Planning Implant-Supported Restorations: From Single Tooth to Full-Arch

In this article, we will discuss which restorations can restore chewing function completely and how many implants are needed for this. We will also cover how to distribute implants and why several bridges are often better than a full-arch restoration. In our previous article on errors and complications during implant-supported dental restorations, we examined the consequences of poor planning and lack of coordination between the surgeon and the prosthodontist. In this article, we will look at what should be taken into account for competent planning.
Stages of successful dental restoration
We will analyze the process from the initial clinical situation presented by the patient to the final result, which is the completed restoration.
- Treatment planning
- Diagnostics, including cone beam computed tomography and optical imaging.
- Developing a treatment plan: placement of implants, decision on the need for bone grafting, etc. Skipping this stage can lead to poor designs, where the prosthodontist and dental technician struggle to fit the prosthesis on chaotically placed implants.
- Preparation for dental restoration
- Extraction of hopeless teeth (if necessary).
- Bone grafting (if necessary).
- Placement of implants, followed by either a delayed protocol or immediate loading, depending on the chosen treatment plan.
- Carrying out restoration
- Physical or digital impressions.
- Designing and manufacturing the temporary or permanent prosthesis.
- Fitting and placing the prosthesis.
- Evaluating the finished result.
Total absence of teeth: recommendations on the number and distribution of implants, bridges and crowns
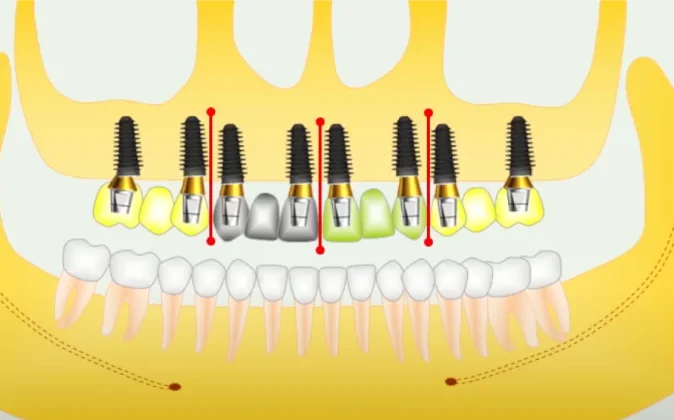
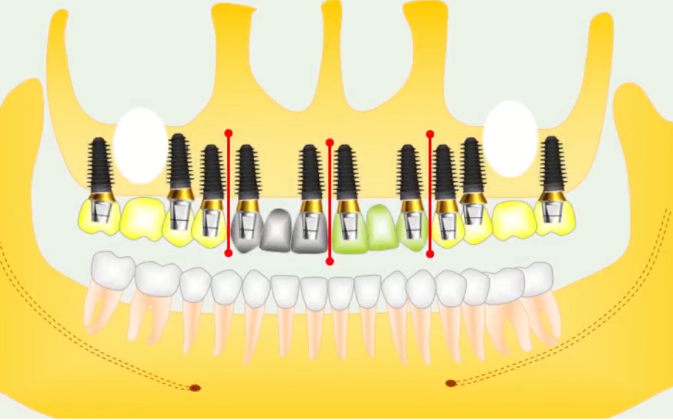
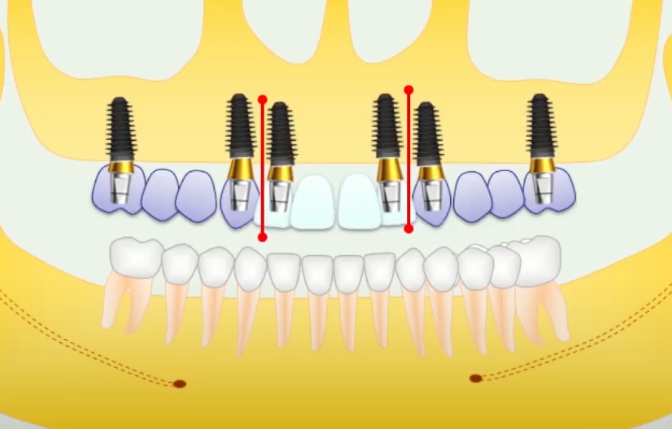
Let’s start with the scenario of total absence of teeth, as this experience can be easily extrapolated to the restoration of smaller or single defects. Below is a diagram of the optimal distribution of implants and dentures for the upper jaw. This regimen is rated green as the most balanced with minimal risk of complications.
