What is better, a tooth or an implant? Part 1

Before we start choosing and discussing the features of implants, let's address the fundamental question of what the patient loses after a tooth extraction and whether there are advantages to restorations on implants over living teeth. Of course, when teeth are lost, there is no alternative to dental implant restoration. The goal of this article is to show how important it is to keep a tooth alive, even if the treatment is more difficult than an extraction and placement of an implant.
Not only patients, but also some dentists do not have a clear answer to this question. After all, a quality restoration looks great, is quite functional, the patient is satisfied and it seems that the restoration on the implant is not inferior to live teeth.
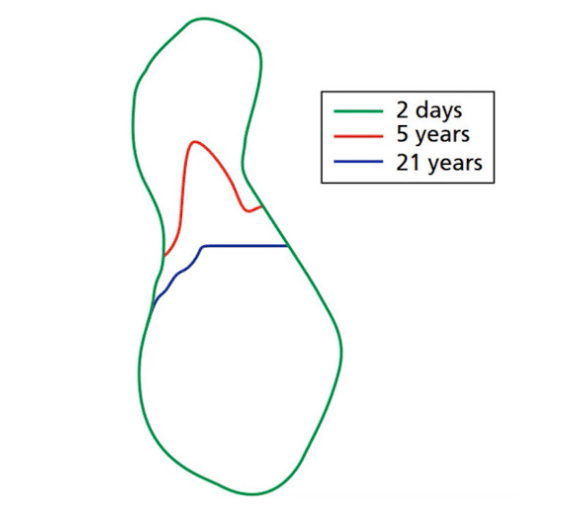
In fact, there’s an unspoken competition among dentists when they send their colleagues a photo and ask them to identify which teeth are natural and which are restorations on implants. Here’s an example of a very good job.

It is impossible to detect which tooth is the restoration before the radiographs have been taken. However, if it were that simple, dentists wouldn’t try to treat and preserve living teeth.
No matter how good an implant restoration looks, it is still a prosthetic tooth root. If you start comparing a living tooth to an implant, you will find that several important functions are lost. Let’s look into this in more detail.
Periodontal ligament after tooth extraction
Root cement, vascular network and innervation in the difference between the tooth and the implant
