How to correct gingival recession
Contents
Gingival Prolapse and Treatment Methods
In this article, let’s understand the causes of gingival prolapse and treatment methods. Let’s start with definitions and classification.
The healthy gingiva covers the crown of the tooth by 1-2 mm and covers the line between the enamel of the crown and the cementum of the tooth root surface. The healthy gingival cuff rests on the attached keratinized gingiva. Gingival recession is a pathological condition, usually accompanied by inflammatory processes, in which there is thinning and displacement of the gingival edge, which leads to the exposure of the tooth root. Gingival recession can be localized, in the area of 1-2 teeth, or generalized, affecting the entire tooth row.
The Danger of Gingival Recession for the Patient’s Health
- Discomfort and difficult hygiene. The gum peeling away from the tooth creates a pocket that is difficult to clean. As a result, plaque and food debris accumulate in it, leading to bad breath, inflammation, and suppuration. The situation is especially paradoxical if the recession is «earned» by the patient’s over-intensive brushing and excessive flossing pressure. An excessive desire for hygiene leads to an inability to maintain it at a basic level.
- Increased sensitivity and severe painful sensations. The bare tooth root is unprotected and reacts to touch, hot and cold food, and air movement. The discomfort causes you to touch the gum with your tongue more often, provoking even more peeling.
- Tooth decay and loss. The unprotected root is exposed to unfavorable external factors, leading to carious and non-carious tooth lesions. Over time, the volume of lesions progresses, leading to nerve damage and, in the most advanced cases, even tooth extraction.
- Tooth mobility. In parallel with the loss of gum, the bone tissue around the tooth is resorbed, which leads to tooth mobility. With progressive mobility, tooth extraction may be a consideration.
Types of Gingival Recession Classification
Miller’s Classification:
- Grade 1 – the depth of recession does not reach the mucosal-gingival junction. Only the loose (unattached) part of the gingiva is slightly reduced.
- Grade 2 – recession extends beyond the mucosal-gingival junction. The attached part of the gingiva is reduced, but the main gingival and bone tissues are preserved.
- Grade 3 – the interproximal papilla (the gum tissue between the teeth) disappears and the lateral surfaces of the tooth are exposed.
- Grade 4 – circulatory loss of soft and bone tissue around the tooth. The tooth is completely exposed around the circumference of the tooth, including the interdental spaces.
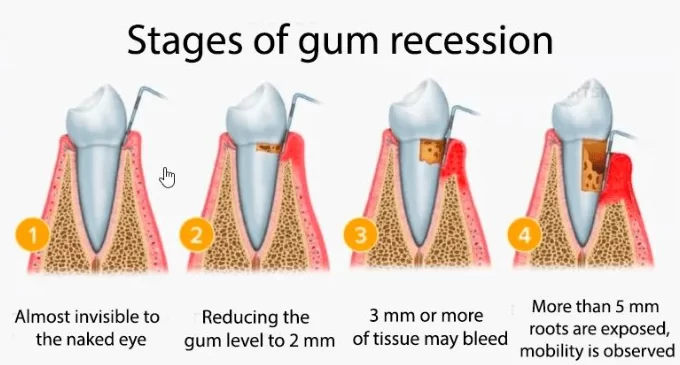
Classification by depth:
- Light: up to 1 mm
- Medium: 1-3 mm
- Severe: more than 3 mm
A distinction is also made between open (visible) and hidden (detected only by probing) gum recession.
Also in this article, we will address a similar problem – restoring the volume of attached keratinized gingiva to form a stable gingival cuff in the case of an implant.
Causes of the Gingival Recession
- The most common and paradoxical cause of gingival recession is improper brushing technique. The use of stiff brushes, abrasive kinds of toothpaste, and traumatic flossing motions can damage the gums and cause them to recede from their physiologic level.
- Poor oral hygiene is the opposite situation. Recession can be caused by plaque buildup and bacteria leading to gum inflammation, which can become chronic and trigger recession. These two problems have the most favorable treatment prognosis if the patient changes their habits.
- Malocclusion of teeth: malocclusions can place uneven stress on the gums, which can lead to gum recession. If the front teeth are crowded and are the first to take the load of chewing, the recession is inevitable because the cortical bone is thinning and receding, and with it the gum. In such a case, only comprehensive treatment to correct the dentition and surgical restoration of the gum level can help.
- Poor-quality prosthetic constructions: crowns, bridges, and fillings with improper fit to the tooth can traumatize the gums and cause them to recede. For example, you can see in the image below that the filling is disrupting the eruption profile and putting pressure on the soft tissue, which will inevitably lead to gum recession. And in this case, successful treatment is not possible without remodeling the crown.