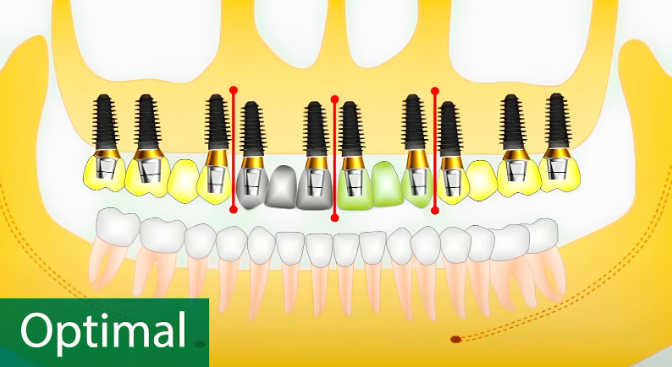
Scheme of complete restoration of the upper jaw: 10 implants; 14 teeth; 4 bridge structures. YouTube / Dr. Kamil Khabiev / Dental Guru Academy
Also note that it is recommended to carry out the restoration in the form of four independent bridges. The advantages of this scheme include:
-
-
- Optimal load distribution: There are no long levers that can dislodge the implants from the bone. The lateral and anterior sections are separated. Additionally, bridges are divided along the line of the central incisors, where the median suture (palatal suture) passes. Along this seam, micromovements of the palatine processes relative to each other are possible. If the prosthesis in this part is solid, it can cause discomfort for the patient and, in some cases, even breakage of the prosthesis along the palatal suture line. We will analyze one of these cases further in the text.
- Four individual bridges are much easier to place than a full-arch restoration. Often, a complete denture is placed with internal stresses or visible gaps where there should not be any. Generally, it is unrealistic to place a bridge on cement retention where there are more than three implants. Screw retention can help, but it does not solve all problems and sometimes creates new ones. In the previous article, we mentioned cases where screw shafts extend onto functional cusps. Even when screw-retained, not all dentures pass the Sheffield test, indicating that the restoration may not last long. While restorations according to the recommended 10 by 14 scheme can easily last 20-30 years, All-on-4 and All-on-6 restorations typically last 5-10 years. During this time, the volume of bone in the distal parts decreases, making it very difficult to create a full-fledged restoration. Voluminous and complex bone grafting operations may be necessary, and during this time, the patient will have to use a removable prosthesis.
- Even a mediocre prosthodontist can correctly perform and fit a high-quality restoration of four bridges, while a successful restoration of a full arch requires exceptional skill.
- Optimal implant spacing: The bone tissue receives adequate nutrition, minimizing the risk of critical bone loss around the implants. For example, in the lateral sections, implants are placed in the area of the 6th and 7th teeth because these are large teeth with enough space between the implants, and the load is greatest there. There is a gap in the area of the 5th teeth to provide enough space for bone tissue nutrition. Implants in the area of the 4th teeth serve as the extreme supports for lateral bridges. Thus, there is sufficient bone tissue, and the strength of the structure is optimal.
- Standard implants with a diameter of 4.0-4.5 mm can withstand any load with this design, while being thin enough to allow sufficient bone tissue between them. Moreover, these diameters are common and readily available.
- Maintainability: If a chip or crack occurs in one of the sections, it can be removed for repair or replacement without leaving the patient completely without teeth. In the side sections, the bridges can be removed without any visible impact, allowing the patient to chew on the other side. If something breaks in the area of the front teeth, a temporary bridge can be quickly made. Even if one or two implants are lost, new bridges can be made to maintain functionality while the new implants integrate.
- Excellent aesthetic result: There is no artificial gum, and the teeth look as natural as possible.
-
In a dialogue with the patient, we recommend offering this option first. Emphasize that only this option will restore the chewing function completely and last as long as possible. The pictures below show examples of restorations built on this principle.
