they would in another clinic.
We advise dentists to use their skills and expertise as the basis for marketing. This approach creates a win-win situation.
From the surgeon’s perspective, this procedure took an extra ten minutes and only used a scalpel and suture material. Since the soft tissue dissection and flap raising would have been necessary for the implantation in any case, the preparatory part of the surgery is also the beginning of soft tissue plastic surgery. As a result, the patient receives more value than if they had gone to another clinic where this procedure is not offered or is offered at an additional cost.
A satisfied patient will share their positive experience, and someone else is highly likely to seek your care based on that recommendation.
Offering free healing caps if you know the patient will complete their prosthetics in the same clinic is also an option. With proper care,healing caps can be reused, which means there is no cost to you.
Each clinical case is unique. Therefore, you must assess individually what you can offer as a bonus to distinguish yourself from competitors.
How to Present a Complex and Expensive Treatment Plan
It is strongly discouraged to present all the information on the first visit. This is especially true for the cost of the treatment. Instead, after the initial examination and X-rays, briefly outline a few treatment options. Highlight the patient’s problems, the risks of not doing anything, and the prospects for treatment. Invite the patient back for a second visit. Use that time to develop detailed treatment options, consult with the prosthodontist, etc. If the patient does not return, that is fine, you will not worry about whether the price you quoted was too high.
Patients who attend the second visit have likely thought about the problem and are more trusting. They are much more likely to choose one of the proposed treatment options.
Practical experience shows that if you state the price immediately, this often causes rejection due to the patient feeling overwhelmed with information. People need time to process and understand their situation.
How Does a Clinic Coordinator Influence Sales?
A clinic coordinator doesn’t have to be a person with specialized medical training, but it’s highly desirable. Coordinators are often students or those who haven’t finished their studies, or even doctors who cannot provide treatment for various reasons. This may be due to health limitations or a lack of psychological readiness for surgery. However, these individuals may be excellent managers and coordinators.
A busy surgeon or dentist is likely overloaded with work. They lack the time needed to build trusting relationships with every patient they consult. For a coordinator, personal interaction and communication is the focus of their activity.
The coordinator does not define the treatment plan, but works with the cost. Often, they calculate the final treatment cost.
The coordinator may offer the patient credit options or a payment plan. They also coordinate appointment times.
Patients often confide more openly in coordinators, asking questions they forgot to ask the doctor.
For example, the patient may have had a successful surgery and implant integration at a high-quality clinic. However, when it was the prosthodontist’s turn, they experienced discomfort. Perhaps they disliked the doctor’s smoking habit.
If the patient has a trusting relationship with the coordinator, the patient can mention it and ask for another doctor to work with. They are unlikely to mention this to the doctor directly and might have left for another clinic without completing treatment.
Additionally, the coordinator:
- Provides the patient with additional information, ensuring it’s clear. Patients can be overwhelmed during a consultation and may forget to ask questions or not understand some of the information. After the consultation they may remember, for example, “What is better, metal-ceramic or zirconium?”.
- Shows similar case presentations (the doctor does this as well), which is a powerful sales tool. Without demonstrating successful cases, convincing a patient to choose your clinic is difficult. Demonstrating successes sells your practice and your expertise. Therefore, develop an organized bank of cases and presentations to show patients cases similar to their own.
- Answers “basic” questions such as, “Which implants are better?” or “Why do we need this procedure?”.
- Schedules visits and advises on preparation for surgery.
- Follows up with the patient after surgery, checks on their progress, and answers further questions.
Often, the coordinator is why a patient chooses a more expensive treatment option. For example, a doctor may offer metal-ceramic or zirconia prosthetics, leaving the patient to choose. The coordinator can explain that metal-ceramics can oxidize and develop defects over time, whereas zirconium is more stable. They can also provide pictures and samples. As a result, the patient might choose zirconia.
Building Trust Through Social Networks and Free Advice
The platform can be any: Facebook, Instagram, your office or clinic’s website, etc. Content focusing on two main topics tends to be the most effective:
- Successful cases with explanations as to why it was performed that way and what the outcome was. You can even offer a discount in exchange for permission to publish a case study. Be sure the agreement between you and the patient is in writing.
- Tips and tricks. For example, how to care for different types of dentures, both removable and implant-supported. Is there a difference in care between zirconium and metal-ceramic prostheses? What to do if you have gum inflammation and can’t immediately get to a dentist?
This approach is very effective. A potential patient sees this information and thinks, “This doctor explains things very well, I wish they could help me with my problem.” If a patient comes through social networks, 50% of the needed trust has already been established.
If you are not yet utilizing social media, start soon. Regular, consistent posting (at least once a week) is more important than posting daily. The results might not be noticeable immediately, but you can never know which video will gain widespread attention.
What Questions Do Patients Most Often Ask?
We have already discussed this a bit, but here are some of the most common questions:
- Doctor, which implant is better? The best answer is to say the implant that perfectly fits their specific clinical case is the better option. You can then explain bone density, immediate versus delayed implant placement, etc. Be prepared to answer this question calmly and logically.
- Why is this implant cheaper? Is it worse? No, all implants approved for use are of high quality. The price is dependent on the complexity of the case. A simple, inexpensive, single-thread implant is suitable for simple cases such as a single-tooth defect, provided the alveolar ridge has sufficient height and volume. Implants that can be installed in the socket of a freshly extracted tooth require completely different specifications and have different prices.
- What is the advantage of an expensive implant? The answer is in the previous points.
- How does an expensive implant differ from an inexpensive one?
- Can I get inexpensive implants instead of expensive ones?
Finally, let’s summarize. You will consistently attract patients if you:
- Occupy all market segments:
- Basic
- Standard
- Premium
- Can perform implantation in any clinical situation.
- Develop unique additions to the primary treatment—something your competitors don’t offer, like the soft tissue procedures we mentioned earlier.
- Learn to sell services and increase revenue by regularly seeing existing patients.
- Establish fair pricing. The prices do not need to be low, but the patient must feel that they are receiving more value than the money they spent.
That’s all for now, until the next publication.