.

. - Unhealthy habits: smoking, drinking alcohol, and other psychoactive substances negatively affect the condition of the gums and can lead to their recession.
- Periodontal diseases: periodontitis, gingivitis.
- Physiologic recession – is observed in elderly people and is associated with aging tissues, inflammatory processes in this case are weakly expressed or not observed at all, and the teeth remain stable.
- Systemic diseases: diabetes mellitus, osteoporosis, autoimmune diseases.
- Hormonal changes: pregnancy, menopause.
- Vitamin and mineral deficiencies: deficiency of vitamin C, calcium, and zinc.
- Taking certain medications: anticonvulsants, antidepressants.
Diagnosis of Gingival Recession
During the examinations, the doctor needs to record all the points to decide the need and possibility of treatment. Identifying whether the recession is a primary disease or a concomitant disease is also important. In the latter case, the underlying cause should be treated first.
Visual Assessment:
-
Color Evaluation:
- A healthy gum line has a pale pink color
- When gum recession occurs, there may be a discoloration of the gum:
Redness: inflammation, combined with swollen gums and bleeding may indicate an associated disease, periodontitis.

Pallor can be a sign of recession without inflammation, but a whitish tint to the gums can also indicate periodontal disease.
Cyanosis: impaired blood supply.
2. Shape Assessment:
- A healthy gingival margin has a festooned contour
- With gum recession, there is a change in the shape of the gum:
- Flattening: loss of festooned contour.
- Rounding: smoothing of the gingival margin.
- Retraction: formation of a deepening in the recession area.
3. Size Assessment:
- The class of tooth root exposure is visually assessed
- The following gradations are used:
– Light: exposure of up to 1/3 of the crown height.
– Medium: exposure of 1/3 to 2/3 of the crown height.
– Severe: exposure of more than 2/3 of the crown height.
Measuring the level of gingival recession:
-
Probing:
- A periodontal probe is used
- The distance from the gingival margin to the cementoenamel margin is measured
- Values are written at 4 points around each tooth:
-
- Mesial-bucal.
- Distal-bucal.
- Mesial-lingual.
- Distal-lingual.
Gingival Index (GI):
The degree of gingival inflammation is assessed. A 0-3 scale is used:
- 0 – no inflammation
- 1 – mild inflammation (redness, swelling)
- 2 – moderate inflammation (redness, swelling, bleeding)
- 3 – severe inflammation (redness, swelling, bleeding, purulent discharge)
Additional diagnostic methods:
- Photographic recording:
- Allows you to dynamically monitor changes in the level of gingival recession
- Pictures are taken using standardized anglesExamination through a binocular microscope to accurately define the cemento-enamel junction boundary.
X-ray and CT scans:
- The degree of bone resorption in the area of recession is assessed
- Both targeted shots and an orthopantomogram are used
- It is also used for differential diagnosis to rule out similar diseases (tooth extrusion, periodontal disease, etc.)
If the diagnosis is made and it is confirmed that gingival recession is not associated with other diseases, we start treatment.
Gingival Recession Treatment and Correction Methods
Treatment cannot be successful unless the traumatic factors are removed. If it is improper brushing or poor oral hygiene, it is quite easy to remove such factors. But gingival recession can also be caused by:
- Anatomical features of the patient
- Improper design of braces that make it difficult to clean your teeth
- Poorly fitted crown or dental bridge that presses on the gum or interferes with the normal bite
In such cases, it may require fairly long and complex treatment, including denture replacement or orthodontic treatment. In the following, we describe a standard protocol that assumes the traumatic factors have been eliminated or are in the process of being eliminated:
- Professional dental cleaning and removal of deposits both on the teeth and from gum pockets.
- Dental treatment. In the vast majority of cases, the teeth around which gum recession is observed need the removal of carious and non-carious defects. If tooth shape defects that affect gum recession are identified, it is quite common to correct them with odontoplasty.
- If the gingival recession is moderate, it is possible to manage with conservative treatment methods after the traumatic factors have been eliminated. The patient is prescribed the following:
- No toothbrushing and flossing for 2-3 weeks
- Anti-inflammatory rinses, gels and ointments
- Therapy with antibiotics in case of significant inflammatory processes
- Drugs to stimulate the growth of gum tissue, often vitamin and mineral complexes containing vitamin C, vitamins A and E, as well as calcium and magnesium
Collagenoplasty is also among the conservative methods. The essence of the method is the placement of collagen materials, in the form of sponges, gel, etc., into the defect area. In either case, these are resorbable materials that the body recycles and uses to regenerate its own tissues.