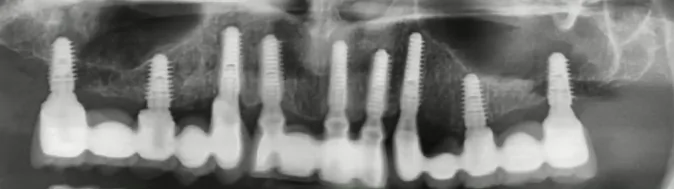
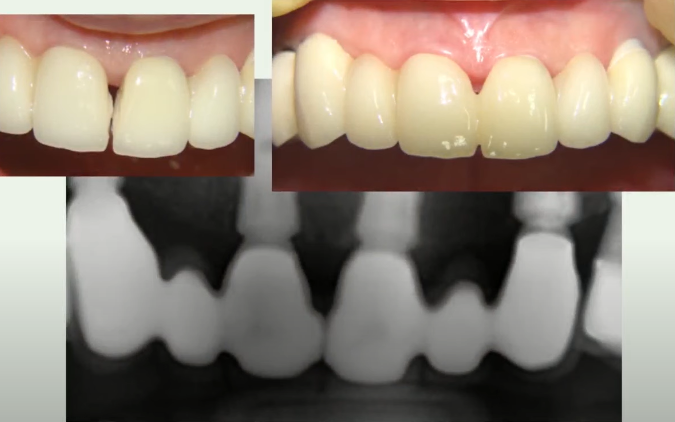
Examples of Restorations Using the Scheme of 10 Implants for 14 Teeth in the Upper Jaw and 8 Implants for 14 Teeth in the Lower Jaw. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
These and other patients continue to be monitored, and the restorations are in excellent condition. There are no problems along the gum line or with bone resorption. Both cases involve single-stage implantations with immediate loading. This is clearly visible by how well the axes of the implants align with the crowns. This result is easy to achieve if you follow the sockets of newly extracted teeth. The surgical template does not provide such accuracy.
However, among patients who received restorations using the popular All-on-4 protocol, there were more complaints of problems. Although everything is within normal limits, we do not advocate abandoning these methods of prosthetics. We encourage discussing all options with the patient, including the risks and benefits of each.
The recommended regimen is conditional and may vary depending on the clinical situation. The positions of certain implants can be shifted, for example, to bypass the maxillary sinuses. But the principle remains the same.
According to statistics, people lose their sixth teeth first. If such a tooth was lost a long time ago, placing an implant in this place becomes problematic. In such cases, the implants are shifted to the area of the 5th teeth. The illustration below shows an example where implants need to be placed to bypass the maxillary sinuses without performing a sinus lift.
Scheme of 10 Implants for 14 Teeth with Displacement from the Area of the 6th Teeth. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
Yes, with this scheme, the implant in the area of the fourth tooth is somewhat compromised because it is “sandwiched” between the canine and the fifth tooth. However, if sufficiently thin implants (⌀4.2) are used, the condition of maintaining a minimum of 1.5 mm of bone tissue between implants is met.
Complete restoration of the dentition can be achieved using 8 implants, but this is recommended only if the occlusion is favorable. This approach can save costs while providing the patient with the same 100% function as with 10 implants. However, this is considered a yellow version, unlike the previous green one.
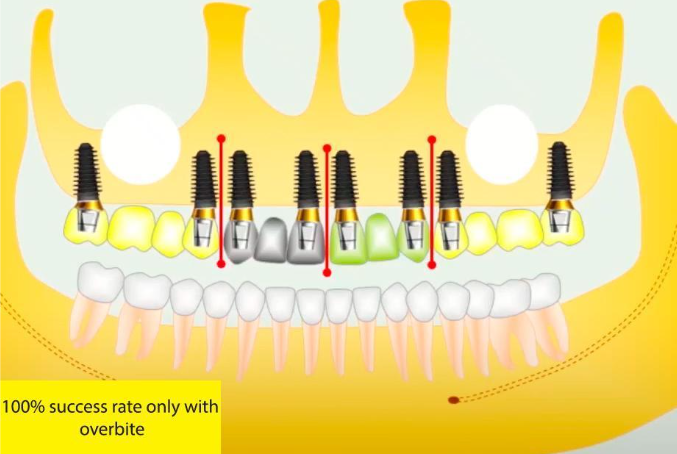
A scheme of 8 implants for 14 teeth in the upper jaw is recommended only for favorable occlusion. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
You can also reduce the size of the crowns in the molar area to decrease the load. Additionally, you can create a shortened dentition of 12 teeth on 8 implants, as shown in the following illustration.