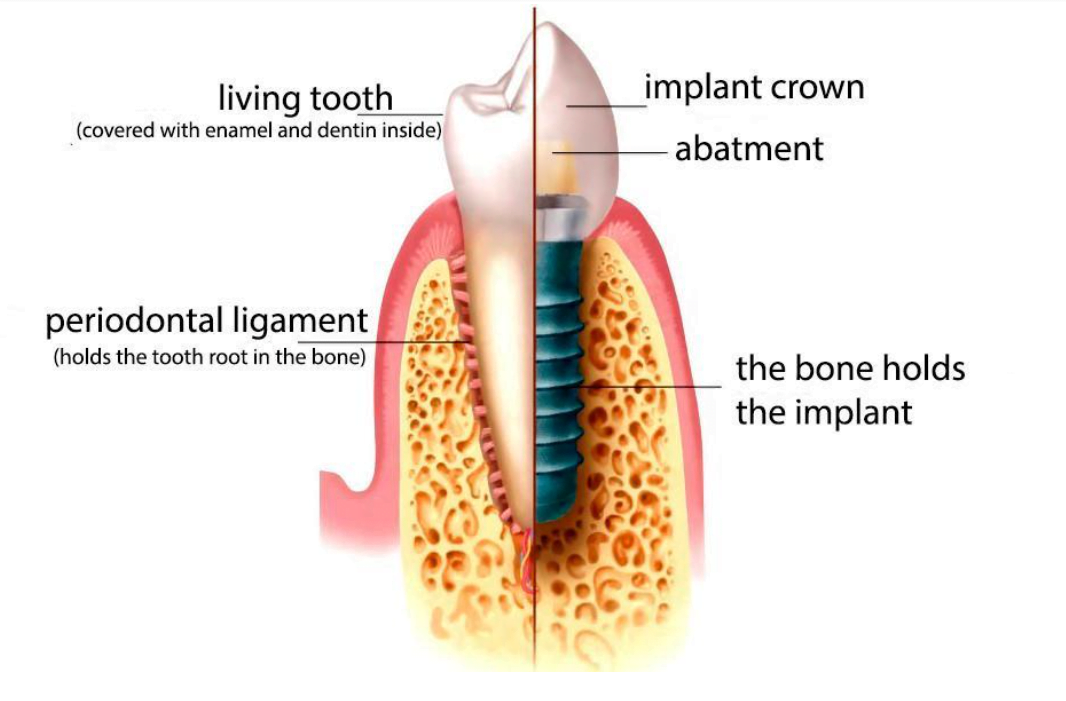
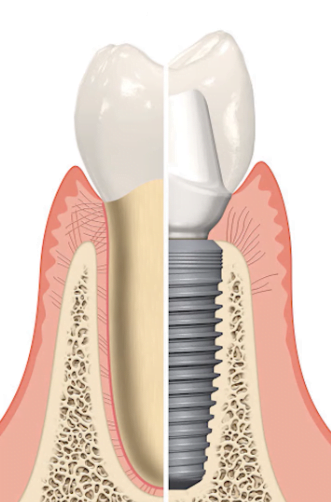
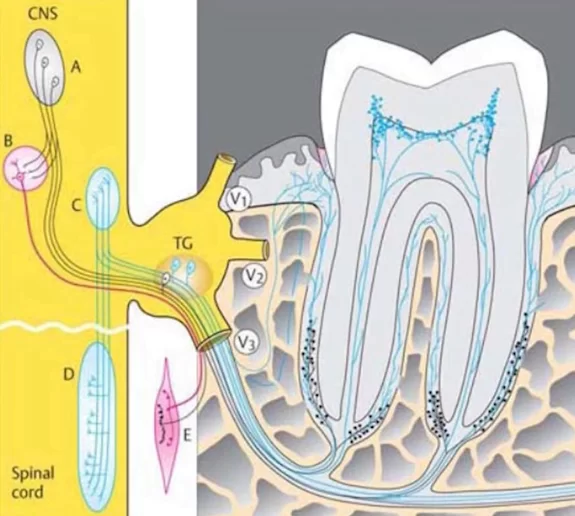
After a tooth extraction and implant placement, the periodontal ligament that separates the tooth root from the bone is lost, see illustration below.
It is a colossal complex of vessels, ligaments and nerves. Here are the most important functions of the periodontium:
- Cushioning: When chewing, the teeth come into contact with each other and experience both axial and lateral loads. The elastic fibers of the periodontium allow for compensation of these loads. A living tooth is physiologically mobile and can recede slightly into the jaw and move sideways under lateral loading. The tooth will return to its original position after the pressure has been removed. Implant-supported crowns lose this ability. This difference is not observable in daily life, but the normal physiological mobility helps to preserve the enamel and the integrity of the teeth during stressful situations. An immobile implant can cause a crack in an opposing or neighboring tooth.
- The periodontium has an excellent blood supply. Bleeding during tooth extraction occurs mainly through the periodontal vessels. After the loss of this vasculature, the nutrition of the implant-adjacent tissue is impaired. This leaves only the capillaries in the bone itself and partial nutrition from the periosteum. This also partially impairs the nutrition of the soft tissue in the coronal area of the periodontium where they pass into the gingival cuff, which will be the next point.