4. Surgical treatments. Unfortunately, surgical intervention is required in almost 90% of gum recession cases. This is due, among other things, to the late treatment of patients, when the situation is already very advanced. In the most severe stages, complete recovery even by surgery is not possible, but improvement is always possible. At least cover the margin between the enamel and the root cement with gum. The most common surgical treatments for gum recession are:
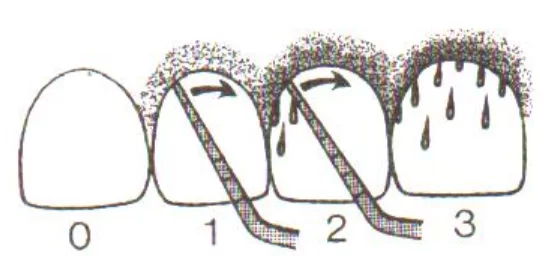
- Tunnel technique without papilla peeling. Many specialists use it successfully. The essence of the method is the gingival detachment without rupture of the papillae with the subsequent placement of a connective tissue graft in the space under the detached gingiva (tunnel). The graft will engraft and restore soft tissue volume and most importantly restore the attached keratinized gingiva. For all its advantages, the tunnel method is only suitable for treating mild to moderate gingival recession.
There are many nuances and varieties of tunnel techniques for gingival restoration, we will not analyze them, as it is impossible to learn and apply the technique on the materials of the review article. If you, as a practitioner, do not yet know the surgical techniques of gingival recession treatment, it is recommended to undergo training, at least watch webinars and recordings of surgeries with comments from more experienced colleagues.
- Vertical flap displacement with papilla peeling. Vertical displacement can be performed with or without a graft. The most common and promising at the time of this writing is Dr. Giovanni Zucchelli’s method. If you’re not already familiar with this technique, we also recommend getting trained and incorporating it into your arsenal. For more information on soft tissue management around implants, read our article on Attached Keratinized Gingiva Issues.
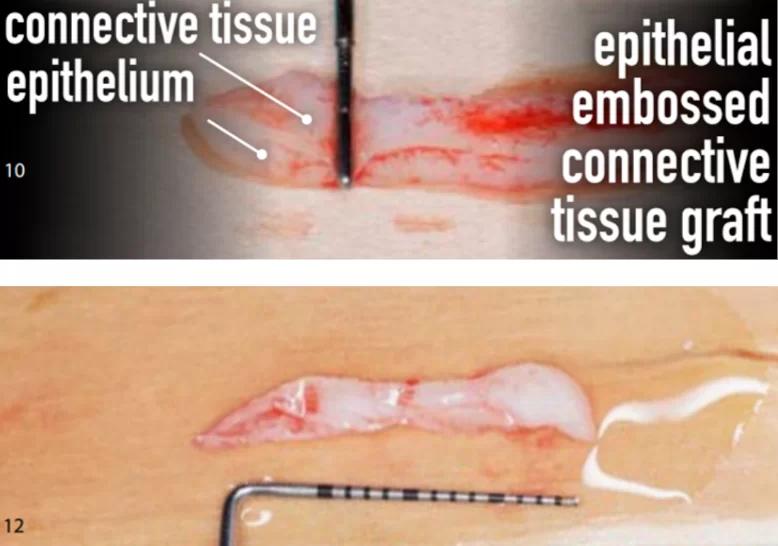
As for the graft, a significant amount of connective tissue graft is needed to correct generalized gingival recession and can only be taken from the mid-palate region – this is the area from the canine to the molars. Material from the cusp can also be taken, but the palate tissue has more fibroblasts, which has a positive effect on the speed of engraftment and restoration of the gingival level.
We did not discuss the details and nuances of techniques such as lateral flap displacement or coronal flap displacement because a separate article is needed to describe each technique and the peculiarities of suturing and graft harvesting. Here we have a general overview of the problem, outlining the key points of diagnosis and gingival level restoration.
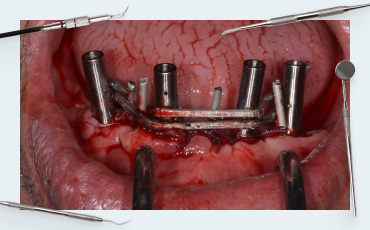
Also worth mentioning are very similar surgical techniques that aim to restore gingival volume when dental implants are placed. In the case of gingival recession, we are dealing with complete or partial loss of attached keratinized gingiva. A similar problem is seen in people who have lost teeth long ago, the soft tissue is thinning and the keratinized gum is almost completely degenerated, as seen in the photo below.
In such cases, implant placement is accompanied by guided bone regeneration surgery to restore the height and width of the alveolar ridge. After healing, a second soft tissue augmentation surgery is performed. Let’s analyze this case in more detail.