This option is optimal when there are no antagonist teeth opposite the upper 7s. This restoration is also quite functional, as we typically consume processed and relatively soft food. Moreover, a shortened denture will be easier to care for and clean.
Why is it Better to Split the Front Axle?
In all diagrams, we see that the front axles are divided along the central incisors. Although many prosthodontists often try and even insist on making a solid bridge, we do not recommend this approach. Let’s explore why using a specific example.
The distribution of implants is close to the recommended scheme. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
Please note that all but one implant are quite narrow. A wide implant was placed in the area of the 17th tooth due to the specifics of simultaneous implantation. It would not have been possible to place a narrow implant with an acceptable torque in this location.
Restoration with a bridge connected in the area of the central incisors. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
The division into separate bridges made it possible to place zirconia abutments in the area of the front teeth, achieving excellent aesthetics. In the lateral sections, more affordable titanium abutments, which are not prone to cracks, were placed. As we know, due to the different properties of elasticity and plasticity, titanium and zirconia abutments cannot be combined into one bridge.
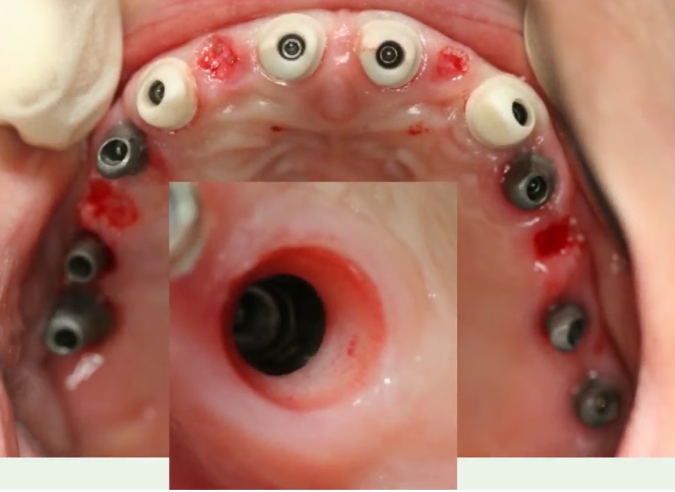
Zirconia abutments and perfectly formed gingival cuff in the area of the anterior teeth. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
However, this case is interesting because the dental technician made not four bridges as ordered, but three. He combined the front section into a single bridge from canine to canine. At first glance, the result appeared to be excellent.
The prosthodontist did not return the work, as the bridge fit well, and the decision was made to place this prosthesis. Moreover, this was an immediate implantation, so there was no time to wait for a new prosthesis. Everything looked good initially, but after about 8 months, the patient returned with a crack in the restoration right along the line between the central incisors.
A crack in the denture along the incisor line and temporary correction of the defect with a composite. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
IIf the prosthesis had been made of PFM, the cracks would not have occurred, but the patient would have experienced unpleasant sensations, and the bone around the implants at the position of the central incisors would likely have begun to resorb. The beginning of this process can already be seen by the loss of the gingival papilla between the central incisors.
The reason for this situation was the micromobility of the patient’s palatine processes. In some people, the central suture fuses at the level of the bone tissue, resulting in almost no mobility. However, in this patient, the fusion was incomplete, and the fibrous connection predominated. Due to the mobility of the palatine processes, the zirconium prosthesis fractured.
The symptoms described by the patient are interesting. When chewing, it felt as if something had gotten between the teeth. These sensations passed, so the patient ignored them until one day there was a click with a flash of pain and a gap appeared.
If the bridge had been divided, such problems would not have arisen, even theoretically.