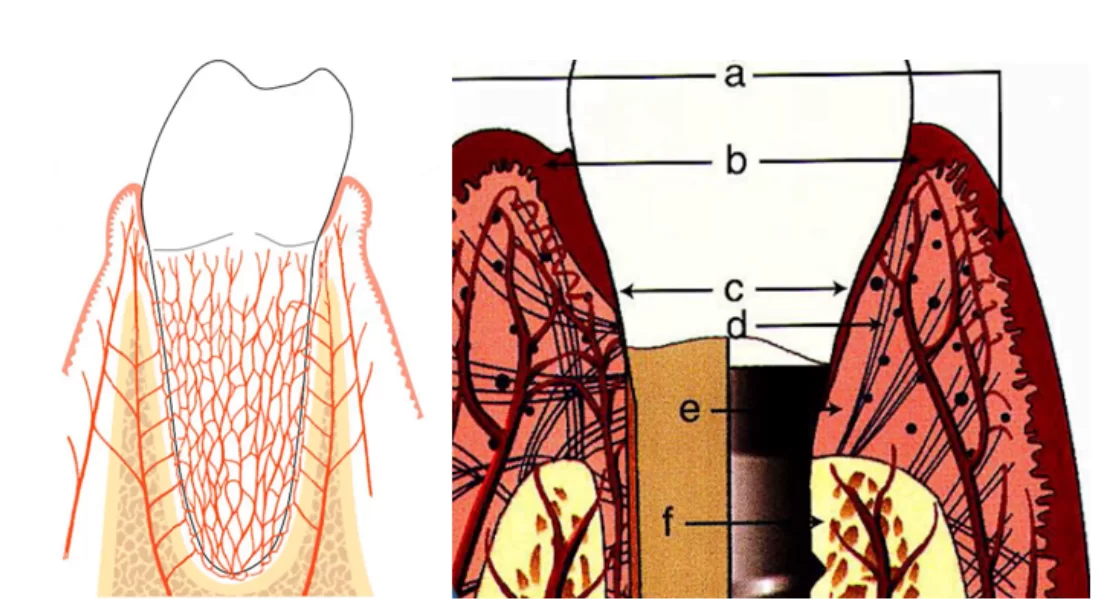
- Protection and separation of the non-sterile environment of the oral cavity from the sterile environment under the soft tissues. We are talking about the biological width or as it is also called – the gingival cuff. It is a complex of collagen fibers and epithelium, which form a tight cuff around the upper part of the root. In addition to the physical separation, the periodontal complex contains humoral and cellular immunity factors.
After implant placement, this soft tissue complex is restored, but it is only partially restored. The immune component is almost completely lost. In most cases, partial restoration of the gingival cuff is enough to avoid problems, but it is not uncommon to have problems with non-sterile fluids seeping under the implant neck. This causes chronic inflammation and can even lead to peri-implantitis. This is why oral hygiene with dental implants is much more difficult than conventional hygiene procedures.Using a cantilever when it is impossible to add another dental implant - The tactile function is also provided by the periodontium. The sensitivity threshold of healthy teeth is 20 microns – a person can feel the presence of a foreign object of this insignificant magnitude. Prosthetic teeth also develop tactile sensitivity over time, but there the sensitivity limit is 100-150 microns, which is at least five times lower.
- The periodontal complex is also involved in dental-alveolar advancement. As the teeth wear out over the course of their lives, they gradually extend out of the alveolus. In addition to upward tooth advancement, living teeth are involved in what is known as mesial drift, which is the gradual movement of the dental socket from the distal jaw to the front teeth. Dental implants do not drift, which can lead to gaps between the natural tooth and restoration after a few years, when the natural tooth “floats away” and the implant remains in place. For the same reason, dental restorations with dental implants are not recommended for very young people, especially in the aesthetic zone. An example is shown in the pictures below.
The radiograph clearly shows that the root of the living tooth has moved forward, but the crown with the implant has remained in place, resulting in an aesthetic defect.
light of the above, it is clear that the dental implant is not a full-fledged copy of a living tooth root. That is why dentists try to save teeth even with minor cracks, treat and fill root canals when periodontitis has begun, etc.