First, two 4 mm diameter implants were placed, as you can see from the photo below, the bone ridge does not cover the upper part of the implants, so bone augmentation was performed simultaneously with the placement of the implants.
Xenogenic bone graft (of animal origin) was used as bone filler which was fixed with a collagen membrane, see photo below.
After 6 months, the bone integration process was completed and the next surgery was performed to restore the volume of keratinized attached gingiva. As can be seen in the illustration below the patient was left with only a narrow strip of keratinized gingiva about 2 mm wide.
Surgery was performed to restore the attached keratinized gingiva using a connective tissue graft that was obtained from the patient’s palate.
But let’s get back to gum recession treatment and look at a successful example of comprehensive treatment, check out the before and after photos.

An example of a successful complex treatment. The dentition was straightened, the jaw began to move as it should anatomically, and the gingiva was surgically restored
The top photo shows that the patient had a malocclusion, which caused bone loss and significant gingival recession. The jaws could not move when chewing as it is inherent in the anatomy of the masticatory apparatus.
The inclination of the lateral and anterior teeth of the maxilla (indicated by the red lines) limited the movements of the mandible.
The bite was corrected, the gingival level was surgically restored and we had a beautiful result, see photo above. Three specialists were involved in the treatment of this patient:
- Periodontist
- Orthodontist
- Surgeon
All the above said again emphasizes the importance of a comprehensive approach to correcting gingival recession.
Post-treatment care and preventive care
Be sure to educate the patient. Some practitioners practice a kind of exam. They do not begin treatment until the patient demonstrates a full understanding of proper oral hygiene and shows that they have mastered all the necessary skills to use a toothbrush, floss, and irrigator. The patient bears much of the responsibility for the success of the treatment and whether there will be complications.
So, the patient should clearly understand that in the first 24 hours after surgery, they need to:
- Limit physical activity
- Avoid hot food and drinks
- Do not brush their teeth in the area of surgery
- Rinse the mouth with 0.02% chlorhexidine solution 2-3 times a day
- Apply cold compresses to the cheek in the area of surgery
After the surgery they should:
- Brush their teeth only with a very soft toothbrush and gentle toothpaste (no abrasives), and do not brush the surgery area for the first 3-4 days.
- Not use an oral irrigator as there is a chance of washing out the blood clot and causing complications.
- Rinse the mouth with 0.02% chlorhexidine solution 2-3 times a day.
- Show up for follow-up dental checkups in:
– 7-10 days after surgery
– 1 month after surgery
– 3 months after surgery
– 6 months after surgery
Prevention of gingival recession after successful healing:
- Maintain optimal oral hygiene. Do not traumatize the gums by brushing too hard or brushing too vigorously.
- Brush your teeth 2 times a day with fluoride toothpaste.
- Floss once a day, but floss gently to avoid gingival trauma and bleeding.
- Visit the dentist regularly (once every 6 months).
- Quit smoking.
- Reduce consumption of sugary foods.
Proper oral hygiene is crucial not only for preventing gingival recession but also for the success of dental implants. Learn more in our article on Soft Tissue Implant Integration.
Potential complications after surgical treatment of the gingiva:
- Bleeding. In case of minor bleeding, recommended the patient press a sterile gauze tampon to the wound for 10-15 minutes, alternating with cold compresses. If the bleeding does not stop, the patient must seek your help immediately.
- Swelling. On their own, the patient can relieve swelling with cold compresses for 10-15 minutes 3-4 times a day. Prescribe anti-inflammatory drugs (ibuprofen, paracetamol); just warn about the importance of not exceeding the dosage. If the swelling does not go away within 3-4 days, the patient should come to you for evaluation.
- Pain. NSAIDs can also help; if the pain is too severe and does not go away for more than 4-5 days after surgery, the patient should contact you.
- Infection. Some specialists prescribe antibiotics immediately and even give the patient an antibiotic a few hours before surgery. Inform the patient how to identify signs of infectious inflammation so that if they notice such signs, they will contact you immediately.
- Transplant rejection is the most difficult type of complication. Explain to the patient that if they notice any of the following symptoms, they should see a doctor immediately:
- Redness, swelling, pain, and/or bleeding in the graft area
- The appearance of purulent discharge
- Loosening or detachment of the graft
- Unpleasant breath smell
- Increased tooth sensitivity in the area of the graft.
- General malaise, increased body temperature.
In case of early intervention, results of surgery can still be salvaged, otherwise, there is a long-term treatment and reoperation to be done.
We hope this article was helpful to you. We look forward to bringing you more informative content in our upcoming posts.