What to Do if It Is Not Possible to Place Implants in the Area of the Central Incisors
Such situations occur when there is a significant deficiency of bone tissue in this area. In these cases, we recommend a scheme with three bridges, as shown in the illustration below. It is still possible to take a risk with the union of the central incisors, but the bridge should not be purely zirconia.
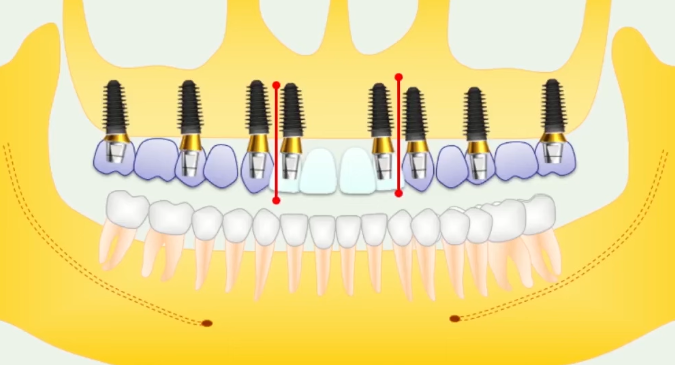
Scheme of restoration of 14 teeth on 8 implants when it is impossible to place implants in the area of the central incisors. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
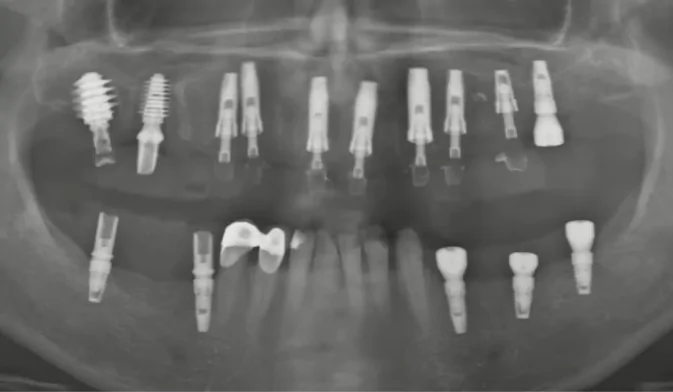
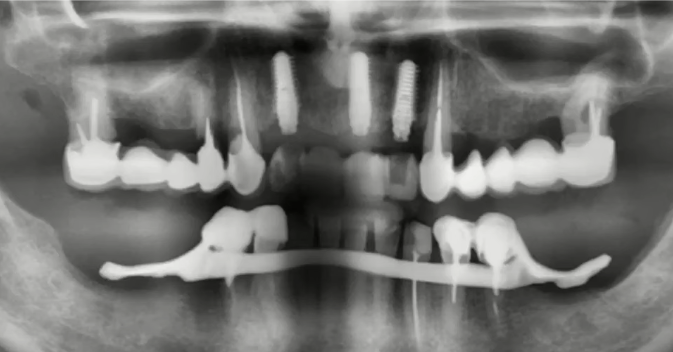
Let’s look at a specific example. The orthopantomogram below shows the clinical picture with which the patient presented.
Important advice for your doctor: always think ahead. The patient complained only of mobility and pain in the anterior teeth of the upper jaw.
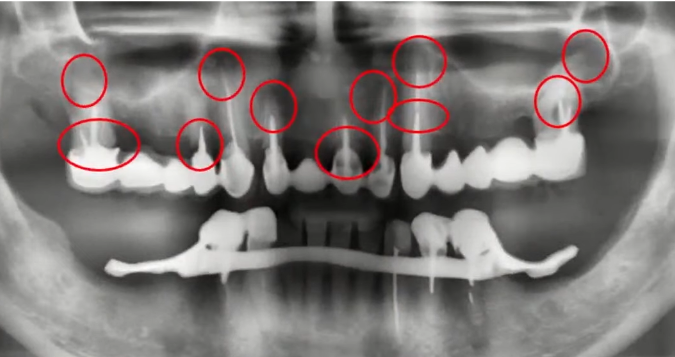
The patient’s complaints: the four front teeth of the upper jaw are mobile and painful. All problem areas are marked in red, even those that are not yet causing discomfort. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
However, the picture shows that the bridges in the lateral parts of the jaw rest on two pulpless stumps, indicating that problems will likely arise in the near future.