Changes in the structure of the mucous membrane after tooth extraction
Let’s first look at the varieties and functions of oral mucous membranes. There are three types of mucous membranes, see the table below.
|
Function |
% of the surface area |
Notes |
| Chewing mucosa |
25% |
Keratinized fixed gingiva around the teeth |
| Lining the mucosa |
60% |
Thin and flexible mucosa that covers the inner surfaces of the cheeks and jaws below the level of keratinized gums |
| Specialized mucosa |
15% |
The mucosa with glands is the surface of the tongue, salivary gland outlets, etc. |
Let’s break down the chewing mucosa in more detail.
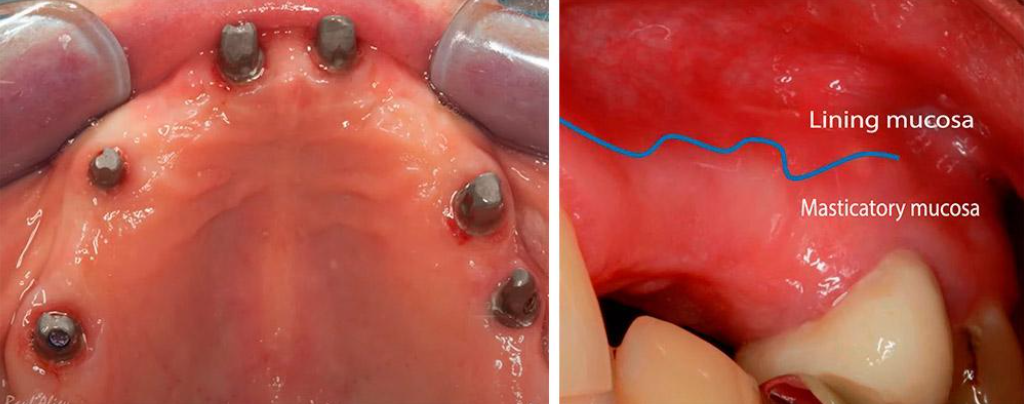
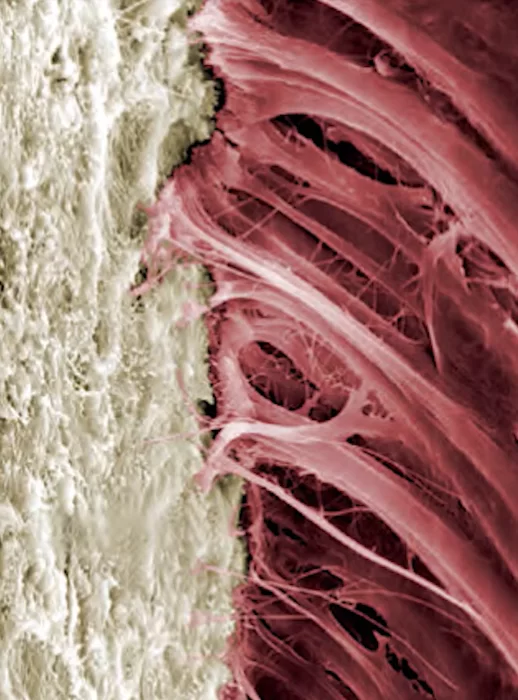
The keratinized gum, aka chewing mucosa, is a dense membrane fixed to the bone that can withstand the friction of food clumps and surrounds the teeth in a tight ring. Also, almost the entire upper palate is covered by this type of gum.