Even without CT images, it is clear that the 14th tooth has decayed, and there are cysts and perforations in the area of the 16th and 17th teeth. Additionally, there is a cystic granuloma at the end of the 13th tooth. The situation on the other side is slightly better.
There is no point in “saving” and re-treating such teeth, as it would cost more than placing an implant. The optimal treatment plan is the complete removal of the remaining teeth and restoration of the dentition supported by implants.
Many dentists might suggest the All-on-4 scheme because it is simple, fast, and inexpensive. However, this would be a mistake, as it would not be possible to obtain a stable structure with four bone implants of such quality.
This patient was offered a treatment plan as shown in the diagram above. While the solution is not ideal, it is the best option based on the condition of the patient’s bone tissue.
The patient was also offered a step-by-step and time-extended treatment option. First, place the anterior bridge on two implants. Then, when the remaining teeth that hold the side bridges are gone, place three implants on each side and create two more bridges.
This option addresses the patient’s current problem, as only the front teeth are causing pain. The patient reviewed the treatment plan and agreed to the step-by-step approach. The first stage involves the placement of implants with the simultaneous placement of a prosthesis.
During the operation, it was decided to place three implants because it was uncertain whether two implants would achieve sufficient primary stability. The defects in this area were extensive, and after the teeth were removed and the sockets were cleaned, there was even less bone tissue left for reliable retention of the implants.
Three implants placed at the first stage of treatment. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
If we were talking about a delayed protocol, two implants would be sufficient. They would integrate reliably and hold the bridge without any problems. In this case, however, the situation is further complicated by the large length of the future abutments and crowns, which act as a lever.
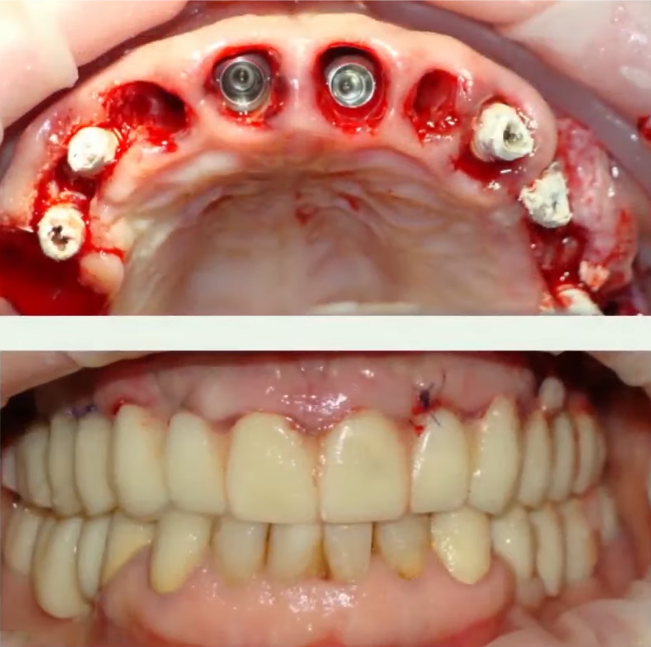
A temporary bridge was successfully placed on these three implants, and after three months, a permanent prosthesis was fabricated and successfully placed. See the picture below.
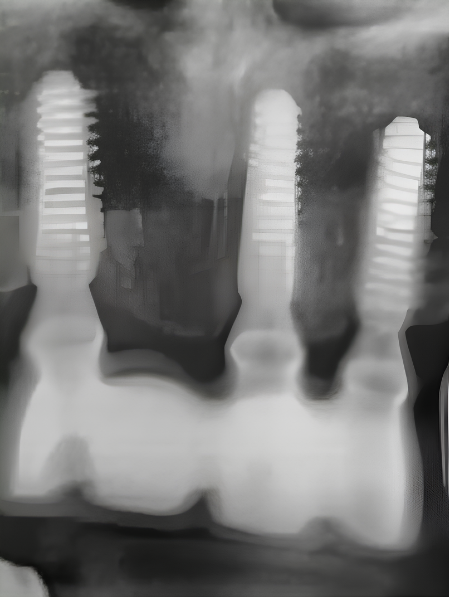
Maxillary incisor prosthesis supported by three implants. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
Although this is not exactly the concept indicated in the diagram, we are interested in the next stages of treatment. The patient’s bridge prosthesis on the right fell out after 8 months, and the patient finally understood the concept of the treatment. It is noteworthy that the patient returned to the same clinic where he received a detailed treatment plan, as trust had already been established. He saw and understood the complete treatment plan and was pleased with the previously completed restoration.