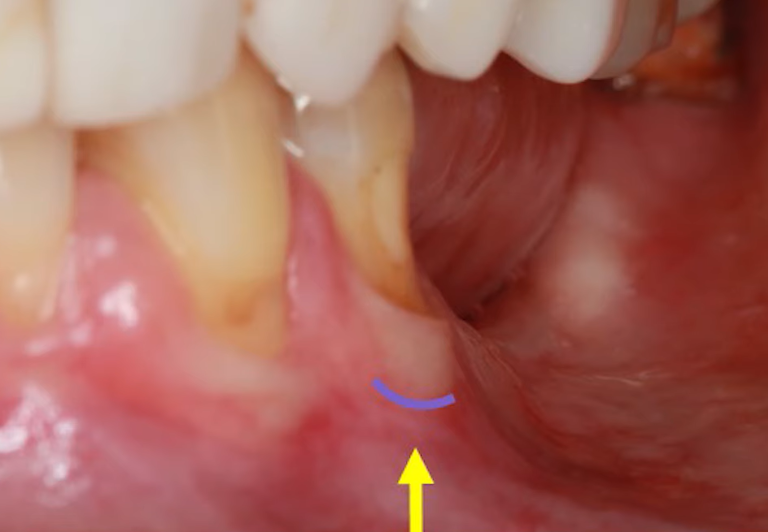
We are interested in the chewing mucosa that surrounds the teeth. Normally, there is always some amount of keratinized gum around the tooth. If the patient has a thick phenotype, the chewing mucosa is thick and massive. If the phenotype is thin, the band of attached keratinized gingiva may only be a couple of millimeters. This type of mucosa is always there when there is a living tooth root. Sometimes it is very thin and if there is advanced periodontal disease may be unattached as in the picture below, but it is always there and serves a critical function.
The dense, attached gingiva is an important part of the barrier that protects the internal structures of the tooth root from the non-sterile environment of the oral cavity. The body repairs the keratinized layer after damage. There have been experiments on dogs in which a mucosal flap was cut off and unfolded and sewn so that there was soft mucosa around the tooth. After a few weeks it was transformed into a dense attached gum with high keratinization.
However, after the tooth is removed, there is a gradual loss of the chewing mucosa. It is replaced by normal soft mucosa.
This is an irreversible loss because little or no new keratinized gum forms around the implant. If the tooth was lost several years ago, the dentist has to deal with a significant deficit of keratinized gum. This can lead to chronic inflammation of the soft tissue around the implant neck and even peri-implantitis. Therefore, if the tooth is definitely to be extracted, it is better to place the implant immediately or in the first weeks or months after the tooth extraction.
What happens to the bone structures of a tooth socket after extraction and placement of an implant?
Another important component of a living tooth that is irrevocably lost is the cementum of the tooth root. It is to the tooth root cement that the collagen fibers that make up the periodontal tissue complex are attached. In addition, it is a living bone tissue, which actively participates in the regeneration processes of bone and soft tissue. The titanium implant does not have this ability and a full-fledged connection of the collagen fibers, as in the picture below, to the implant surface is not possible. Because of this, the soft tissue complex around the implant cannot form the same quality connection. As a consequence, the gingival cuff around the implant is not as good as around a live tooth.
To improve the situation, the surface of the latest generations of dental implants has been made rough so that collagen fibers can more easily attach to them.
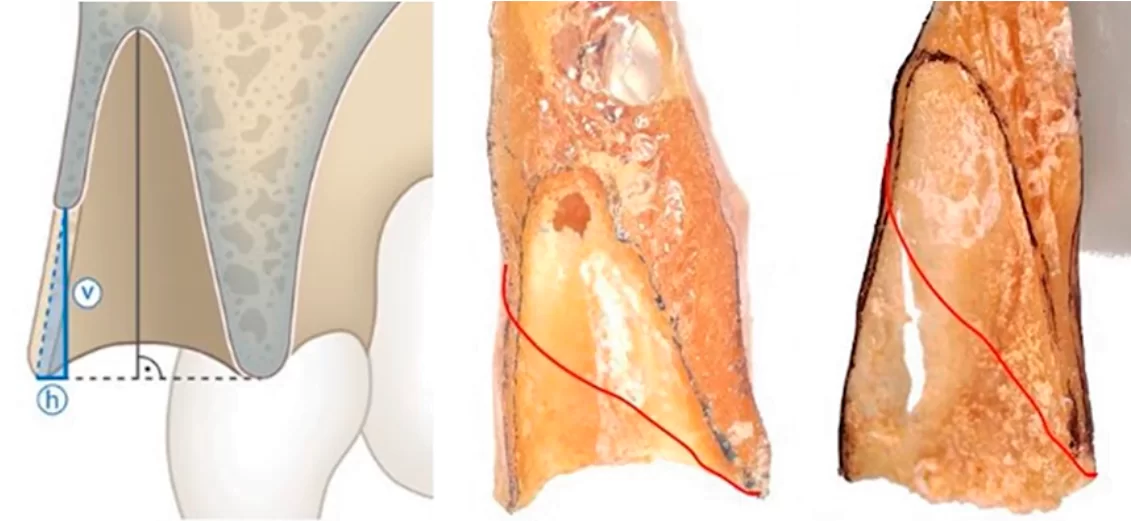
Another irreplaceable loss is the bandle bone. This is the dense lamina that lines the inside of the hole where the root of the tooth was. After the tooth is extracted, it is inevitably resorbed and replaced by cancellous bone. More precisely, the hole is filled with cancellous bone in the case of premolars and molars. Again, this is not critical, but the width and height of the alveolar ridge is reduced and the dentist could be faced with a lack of bone for the implant.