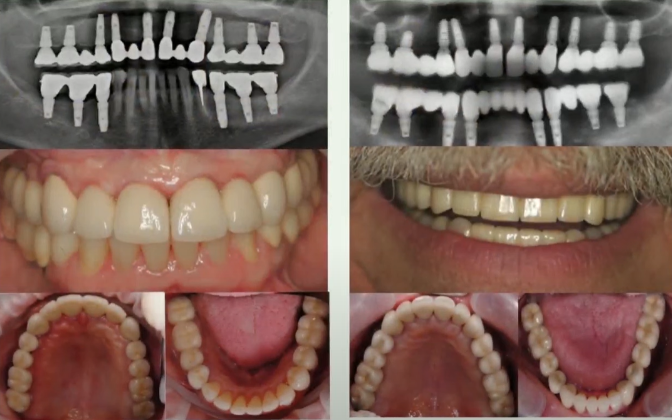
At the second stage of treatment, six more implants were placed, and a new temporary bridge was made. The new bridge restores part of the dentition up to the 5th teeth.
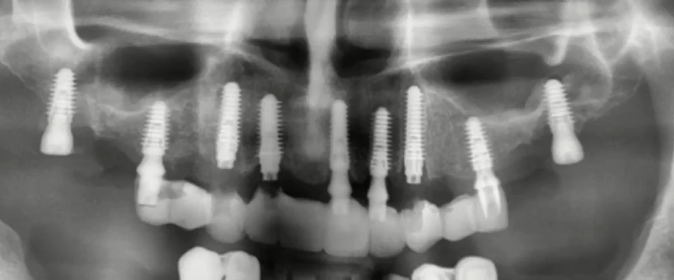
Six more implants and a temporary prosthesis were placed, supported by already integrated implants and two newly placed ones. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
The new bridge rests on fully integrated implants in the anterior section and on new implants placed in the area of the 5th teeth. The condition of the bone tissue in the area of the 7th teeth was so poor that it was decided not to load the implants and allow them to fully integrate. Therefore, gum formers were placed in them, and the remaining implants were closed with plugs.
The patient used the truncated prosthesis for four months, after which three permanent bridges were placed. Additionally, a previously made permanent bridge for four teeth was placed in the anterior section.
It is also interesting that a year later, the same patient returned for restoration of the lower jaw, where he had a removable (clasp) denture. He came on his own without waiting for new difficulties, which once again emphasizes the importance of trust between doctor and patient. Although at the first appointment he categorically refused the treatment plan for the lower jaw, saying, “I’ve been wearing a denture for 20 years, and I’m happy with everything.”
Not all doctors take the patient’s side and defend their interests, and this is especially important for specialists in private practice. But back to our case, this is what the picture looks like after placing bridges on the lower jaw.

The third stage of treatment is restoration of the dentition in the lateral parts of the lower jaw. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
Chewing function has been completely restored, and the aesthetic result is also very good. The patient appreciated all the advantages of implant-supported fixed dentures and was very satisfied.
How Effective are Restorations Supported by Six Implants?
We are not talking about the All-on-6 restoration scheme, which uses a solid arched prosthesis with screw retention, but about a scheme of three bridges. retention can be either screw or cement. The diagram is in the illustration below.
Scheme of 12 teeth on 6 implants – 3 bridge structures. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
This option can hardly be called optimal; moreover, full-arch restoration with an ideal passive fit is better than the proposed scheme. However, creating such a restoration is extremely difficult, even with screw retention, and such a prosthesis will be very expensive.