The situation is much more difficult in the anterior teeth area. The bandle bone is often the only bone plate that holds the root of the tooth on the vestibular side. After the resorption of this bone plate a very narrow and thin alveolar ridge remains.
If the implant is delayed, the dentist is faced with a bone deficit. This can be overcome by alveolar ridge augmentation surgery, but it is not an easy operation with a high risk of complications. That is why immediate implants are preferred in the anterior teeth area. The dental implant is then placed in the existing extraction site, and the bone is fused around the titanium implant with minimal bone loss, although there is almost always a small circular resorption after the implant is placed. However, the loss does not exceed 1-2 mm, and it is much less compared to the loss of ridge width and height in the case of delayed implantation.
Bone of the jaw – its features and behavior after tooth extraction
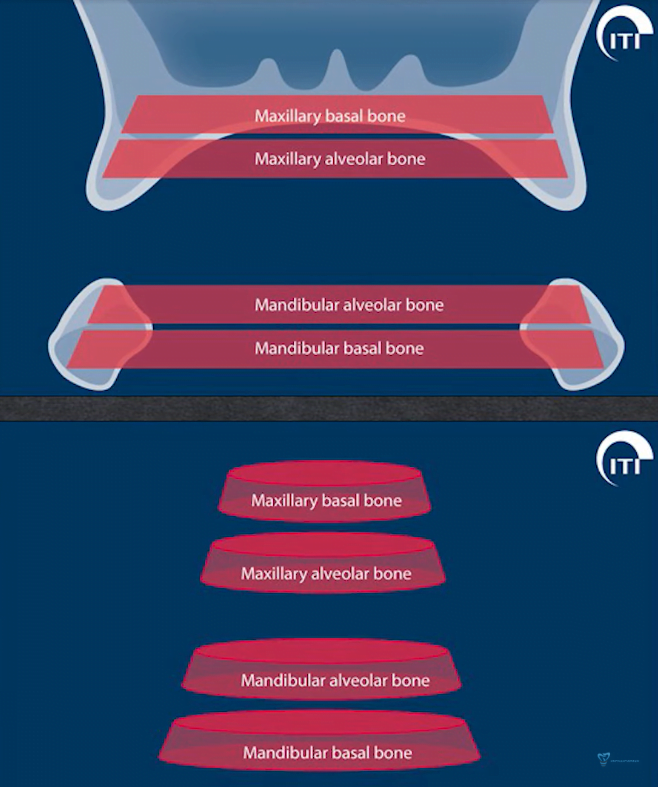
Let’s take a closer look at the bone structures of the jaws. The bone of the jaw consists of two areas:
- Basal bone – refers to the skull bone and remains unchanged (or almost unchanged) after removal of a tooth.
- The alveolar part (alveolar process in the case of the upper jaw). This part is subject to resorption. The body begins the process of transformation and dissolution of this part of the bone after the removal of teeth.
After all, this bone has no independent purpose, and it is the teeth that develop and maintain it. And those loads that are transmitted through the roots and the periodontal layer. If enough time passes after a tooth is extracted, the alveolar part of the bone disappears almost completely.