Therefore, the proposed option is still quite workable and even has several advantages compared to the average (non-ideal) All-on-6 scheme, namely:
-
-
- Better load distribution
- Easier to achieve a good passive fit with three bridges than with one large prosthesis
- If cement retention is chosen, there are no exits of the screw shafts to the functional cusps
- Better maintainability and durability of the distributed system
- Moderate selling price
-
IMPORTANT WARNING! Do not make a restoration supported by 6 implants from two bridges separated along the line of the anterior incisors.
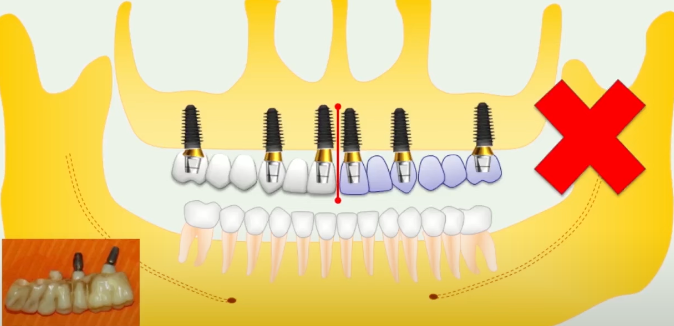
It is strictly not recommended to do restorations with the division of bridges according to this scheme. YouTube/Dr. Kamil Khabiev / Dental Guru Academy
We have already described this case in an article about errors and complications during restoration, but it never hurts to warn again. The problem is that the specialization and load on the teeth in the anterior and posterior sections are very different. When chewing, the bridge acts as a lever and can dislodge the implant in the area of the front incisor. In this case, several unfavorable factors converged:
-
-
- The bridge combined zirconia and titanium abutments, which should not be done
- The prosthesis was made of zirconium dioxide, a material that is durable but fragile
- The patient suffered from bruxism
-
IMPORTANT! When combining the lateral sections with the anterior sections, the abutments and implants in the anterior section are ALWAYS the first to suffer.
How to Talk to a Patient During the Planning Stage
Always remember that you need to communicate with the patient from two perspectives: logic and emotions.
For example, a person can get excited with anticipation of the result; they had bad teeth but now expect a Hollywood smile. The patient agrees to everything and is ready to pay. However, when they experience swelling, pain, and other issues, their mood drops. The patient begins to complain: why is it taking so long, it’s inconvenient, when will that Hollywood smile appear? And when they find out that the irrigator is now a permanent, daily necessity, conflicts and discontent may arise.
If you conduct a dialogue only from the logical perspective, the patient will start questioning the cost, bargaining, and asking for cheaper options, which they may later regret.
Therefore, it is important that the patient understands that the proposed option:
-
-
- Is justified and will restore the dentition in the best possible way
- Explains why implants need to be placed in specific locations and in specific numbers
- Clarifies the risks and disadvantages of cheaper solutions like All-on-4
-
Even if the patient then goes to another clinic where they are told, “Why so many implants?” and offered a simpler, quicker, and cheaper solution, their inner critic will already be activated. They will understand what they will lose in the pursuit of cheapness, knowing about the incomplete restoration of chewing function, the risk of cracks and breakage of the prosthesis, etc.
A patient who understands all the disadvantages and advantages is more likely to make the right decision. Often, people find extra money because they understand that it is better to pay now and do it once and efficiently than to fix problems later at exorbitant prices.
We believe that applying the All-on-4 protocol when everything can be done with 10 or 8 implants is harmful to the patient. These protocols are good when it is not possible to make a full restoration, or insurance only covers this option. In general, there are direct indications for these protocols; in all other cases, when it is possible to make a complete restoration on a larger number of implants, this is what should be done.
A good and honest approach towards the patient is to give them all the options, from the minimum with a removable denture fixed to the gum, to the maximum with support on 10 implants. Most likely, the patient will choose something in between, but this will already be their area of responsibility. They had complete information, and only the patient is responsible for the choice and its consequences. Trust is very valuable—it is a direct contribution to reputation.
That’s all for now. Until the next publications.