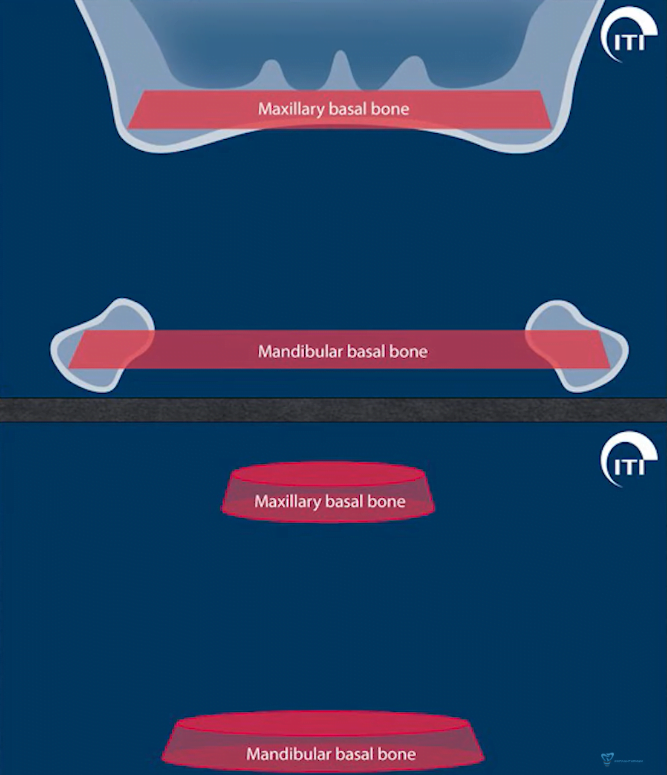
Bone is an invaluable human resource. You have to remember that and try to inform the patient about all the consequences. After all, if he or she decides to do a restoration in five years, it will be incredibly difficult to do so. Especially if the patient is elderly, because the older the patient, the more active the resorption and loss of bone and connective tissue. The risk group also includes patients with a thin phenotype, in which the resorption of the alveolar part of the bone tissue is faster. The figure below shows the process of bone loss at different times after a tooth extraction.
As you can see after five years there is very little alveolar ridge left, but it is still possible to perform bone augmentation surgery and place an implant. After 21 years, the alveolar ridge is completely resorbed, sinking to the level of the basal bone.
So, let’s summarize the loss of a tooth extraction:
- The periodontium, and with it the cushioning properties and the ability to participate in dental-alveolar advancement and mesial drift.
- The bandle bone, and with it a significant portion of the bone tissue suitable for implant placement.
- The inevitable process of alveolar bone resorption begins. Of course, the height and width of the alveolar ridge is not lost as quickly as in the case of the bandle bone. Whereas there it counts in weeks, here it counts in years.
- The way in which the soft tissue of the gingival cuff (biological width) is nourished deteriorates. With it the ability to resist infections and suppress inflammatory processes in the implant area decreases.
- Keratinized gingiva. You only have to deal with the amount of dense gum tissue that the patient has at the time of implant placement.
- Tactile sensitivity is impaired, which causes some discomfort to the patient. Although there is evidence that over time, osteoperception develops, that is, sensitivity through the bone. If a person is able to feel a foreign object of thickness from 20 microns through the teeth, through osteoperception one can feel objects of thickness from 100-150 microns.
Therefore, it is important to make every effort to keep the tooth alive. When this is not possible, an implant should be placed as soon as possible. In addition, it is necessary to minimize all the negative consequences associated with replacing a living tooth with a dental implant.
Many of the problems addressed in this article are described in detail in separate publications on our website. Articles not only contain in-depth analysis of bone and soft tissue processes, but also provide recommendations on how to improve the prognosis for successful implantation and engraftment of a dental implant.
We hope you have found this and the other articles on our blog useful. Until future publications!
-
Hot
-
Hot